The pathogenesis of atheromatous disease is multifactorial. Vascular lesions develop through various biochemical and cellular mechanisms, such as inflammation, oxidation, fibrosis, and cell proliferation and migration. These abnormalities are activated in response to different types of injury to the arterial intima layer. Among them, the main etiologic factor is cholesterol build-up. Excess circulating cholesterol is readily deposited on the artery wall, as it overwhelms the cholesterol extraction capacity mediated by high-density lipoproteins (HDL). Because the human body has no enzyme mechanisms to degrade cholesterol, its response to this vascular aggression is considered a foreign body reaction that attempts to mitigate the ectopic presence of cholesterol in the arterial wall, a functionally important area. The etiologic role of cholesterol in arteriosclerosis has been widely proven by basic research and clinical databases, and there are excellent recent reviews.1
LIPOPROTEIN PARTICLES, A KEY COMPONENT IN THE PATHOGENESIS OF ARTERIOSCLEROSISOne of the key issues to consider when studying the pathogenesis of arteriosclerosis is how excess cholesterol reaches the artery wall. Cholesterol is carried in the plasma by the lipoprotein system, and all lipoprotein particles carry cholesterol. In the case of triglyceride-rich lipoproteins (TRL)—such as very-low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL), and remnant lipoproteins—, there is a higher percentage of triglycerides than cholesterol. However, each particle is able to carry as many cholesterol molecules as low-density lipoproteins (LDL), and perhaps even more.2 Because all lipoprotein particles with a diameter <70nm can cross the vascular endothelial barrier, TRL should be considered an atherogenic carrier and, although they are not usually retained in the arterial intima as occurs with LDL, they do interact with macrophages, depositing cholesterol within the intima and exacerbating inflammatory mechanisms by providing a massive source of triglycerides/fatty acids.3 The cholesterol in TRL is known as remnant cholesterol (RC) and has been reported to be an even stronger predictor of cardiovascular risk than LDL-C.4,5
Among atherogenic particles, LDL carry the largest amount of plasma cholesterol. An excess increases subendothelial infiltration, which is the main pathway by which cholesterol enters the arterial wall. Once in the arterial intima, LDL are retained by components of the extracellular matrix, where they are modified in a number of ways, such as lipid peroxidation, thus activating cellular, inflammatory, and proliferative mechanisms leading to atheromatous lesion formation.1
Smaller LDL particles with a higher cholesterol density are more readily able to infiltrate the arterial wall and adhere to proteoglycans in the extracellular matrix. Consequently, the smallest, densest LDL are more atherogenic than larger LDL.6
Therefore, the atherogenic context is well defined. Cholesterol is an important etiologic factor that cannot reach the arterial wall by itself, but only as part of lipoprotein particles. Specifically, TRL deposit cholesterol by introducing it into macrophages and activating inflammatory mechanisms, with LDL particles then penetrating the wall and being retained with more or less affinity, depending on size. In short, atherogenic potential is determined by lipoprotein particles and by the number, size, and composition of these particles.
HOW IS THE COMPLEX ATHEROGENIC PROCESS EVALUATED CLINICALLY?Although 75% of all circulating molecules in plasma are lipids—among the large number of molecules involved in regulating lipid metabolism (apoproteins, enzymes, carrier proteins, and receptors)— and although the composition, size, and number of lipoprotein particles vary, clinicians assess lipid metabolism status by directly determining only 3 parameters: total cholesterol, HDL-C, and triglycerides. Even LDL-C, which is the key clinical parameter for decision-making, is a calculated value. Obviously, this classic lipid profile is insufficient to identify our patients’ proatherogenic metabolic status. One of the main limitations of this basic lipid assessment is that it does not offer an approach to the primary driver of atherogenicity, lipoprotein particles. An indirect approach would be to measure the plasma concentration of apolipoprotein B (apoB), the main apolipoprotein of atherogenic lipoproteins. This is the largest human protein (500kD), and there is only 1 molecule in each lipoprotein particle, from chylomicrons and VLDL to LDL. Therefore, elevated plasma apoB concentrations indicate a higher number of atherogenic particles, compared with low concentrations. The latest dyslipidemia and cardiovascular prevention guidelines of the European Society of Cardiology and the European Atherosclerosis Society (ESC/EAS) acknowledge that LDL-C levels are less important than atherogenic particles and that the therapeutic benefits of cholesterol-lowering drugs are mediated by the reduction in the number of particles.7 These guidelines propose apoB assay as an indirect marker more closely representative of the number of particles and establish certain apoB concentrations as secondary therapeutic targets.
Nevertheless, apoB concentrations do not indicate whether the accumulated particles are TRL, large LDL, or small LDL, for example.
IT'S TIME FOR METABOLOMICS TO BE USED IN CLINICAL MEDICINEIn the era of omic sciences, metabolomics, and lipidomics, the clinical approach to studying lipid metabolism is, to say the least, laughable.
The article by Puig-Jové et al.8 published recently in Revista Española de Cardiología offers a clinical view of the use of the lipidomic technique based on the magnetic resonance (1H-NMR) of serum to directly evaluate the number and size of the various lipoprotein particles. The use of 1H-NMR to study lipoproteins was developed several decades ago and has been employed to understand the role of these particles in cardiovascular risk. In recent years, a university-derived Spanish firm (Biosferteslab) has developed a second-generation technique and fine-tuned an advanced lipoprotein test based on 2-dimensional 1H-NMR for clinical application, the Liposcale test.9 This test evaluates the number of lipoprotein particles in the 3 main classes of lipoproteins (VLDL, LDL, and HDL) and in the 3 subclasses of each (large, medium, and small). The test also determines the mean size of each lipoprotein class, as well as the cholesterol and triglyceride content of each fraction, including RC. The technique opens up new possibilities for assessing lipid metabolism and its association with cardiovascular risk as part of the move toward precision medicine.
One example is the study by Puig-Jové et al.,8 which included patients from various hospitals who were classified as normoglycemic, prediabetic, or diabetic and were not receiving any cholesterol-lowering therapy at the time of the study. The patients’ baseline lipid values could be considered within normal limits, regardless of the need for treatment in the case of diabetics, in view of their total cardiovascular risk, and very similar between the groups. There was a clear gradient in body mass index, with a mean of 30 in patients with diabetes. Although conventional lipid parameters did not vary significantly, the NMR-assessed profile showed a gradient associated with the change in carbohydrate metabolism, with patients with diabetes showing an increase in large and small VLDL particles, a higher concentration of LDL particles (particularly smaller ones), and LDL of smaller diameter. Interestingly, fewer HDL particles were detected, with a clear tendency toward lower cholesterol and higher triglyceride levels. In general, the authors observed that 50% of patients with a normal LDL assessment based on classic parameters exhibited abnormalities in the NMR analysis. These observations were made in a group of relatively young patients with diabetes and normal triglyceride levels. In patients with more severe metabolic illness, NMR-identified abnormalities were far more substantial.
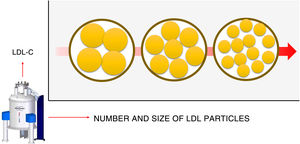
In addition to providing a detailed description of the number and size of the particles, NMR can detect discordant metabolic situations. Discordance is understood to be a situation in which the quintessential clinical parameter for therapeutic decision-making, LDL-C, does not correlate with the number of LDL particles.6 In other words, LDL-C is a marker of LDL particles. Higher LDL-C levels mean more LDL particles. However, there are metabolic situations in which this correlation is weaker, and there are individuals who need more particles to carry the same amount of cholesterol (discordant) (figure 1). Diabetes, metabolic syndrome, and obesity are all characterized by insulin resistance as a pathogenic basis and are clear examples of metabolic discordance. These patients tend to have smaller LDL, as reported by the reference article8 and, therefore, poor in cholesterol. Thus, the same LDL-C concentration but with smaller particles implies a larger number of particles. This fact is not simply a metabolic curiosity, but actually implies differences in the cardiovascular risk assessment. The number of particles is a stronger indicator than LDL-C of more potent cardiovascular risk. Patients with more LDL-C but fewer particles (therefore, with higher LDL levels) are at lower risk than others with similar or somewhat lower LDL-C levels but with more particles (small LDL particles).10
Discordance between low-density lipoprotein-bound cholesterol (LDL-C) and the number of LDL particles. Similar LDL-C amounts, depicted in the figure as the outer circle, can be carried by differing numbers of LDL particles. If these particles are smaller, a larger number will be required and their atherogenicity will be stronger. Nuclear magnetic resonance can be used to evaluate this situation. The arrow indicates an increased risk.
Other parameters are relevant as well. As mentioned, the value of RC has also been recognized in recent years.11 This is cholesterol carried by VLDL, remnant, and IDL particles. Clinical determination of this kind of cholesterol is simple but imprecise, as it is based on subtracting HDL-C and LDL-C levels from total cholesterol. Because LDL-C is already the result of a previous calculation and also includes IDL-bound cholesterol, the method is inexact. In patients with normal blood triglyceride levels, RC is usually about one fifth of the triglyceride concentration. Despite its imprecision, RC has recently been shown to have considerable predictive cardiovascular risk capacity in the PREDIMED4 and Copenhagen City Study cohorts.5 In these studies, RC was found to predict cardiovascular risk more accurately than LDL-C itself. This parameter, which includes cholesterol from all VLDL and IDL subfractions, can be precisely determined by NMR.
In summary, NMR-based study of lipoprotein metabolism provides additional information to manage patients with metabolic abnormalities or established cardiovascular diseases. In patients with residual risk despite an optimal approach, NMR yields additional data because qualitative changes not seen in conventional lipid variables tend to persist and impact the prognosis of these patients.12
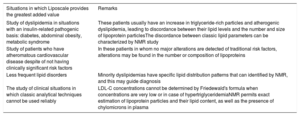
NMR-derived information on lipoprotein metabolism is robust and useful and, therefore, can no longer be neglected in the clinical assessment of our patients. Recently, a group of experts from the Spanish Society of Arteriosclerosis published a consensus document on the usefulness and indications of the clinical use of the Liposcale test to study patients with lipoprotein metabolism abnormalities and cardiovascular risk, as listed in table 1.13
Main indications for the clinical use of the magnetic resonance-assessment of lipoprotein particles
| Situations in which Liposcale provides the greatest added value | Remarks |
|---|---|
| Study of dyslipidemia in situations with an insulin-related pathogenic basis: diabetes, abdominal obesity, metabolic syndrome | These patients usually have an increase in triglyceride-rich particles and atherogenic dyslipidemia, leading to discordance between their lipid levels and the number and size of lipoprotein particlesThe discordance between classic lipid parameters can be characterized by NMR study |
| Study of patients who have atheromatous cardiovascular disease despite of not having clinically significant risk factors | In these patients in whom no major alterations are detected of traditional risk factors, alterations may be found in the number or composition of lipoproteins |
| Less frequent lipid disorders | Minority dyslipidemias have specific lipid distribution patterns that can identified by NMR, and this may guide diagnosis |
| The study of clinical situations in which classic analytical techniques cannot be used reliably | LDL-C concentrations cannot be determined by Friedewald's formula when concentrations are very low or in case of hypertriglyceridemiaNMR permits exact estimation of lipoprotein particles and their lipid content, as well as the presence of chylomicrons in plasma |
LDL-C, low-density lipoprotein cholesterol; NMR, nuclear magnetic resonance.
Modified with permission from Pintó et al.13
It is time to implement metabolomic techniques in clinical medicine, and NMR-based lipoprotein analysis is a clear example.
FUNDINGNo funding of any kind was received to undertake this study.
CONFLICTS OF INTERESTL. Masana has received lecture and consulting fees from Amgen, Amryt, Amarin, Mylan, Novartis, Sanofi, and Servier and is a member of the board of directors of Biosferteslab. D. Ibarretxe has received lecture fees from Sanofi and Rubió.