Delirium, recognized as a crucial prognostic factor in the cardiac intensive care unit (CICU), has evolved in response to the changing demographics among critically ill cardiac patients. This study aimed to create a predictive model for delirium for patients in the CICU.
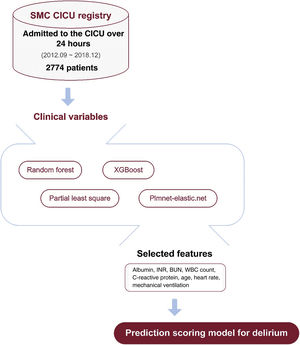
MethodsThis study included consecutive patients admitted to the CICU of the Samsung Medical Center. To assess the candidate variables for the model: we applied the following machine learning methods: random forest, extreme gradient boosting, partial least squares, and Plmnet-elastic.net. After selecting relevant variables, we performed a logistic regression analysis to derive the model formula. Internal validation was conducted using 100-repeated hold-out validation.
ResultsWe analyzed 2774 patients, 677 (24.4%) of whom developed delirium in the CICU. Machine learning-based models showed good predictive performance. Clinically significant and frequently important predictors were selected to construct a delirium prediction scoring model for CICU patients. The model included albumin level, international normalized ratio, blood urea nitrogen, white blood cell count, C-reactive protein level, age, heart rate, and mechanical ventilation. The model had an area under the receiver operating characteristics curve (AUROC) of 0.861 (95%CI, 0.843-0.879). Similar results were obtained in internal validation with 100-repeated cross-validation (AUROC, 0.854; 95%CI, 0.826-0.883).
ConclusionsUsing variables frequently ranked as highly important in four machine learning methods, we created a novel delirium prediction model. This model could serve as a useful and simple tool for risk stratification for the occurrence of delirium at the patient's bedside in the CICU.
Keywords
The role of cardiac intensive care units (CICUs) has evolved due to the changing demographics of critically ill cardiac patients who currently have greater noncardiovascular comorbidities and significantly increased complexity.1 With these changes, CICU patients are also susceptible to intensive care unit (ICU) -associated complications, which may be linked to their hemodynamic or respiratory instability and the use of organ support devices to manage their critically ill condition, similar to other types of ICUs.2,3 Consequently, intensivists need to comprehend general intensive care unit management and apply best-practice principles. However, limited guidance is available to support the management of CICU patients that takes into account the characteristics of critical cardiac conditions.4
Delirium is an acute brain dysfunction characterized by disturbances in awareness, attention, and cognition, with a fluctuating course. Delirium is a significant marker of poor outcomes in critically ill patients, and is associated with increased morbidity and mortality, exacerbation of cognitive impairment, deterioration of functional abilities after discharge, and elevated medical costs.5 Given the rising incidence of delirium in aging patients with complex comorbidities admitted to the CICU, early recognition and proper management of delirium may enhance clinical outcomes. Previous studies have reported that delirium can affect not only patients after cardiac surgery or other procedures but also those with heart failure.6–8 Despite the increased importance of delirium in critically ill cardiac patients, most studies on delirium in CICU patients are limited to specific procedures or a small number of patients.9–11 Furthermore, the clinical factors associated with delirium in CICU patients have not been fully elucidated.
Therefore, this study aimed to investigate the clinical factors associated with delirium in the CICU using machine learning methods and to develop a delirium prediction scoring model specific to patients admitted to the CICU.
MethodsStudy design and populationThis study used data from a retrospective cohort of the CICU of the Samsung Medical Center, an ongoing registry to evaluate the clinical characteristics, management, and outcomes of critically ill cardiac patients. All consecutive patients admitted to the CICU between September 1, 2012, and December 31, 2018, were included in the study. Patients were included if they were aged 18 years or older and excluded if they were admitted for less than 24hours or if data on delirium were unavailable. The study was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2020-10-102), and the requirement for informed consent was waived due to the observational nature of the study.
Standard care in the cardiac ICUThe CICU is a 12-bed ICU with a 1:2 nurse-to-patient ratio. Critically ill cardiac patients receive level 1 care managed by a dedicated cardiac intensivist.12 Details of the comprehensive critical care of the Samsung Medical Center CICU have been described in previous reports.13,14 Briefly, the CICU provides noninvasive and invasive devices for monitoring hemodynamic and cardiovascular support, including mechanical ventilation and extracorporeal membrane oxygenation. Cardiac surgery support is readily available and multidisciplinary care is provided through consultation with a dietitian, pharmacist, and respiratory care practitioner.
The clinical practice guidelines for general intensive care published by The Society of Critical Care Medicine were applied. To monitor delirium, the Confusion Assessment Method for the intensive care unit (CAM-ICU) assessment was performed by nurses three times a day in patients with a Richmond Agitation-Sedation Scale score of -3 (indicating movement or eye-opening to voice but no eye contact) or higher.15 The validated Korean version of the CAM-ICU is routinely used in the CICU.16 A senior nurse rechecked the recorded CAM-ICU results on a daily basis.
Outcome and construction of the delirium prediction scoring modelDelirium was the primary outcome of this study. Delirium was defined as a positive CAM-ICU within 7 days of CICU admission. Clinical characteristics, primary diagnoses, vital signs, laboratory test results, and clinical presentations at CICU admission were included as candidate variables. To select the optimal variables for creating a delirium prediction model for CICU patients, we used several machine learning methods to assess the importance of the candidate variables, including random forest, extreme gradient boosting, partial least squares, and Plmnet-elastic.net. We assessed the importance of the variables and enhanced the appropriateness of their selection with machine learning methods. We selected 4 commonly used models for regression analysis from a range of various machine learning algorithms. Among the variables identified as highly important, we selected those that repeatedly exhibited high importance or were deemed clinically significant based on previous studies and expert consensus (J.H. Yang and R.E. Ko), were selected to construct the model.
Statistical analysisBaseline patient characteristics are summarized as numbers and proportions for categorical variables and medians with interquartile ranges [IQR, 25–75th percentiles] for continuous variables. The clinical characteristics of the delirium and nondelirium groups were compared using the chi-square or Fisher exact test for categorical variables and the Student t-test for continuous variables. Univariate logistic regression analysis was performed to estimate the odds ratios (ORs) for each variable. The ORs of each variable are reported with 95% confidence intervals (95%CIs). Coefficients, standard errors, and Z-values were also calculated.
To develop a delirium prediction scoring model, logistic regression analysis was performed using the selected variables to develop a formula for the delirium prediction model for CICU patients. For virtual internal validation, 100-repeated hold-out validation was used to further evaluate the performance of the model. To perform internal validation, the patients were divided into a 7:3 ratio. Logistic regression was conducted using the enter method, using a variable beta coefficient value to achieve more accurate predictions with small variables. In the construction of prediction models, logistic regression provides estimated regression coefficients that are of interest. These coefficients represent the log-odds of the outcome variable. To facilitate meaningful comparisons across variables, we standardized these coefficients. Standardization ensured that we evaluated the effect of each variable on a common scale. Specifically, standardization was based on the ranges of the variables, identifying the scenario in which the range of each variable was largest range. The prediction scoring model for delirium assigns scores reflecting the likelihood of delirium onset. Higher scores indicate higher risk.
We conducted a calibration plot to demonstrate that the information loss was negligible when converting the continuous values of the predictors to categorical values. The calibration plot compares the observed and predicted probabilities of delirium based on 2 models: one using the continuous values of the clinical factors as predictors, and the other using the categorical values of the clinical factors as predictors. A receiver operating characteristic curve was used to demonstrate the performance of the prediction model using the area under the curve (AUROC) and 95%CIs. All tests were 2-sided, and a P value ≤ .05 was considered to indicate statistical significance. All analyses were performed using R Statistical Software (version 3.2.5; R Foundation for Statistical Computing, Austria).
ResultsBaseline characteristics and in-hospital outcomesDuring the study period, 4261 patients aged 18 years or older were admitted to the CICU. We excluded patients who were not admitted for more than 24hours (n=1473) and those without available data on delirium (n=14). Finally, 2774 patients were included in the analysis. Of the 2774 eligible patients, 677 (24.4%) experienced delirium during CICU admission. The baseline characteristics of the patients are shown in table 1. Overall, patients with delirium were high-risk participants. More patients in the delirium group were treated with extracorporeal membrane oxygenators (12.4% vs 2.0%, P<.001) and received mechanical ventilation support (38.7% vs 5.4%, P<.001) than those in the nondelirium group. Regarding clinical outcomes, CICU death (11.4% vs 1.8%, P<.001), hospital death (18.2% vs 3.1%) and CICU length of stay (4.7 [IQR 2.4–9.0] days vs 1.9 [IQR 1.3–3.0] days, P<.001) were significantly higher in patients in the delirium group than in those in the nondelirium group.
Baseline characteristics, in-hospital management, and clinical outcomes
| Variables | Nondelirium group(n=2097) | Delirium group(n=677) | P |
|---|---|---|---|
| Age, y | 65.0 [54.0-74.0] | 72.0 [61.0-80.0] | <.001 |
| Sex, male | 1410 (67.2) | 384 (56.7) | <.001 |
| Body mass index, kg/m2 | 23.7 [21.9-25.8] | 23.7 [21.0-25.0] | <.001 |
| Comorbidities | |||
| Hypertension | 1122 (53.5) | 415 (61.3) | <.001 |
| Diabetes | 634 (30.2) | 264 (39.0) | <.001 |
| Chronic neurogenic disorder | 20 (1.0) | 26 (3.8) | <.001 |
| Chronic lung disease | 118 (5.6) | 62 (9.2) | .002 |
| Heart failure | 453 (21.6) | 228 (33.7) | <.001 |
| History of PCI | 382 (18.2) | 157 (23.2) | .005 |
| History of CABG | 110 (5.2) | 66 (9.7) | <.001 |
| History of heart transplant | 36 (1.7) | 17 (2.5) | .250 |
| Reason for admission | <.001 | ||
| Acute coronary syndrome | 1006 (48.0) | 210 (31.0) | |
| Heart failure | 531 (25.3) | 312 (46.1) | |
| Othersa | 560 (26.7) | 155 (22.9) | |
| Cardiac arrest before admission | 132 (6.3) | 141 (20.8) | <.001 |
| Severity score | |||
| SOFA score | 2 [1-4] | 6 [4-9] | <.001 |
| APACHE II score | 8 [5-12] | 17 [12-22] | <.001 |
| Shock | 273 (13.0) | 249 (36.6) | <.001 |
| Vital signsb | |||
| Systolic blood pressure, mmHg | 124 [106-143] | 116 [99-138] | <.001 |
| Diastolic blood pressure, mmHg | 73 [62-85] | 68 [57-81] | <.001 |
| Mean blood pressure, mmHg | 90 [78-104] | 85 [71-99] | <.001 |
| Heart rate, bpm | 81[68-97] | 95 [80-112] | <.001 |
| Respiratory rate | 18 [16-21] | 20 [17-24] | <.001 |
| Body temperature, °C | 36.7 [36.3-37.1] | 36.7 [36.2-37.2] | .431 |
| Saturation, % | 98 [96-99] | 97 [94-99] | <.001 |
| Laboratory testsb | |||
| White blood cell, x 103/μL | 9.26 [7.17-12.36] | 12.89 9.65-17.02] | <.001 |
| Hemoglobin, g/dL | 12.4 [10.5-14.0] | 10.1 [8.8-11.8] | <.001 |
| Platelet, x 103/μL | 187 [148-229] | 146 [94-207] | <.001 |
| Total bilirubin, mg/dL | 0.9 [0.6-1.3] | 1.1 [0.7-1.9] | <.001 |
| Aspartate transaminase, U/L | 38 [24-78] | 58 [32-192] | <.001 |
| Alanine aminotransferase, U/L | 28 [18-47] | 34 [18-103] | <.001 |
| Albumin, g/dL | 3.8 [3.5-4.2] | 3.2 [2.8-3.7] | <.001 |
| Blood urea nitrogen, mg/dL | 19.2 [14.2-27.9] | 29.4 [20.5-46.9] | <.001 |
| Creatinine, mg/dL | 1.01 [0.81-1.42] | 1.48 [0.98-2.29] | <.001 |
| Sodium, mmol/L | 138 [135-140] | 136 [133-139] | <.001 |
| Potassium, mmol/L | 4.3 [4.0-4.7] | 4.5 [4.1-5.0] | <.001 |
| Chloride, mmol/L | 104 [101-106] | 103 [99-107] | .090 |
| C-reactive protein, mg/dL | 0.90 [0.14-2.48] | 3.22 [0.90-9.42] | <.001 |
| INR | 1.10 [1.01-1.24] | 1.32 [1.13-1.83] | <.001 |
| Troponin I, ng/mL | 1.17 [0.07-12.80] | 1.17 [0.22-11.84] | .002 |
| NT-proBNP, pg/mL | 1388 [245-6255] | 7545 [1856-18 114] | <.001 |
| Lactate, mmol/L | 1.7 [1.1-2.7] | 2.2 [1.3-4.5] | <.001 |
| In-hospital managements | |||
| ECMO | 41 (2.0) | 84 (12.4) | <.001 |
| Intra-aortic balloon pump | 15 (0.7) | 13 (1.9) | .012 |
| Oxygenation support | <.001 | ||
| Mechanical ventilation | 114 (5.4) | 262 (38.7) | |
| Oxygen support | 726 (34.6) | 314 (46.4) | |
| None | 1257 (59.9) | 101 (14.9) | |
| Clinical outcomes | |||
| CICU death | 37 (1.8) | 77 (11.4) | <.001 |
| CICU length of stay, d | 1.9 [1.3-3.0] | 4.7 [2.4-9.0] | <.001 |
| Hospital death | 64 (3.1) | 123 (18.2) | <.001 |
APACHE II, Acute Physiology and Chronic Health Evaluation II; CABG, coronary artery bypass grafting; CICU, cardiac intensive care unit; ECMO, extracorporeal membrane oxygenation; NT-proBNP, N-terminal brain natriuretic peptide; PCI, percutaneous coronary intervention; SOFA, sequential organ failure assessment.
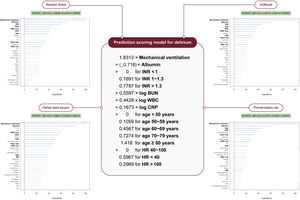
A flow diagram of the study is shown in figure 1. Using the clinical features available at CICU admission, we applied machine learning methods to assess the relevance of potential predictors. Figure 2 shows the relative importance of each variable and the performance of the model among different machine learning algorithms. Detailed ranking of the top 40 variables by their importance scores is shown in table 1 of the supplementary data. The machine learning models demonstrated good predictive performance for delirium occurrence: the random forest had an AUROC of 0.8692 (95%CI, 0.8426-0.8958), extreme gradient boosting had an AUROC of 0.8377 (95%CI, 0.8066-0.8688), partial least squares had an AUROC of 0.8662 (95%CI, 0.8400-0.8924), and plmnet-elastic.net had an AUROC of 0.8662 (95%CI 0.8400-0.8924).
Selection of features by machine learning method and score calculation formula. The figure displays the 30 most influential variables of each machine learning method. 95%CI, 95% confidence interval; ALT, aspartate aminotransferase; AST, alanine aminotransferase; AUROC, area under the receiver operating characteristic curve; BMI, body mass index; BT, body temperature; BUN, blood urea nitrogen; CABG, coronary artery bypass graft; CNS, central nervous system; CRP, C-reactive protein; DBP, diastolic blood pressure; Hb, hemoglobin; Hct, hematocrit; HR, heart rate; INR, international normalized ratio; MAP, mean arterial pressure; MCS, mechanical circulatory support; SBP, systolic blood pressure; SPO2, oxygen saturation by pulse oximetry; RR, respiratory rate; WBC, white blood cells; XGBoost, extreme gradient boosting.
Among the potential predictors, we selected those that were clinically significant and frequently ranked as highly important for developing a delirium prediction model for CICU patients. Using machine learning methods, we selected 11 variables that shared the feature of high ranking, such as mechanical ventilation, albumin, blood urea nitrogen (BUN), international normalized ratio (INR), white blood cells, C-reactive protein, age, platelet count, hemoglobin, heart rate, and creatinine. We used a minimal set of clinically meaningful and easily applicable variables selected from the repeated variables. The final model included albumin level, INR, BUN level, white blood cell count, C-reactive protein level, age, heart rate, and mechanical ventilation as predictors.
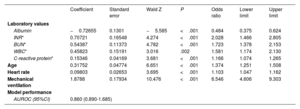
Model constructionA logistic regression model was constructed using selected variables. The predictive performance of the logistic regression model was good (AUROC, 0.860; 95%CI, 0.850-0.890, table 2). Figure 1 of the supplementary data shows a restricted cubic spline plot used to examine the association between each continuous variable and the occurrence of delirium. Age, INR, and heart rate were converted into categorical variables for ease of use in clinical settings. Age was transformed into a categorical variable using a spline curve. To facilitate clinical acceptance, we chose the cut points for heart rate and INR based on the clinical definitions. For heart rate, we used 40 bpm and 100 bpm as the cut points according to the definitions of bradycardia and tachycardia. We adopted 40 bpm as the cut point for considering the implantation of a temporary pacemaker for patients with third-degree heart block (or atrioventricular block) who had a heart rate below 40 bpm when awake.17 For INR, we used 1.2 and 1.7 as the cut points, based on the normal value of 1.2 and the application of the Model for End-Stage Liver Disease Score,18 which is a score that calculates the severity of liver disease. Finally, the delirium prediction scoring model was developed and the score calculation formula is presented in the blue box of figure 2 (AUROC, 0.861; 95%CI, 0.843-0.879). The cutoff value of 0.2 was selected based on the Youden index value. When a cutoff score of 0.2 was used, a sensitivity of 0.83 (95%CI, 0.77-0.88), specificity of 0.71 (95%CI, 0.67-0.74), positive predictive value of 0.47 (95%CI,0.42-0.53), and negative predictive value of 0.93 (95%CI, 0.90-0.95) were obtained. The results of the goodness-of-fit test between the observed probability calculated using the model with the continuous values of predictors and the predicted probability calculated using the model with the categorical values of predictors indicated no statistical difference between the 2 models, as evidenced by P=.585 (figure 2 of the supplementary data). An Excel file that enables automatic calculation of the formula with user input is provided in table 2 of the supplementary data.
Logistic regression model using selected features
| Coefficient | Standard error | Wald Z | P | Odds ratio | Lower limit | Upper limit | |
|---|---|---|---|---|---|---|---|
| Laboratory values | |||||||
| Albumin | −0.72655 | 0.1301 | −5.585 | <.001 | 0.484 | 0.375 | 0.624 |
| INR* | 0.70721 | 0.16548 | 4.274 | <.001 | 2.028 | 1.466 | 2.805 |
| BUN* | 0.54387 | 0.11373 | 4.782 | <.001 | 1.723 | 1.378 | 2.153 |
| WBC* | 0.45823 | 0.15191 | 3.016 | .002 | 1.581 | 1.174 | 2.130 |
| C-reactive protein* | 0.15346 | 0.04169 | 3.681 | <.001 | 1.166 | 1.074 | 1.265 |
| Age | 0.31752 | 0.04774 | 6.651 | <.001 | 1.374 | 1.251 | 1.508 |
| Heart rate | 0.09803 | 0.02653 | 3.695 | <.001 | 1.103 | 1.047 | 1.162 |
| Mechanical ventilation | 1.8788 | 0.17934 | 10.476 | <.001 | 6.546 | 4.606 | 9.303 |
| Model performance | |||||||
| AUROC (95%CI) | 0.860 (0.890-1.685) | ||||||
95%CI, 95% confidence interval, AUC, area under the receiver operating characteristic curve; BUN, blood urea nitrogen; INR, international normalized ratio; WBC, white blood cell count.
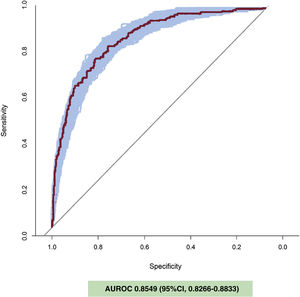
A 100-repeated cross-validation was performed using all eligible patients. In this simulation, 70% of the patients were used for training, and 30% for testing. The average cross-validated AUROC was 0.8549 (95%CI, 0.8266-0.8833; figure 3).
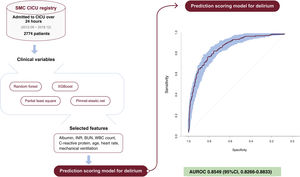
DiscussionThis study aimed to identify the clinical variables associated with the occurrence of delirium and develop a predictive scoring model for CICU patients. The main findings were as follows: a) the machine learning models for delirium prediction, such as random forest, extreme gradient boosting, partial least squares, and plmnet-elastic.net, showed good predictive performance; b) we constructed a delirium prediction scoring model using logistic regression methods with albumin, INR, BUN, white blood cells, C-reactive protein, age, heart rate, and mechanical ventilation, which were either high-importance variables in various machine learning models or clinically significant variables; c) the newly-developed risk model can be easily used at the patient's bedside. Moreover, its predictive performance is comparable to that of machine learning models and remained so in internal validation (figure 4).
Central illustration. AUROC, area under the receiver operating characteristic curve; BUN, blood urea nitrogen; CI, confidence interval; CICU, cardiac intensive care unit; INR, international normalized ratio; SMC, Samsung Medical Center; WBC, white blood cells; XGBoost, extreme gradient boosting.
Coronary care units were established in the 1960s to provide rapid resuscitation of patients with dysrhythmia resulting from acute myocardial infarction. Over time, they have evolved into CICUs, offering comprehensive critical care to patients with various cardiovascular diseases.12 Recently, with the aging population and the development of medical technologies, patients admitted to the CICU have had more complex cardiovascular diseases and severe comorbidities. Consequently, the prevention and management of delirium have become important issues for critically ill cardiac patients, similar to those in general ICUs.3 In previous studies, 2 delirium prediction models were constructed using data from patients in the general ICU: the Prediction of Delirium in ICU patients (PRE-DELIRIC) model, which used 10 predictors that could be obtained within 24hours of ICU admission, and the Early PRE-DELIRIC model, which aimed to achieve early detection of delirium risk in patients who may benefit from delirium prevention.19,20 These models demonstrated acceptable predictive performance in critically ill cardiac patients admitted to the CICU.21 However, to date, there has been no existing delirium prediction model specific to CICU patients with dedicated CICU cohorts. Therefore, our aim was to develop a delirium prediction scoring system for CICU patients.
First, we applied several machine learning methods to select highly important variables for delirium prediction. The models created by machine learning produced highly explanatory models by inputting numerous variables into algorithms, but there were clear limitations to using them at the bedside in actual clinical settings. Then, we developed a predictive scoring system, using logistic regression with selected variables that could be easily applied at the bedside. Because its performance is comparable to that of various machine learning models, this novel model may be useful in daily practice to identify patients susceptible to developing delirium, underscoring the significance of our study.
We selected variables including albumin, INR, BUN, white blood cell counts, C-reactive protein, age, heart rate, and mechanical ventilation that consistently showed high importance for the occurrence of delirium using several machine learning methods. In the CICU patients, shock and cardiac arrest were significantly more common in the delirium group than in the nondelirium group. However, these clinical factors did not show high importance in the machine learning analyses. A recent systematic review reported precipitating factors associated with delirium.22 Mechanical ventilation, albumin level, kidney injury, leukocytosis, infection, and age were identified as risk factors associated with delirium in this systematic review, which included 315 studies involving 101 144 patients. These factors were also found to be important in our analysis. Interestingly, age, BUN level, and mechanical ventilation, which are variables in the PRE-DELIRIC and Early-PRE-DELIRIC models developed for delirium prediction in general ICUs, were also highly important in our analysis. These findings suggest that in patients admitted to the CICU, variables related to general critical care are more important factors for delirium occurrence than cardiac-specific variables.
The most powerful predictors of delirium are mechanical ventilation, albumin levels, and inflammatory markers. Delirium occurs in up to 80% of the patients who undergo mechanical ventilation in the ICU.23 Mechanical ventilation is an essential intervention for critically ill patients in the CICU. The frequency of mechanical ventilation support in the CICU varies according to patient characteristics and the admission criteria; however, it is estimated to range from 13% to 40% of all CICU patients.3,24,25 Mechanical ventilation poses a risk for delirium, as it can induce physiological stress, inflammation, sedation, immobilization, and sleep disruption.26 Therefore, it is crucial to monitor and prevent delirium with optimal sedation strategies in mechanically ventilated patients in the CICU as well as to optimize the weaning and extubation processes. Analyses using the machine learning method revealed that the only vital sign associated with delirium at the time of CICU admission was heart rate. Tachycardia indicates the presence of intrinsic metabolic stress with an increased adrenergic tone.27 Tachycardia upon at CICU admission can be a manifestation of metabolic derangement and hypoxemia, which are potential contributors to delirium. Taken together, basic blood tests and monitoring of basic vital signs in critical care are more important than cardiac-specific tests to predict delirium in the CICU, as in the general ICU. Interestingly, comorbidities and previous medical history were not among the top-ranked variables. The occurrence of delirium in CICU patients seems to be more influenced by their condition at admission than by their comorbidities and previous medical history.
In this study, the delirium prediction model created uses variables that can be collected on the day of CICU admission. The model enables the prediction of delirium during the patient's CICU stay. Given the absence of curative methods for delirium, efforts should focus on identifying high-risk patients and implementing preventive measures to reduce its incidence.28 Our study highlights risk factors such as mechanical ventilation status, inflammation, and decreased albumin levels. The CICU needs to follow the basic care principles for critically ill patients that are applied in medical ICUs. Continuous assessment and enhancement of the overall critical management are necessary to address gaps. In our CICU, delirium is regularly assessed by CICU nurses using the objective and reliable CAM-ICU method thrice daily. These efforts are necessary to prevent delirium in the CICU.
LimitationsThis study has several limitations. First, the significance of our findings may have been influenced by the inherent biases of the nonrandomized registry data. However, we used an extensive database of all consecutive patients admitted to the CICU of the Samsung Medical Center. Second, this study was performed retrospectively and internally validated. Prospective interventional studies are required to verify the performance of the model and confirm its clinical usefulness. However, a 100-repeated cross-validation was conducted for the prospective simulation. Third, this study was conducted in a single level 1 care CICU. Therefore, the generalizability of the findings requires further validation. Despite these limitations, a strength of our study was that the CAM-ICU assessments were conducted by nurses 3 times daily for all consecutively admitted CICU patients. Therefore, we analyzed precise information on delirium in CICU patients.
CONCLUSIONSAfter exploring the variables associated with the occurrence of delirium using various machine learning methods, a risk model was created with variables of high importance, such as mechanical ventilation, albumin, INR, BUN, white blood cell counts, C-reactive protein, age, and heart rate. The model showed good predictive performance for delirium.
FUNDINGNone of funding.
ETHICAL CONSIDERATIONSThe Institutional Review Board of the Samsung Medical Center (approval no. 2020-10-102) waived the requirement for informed consent because of the observational nature of the study. This study considered potential sex variables according to international guidelines. Data supporting the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available because of privacy and ethical restrictions.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence was used in the preparation of this article.
AUTHORS’ CONTRIBUTIONSConception and design: R.E. Ko, J.H. Ahn, and J.H. Yang. Data analysis and interpretation: J.H. Ahn, R.E. Ko and J.H. Yang. Drafting the manuscript for intellectual content: R.E. Ko and J.H. Yang. Revision of the manuscript: J. Lee, S. Kim and S.J. Na. All authors have read and approved the final manuscript.
CONFLICTS OF INTERESTThe authors declare that they have no competing interests.
- -
The role of CICUs has expanded due to an increasingly complex patient population with more noncardiovascular comorbidities, leading to complications like those seen in general ICUs.
- -
Delirium, an acute brain dysfunction, is a significant concern in CICU settings and is associated with increased morbidity, mortality, cognitive impairment after discharge, and elevated health care costs.
- -
Despite its growing importance, there is a gap in understanding the factors associated with delirium in CICU patients, as most studies have focused on general ICUs and postcardiac surgery units.
- -
Machine learning models, including random forest, extreme gradient boosting, partial least squares, and planet-elastic.net, exhibited robust predictive abilities for delirium.
- -
We used these models to create a prediction scoring model for delirium through logistic regression, incorporating key variables such as albumin, INR, BUN, white blood cell count, C-reactive protein, age, heart rate, and mechanical ventilation.
- -
This new, easy-to-use risk model, which matches the predictive performance of its machine learning counterparts, can be readily applied at a patient's bedside, offering robust prediction for delirium.