Few studies in Spain have reported the distribution of metabolic syndrome using the harmonized definition and that of premorbid metabolic syndrome, which consists of metabolic syndrome without diabetes mellitus or cardiovascular disease. Moreover, their regional distributions and clinical management are unknown. The present study examined the distributions and clinical management of both syndromes in Spain.
MethodsThis cross-sectional study was performed from 2008 to 2010 in 11 149 representative individuals of the Spanish population aged 18 years or older. Data were obtained through standardized physical examination, and analytical measurements were done in a central laboratory.
ResultsThe prevalences (95% confidence interval) of metabolic syndrome and premorbid metabolic syndrome were 22.7% (21.7%-23.7%) and 16.9% (16.0%-17.8%), respectively. The frequency of both syndromes increased with age and was higher in men than in women up to 65 years; above this age, the frequency was higher in women. The communities of the south of Spain and the Balearic and Canary islands had the highest prevalence of both syndromes, in some regions reaching double that of the community with the lowest prevalence. About one third of patients with premorbid metabolic syndrome reported that they had not received health recommendations to improve their lifestyles; of those that did receive advice, adherence was low, particularly for reducing weight (31.9%) and salt intake (38.3%).
ConclusionsThe prevalence of metabolic syndrome is high in Spain and considerable geographical differences exist in its distribution. There is substantial room for improvement in the clinical management of premorbid metabolic syndrome.
Keywords
Metabolic syndrome (MS) consists of the aggregation of various cardiometabolic risk factors (RFs), such as abdominal obesity, atherogenic dyslipidemia, and high blood pressure and blood glucose.1 Individuals with MS are at an increased risk of diabetes mellitus (DM) and cardiovascular disease (CVD).1,2 Although the very existence of MS and its clinical utility are controversial,3 the relevance of this syndrome is 2-fold. Firstly, MS serves to signal to the clinical professional that the presence of other RFs should be investigated in those patients with multiple cardiometabolic RFs. Secondly, MS enables better identification of high-risk individuals that require intervention via both clinical and public health strategies. For the purposes of this intervention, 2 main types of patients can be distinguished: those that already have DM or CVD whose prognosis is negatively affected by the elevation of the cardiometabolic RFs and who should be carefully treated, and those free of DM and CVD, described as patients with premorbid MS (PMS). These patients are the focus of primary cardiometabolic prevention, primarily through lifestyle modification and, if necessary, drugs.3
Information on MS epidemiology has been hampered by the existence of various operational definitions. Fortunately, in 2009 an international committee proposed a harmonized definition of MS that facilitates comparisons between studies.4 So far, only 2 national studies in Spain have estimated the prevalence of MS using this new definition. The DARIOS study reported the frequency of MS and PMS in persons aged between 35 and 74 years via independent analyses in 10 autonomous communities in the first decade of this century,5 whereas the di@bet.es study characterized MS frequency in persons aged between 18 and 90 years in 2009 to 2010.6 However, these studies did not report the regional frequency of MS or examine the clinical management of these patients.
Accordingly, this work describes the frequency and detailed geographical distribution of MS and PMS, as well as their clinical management, in the Spanish population aged 18 years or older in 2008 to 2010.
METHODSStudy Design and ParticipantsThe data were derived from the ENRICA study,7 whose methods have been previously published. ENRICA was a cross-sectional study performed with 12 948 representative persons from the noninstitutionalized Spanish population aged 18 years or older. Study participants were selected by stratified clustering sampling. First, the sample was stratified by province and municipality size. Next, municipalities and then census tracts were selected at random. Finally, households were randomly selected in each tract using landline phone listings, and 1 person was selected in each household. Information was collected in 248 municipalities and 1241 census tracts.
From June 2008 to October 2010, data were gathered in 3 sequential stages: a) telephone interview on lifestyle and morbidity; b) first home visit to collect blood and urine samples, and c) second home visit to perform a physical examination and obtain a dietary history. The overall response rate (for all 3 data collection phases) was 51%.
ENRICA participants provided written informed consent. The study protocol was approved by the Clinical Research Ethics Committees of Hospital La Paz in Madrid and Hospital Clínic in Barcelona.
Study VariablesMetabolic SyndromeWaist circumference was measured with a flexible inelastic tape at the midpoint between the last rib and the iliac crest at the end of a normal expiration.8 Blood glucose was measured by the glucose oxidase method after 12-h fasting.9 Blood pressure was measured under standardized conditions with validated automatic sphygmomanometers.10 Serum high-density lipoprotein cholesterol and triglyceridemia were measured by the direct method using elimination/catalase and the glycerol phosphate oxidase method, respectively.11
According to the new harmonized definition,4 diagnosis of MS requires fulfillment of at least 3 of the following 5 criteria: a waist circumference ≥ 102cm in men and ≥88cm in women; a fasting blood glucose level ≥ 100 mg/dL or treatment with antidiabetic drugs; a systolic or diastolic blood pressure ≥ 130 mmHg or ≥85 mmHg, respectively, or treatment with antihypertensive medication; a triglyceride level ≥ 150 mg/dL; and a serum high-density lipoprotein cholesterol level < 40 mg/dL in men or <50 mg/dL in women. To identify individuals with PMS, we excluded those who had a blood glucose level ≥ 126 mg/dL, were being treated with antidiabetic drugs, and had a previous diagnosis of DM or CVD (myocardial infarction, stroke, and heart failure).
Other VariablesIn addition to age and sex, participants were asked about their educational level, occupation, and tobacco and alcohol consumption. Weight and height were measured under standardized conditions with electronic weighing scales and stadiometers.8 The body mass index (BMI) was calculated as weight (in kg) divided by the square of the height (in m), and participants were divided into 3 groups: normal (BMI<25), overweight (BMI 25-29.9), and obese (BMI≥30).
Physical activity was evaluated with a validated index that combines activity at work and at leisure.12 Participants were classified into 4 categories: inactive, moderately inactive, moderately active, and active. Diet was assessed using a computerized dietary history, developed from that used in the Spanish EPIC cohort.13,14 We evaluated the extent to which the diet of the participants fulfilled the main nutritional goals15,16 and was in line with the Mediterranean diet pattern, as determined by a score equal to or greater than 9 in the MEDAS index.17
To assess the clinical management of PMS through lifestyle recommendations, the following questions were used11: “Has your doctor or nurse ever advised you to a) do any physical activity, specifically, walk at least 30min several days a week; b) lose weight; c) eat healthily, concentrating on fish, fruit, vegetables, legumes, and low-fat dairy products and reducing the consumption of red and processed meat, and d) reduce salt intake?”. The possible responses were “Yes, and I am currently following their advice”; “Yes, but I am not currently following their advice”, and “No”. Regarding giving up smoking, participants were asked “Has your doctor advised you to stop smoking?” and, additionally, if a specific program was prescribed to achieve smoking cessation.
Statistical AnalysisAnalyses were carried out with 11 149 participants with complete information on the variables of interest. The prevalences of MS and PMS were estimated, as well as their corresponding 95% confidence intervals, in the entire population and in sociodemographic- and lifestyle-defined subgroups. Associations between level of education and occupation and MS and PMS were summarized using odds ratios and 95% confidence intervals obtained via age-adjusted logistic regression. To compare the prevalence of MS and PMS among autonomous communities, estimations were standardized by age and sex using the direct method. Significance was established with a bilateral P value <.05. The main analyses were performed with the survey method in Stata v.11.18
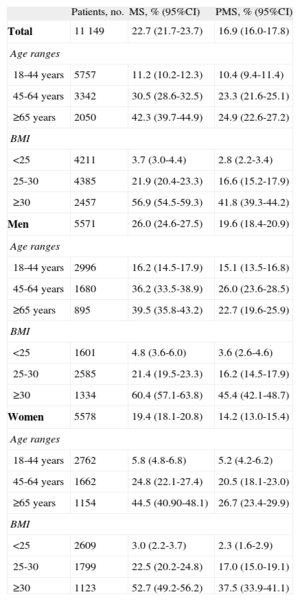
RESULTSThe prevalence of MS was 22.7% (26.0% in men and 19.4% in women). The frequency of MS increased with age, and was higher in men than in women up to 65 years; above this age, the frequency was higher in women. MS was also more frequent in men and women with higher BMIs (Table 1). The frequency of PMS was 16.9% (19.6% in men and 14.2% in women). The distribution of PMS by sex, age, and BMI was similar to that of MS (Table 1).
Prevalence of Metabolic Syndrome and Premorbid Metabolic Syndrome in the Spanish Population Aged 18 Years or Older in 2008-2010, According to Sex, Age, and Body Mass Index
| Patients, no. | MS, % (95%CI) | PMS, % (95%CI) | |
| Total | 11 149 | 22.7 (21.7-23.7) | 16.9 (16.0-17.8) |
| Age ranges | |||
| 18-44 years | 5757 | 11.2 (10.2-12.3) | 10.4 (9.4-11.4) |
| 45-64 years | 3342 | 30.5 (28.6-32.5) | 23.3 (21.6-25.1) |
| ≥65 years | 2050 | 42.3 (39.7-44.9) | 24.9 (22.6-27.2) |
| BMI | |||
| <25 | 4211 | 3.7 (3.0-4.4) | 2.8 (2.2-3.4) |
| 25-30 | 4385 | 21.9 (20.4-23.3) | 16.6 (15.2-17.9) |
| ≥30 | 2457 | 56.9 (54.5-59.3) | 41.8 (39.3-44.2) |
| Men | 5571 | 26.0 (24.6-27.5) | 19.6 (18.4-20.9) |
| Age ranges | |||
| 18-44 years | 2996 | 16.2 (14.5-17.9) | 15.1 (13.5-16.8) |
| 45-64 years | 1680 | 36.2 (33.5-38.9) | 26.0 (23.6-28.5) |
| ≥65 years | 895 | 39.5 (35.8-43.2) | 22.7 (19.6-25.9) |
| BMI | |||
| <25 | 1601 | 4.8 (3.6-6.0) | 3.6 (2.6-4.6) |
| 25-30 | 2585 | 21.4 (19.5-23.3) | 16.2 (14.5-17.9) |
| ≥30 | 1334 | 60.4 (57.1-63.8) | 45.4 (42.1-48.7) |
| Women | 5578 | 19.4 (18.1-20.8) | 14.2 (13.0-15.4) |
| Age ranges | |||
| 18-44 years | 2762 | 5.8 (4.8-6.8) | 5.2 (4.2-6.2) |
| 45-64 years | 1662 | 24.8 (22.1-27.4) | 20.5 (18.1-23.0) |
| ≥65 years | 1154 | 44.5 (40.90-48.1) | 26.7 (23.4-29.9) |
| BMI | |||
| <25 | 2609 | 3.0 (2.2-3.7) | 2.3 (1.6-2.9) |
| 25-30 | 1799 | 22.5 (20.2-24.8) | 17.0 (15.0-19.1) |
| ≥30 | 1123 | 52.7 (49.2-56.2) | 37.5 (33.9-41.1) |
95%CI, 95% confidence interval; BMI, body mass index; MS, metabolic syndrome; PMS, premorbid MS.
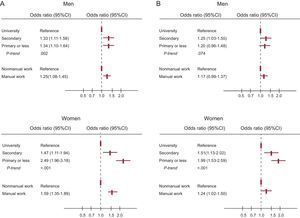
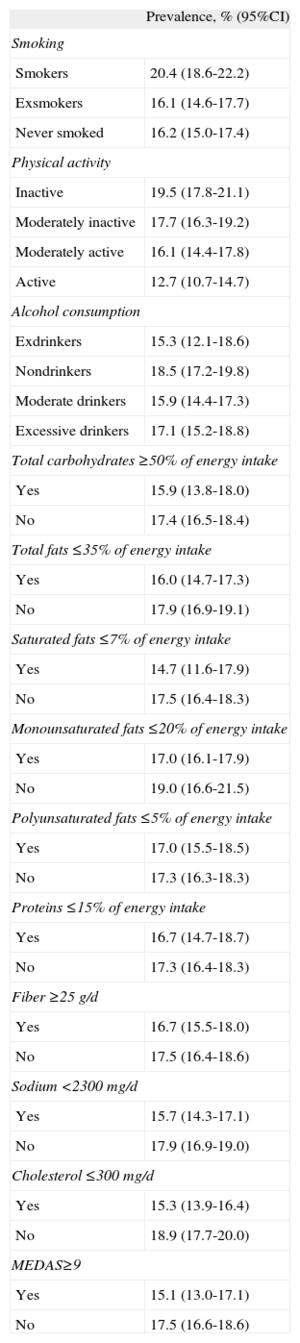
In the sex- and age-adjusted analyses, the frequency of PMS was higher in smokers and was reduced with increased physical activity (Table 2). In contrast, the frequency of PMS was higher in participants whose diet failed to fulfill most of the main nutritional goals and was not in line with the Mediterranean diet pattern (MEDAS<9 points) (Table 2). The prevalence of MS and PMS showed an inverse association with educational level and was higher in manual than in nonmanual workers; these associations were slightly stronger in women than in men (Figure 1).
Frequency of Premorbid Metabolic Syndrome According to Lifestyle, Achievement of Nutritional Goals, and Adherence to the Mediterranean Diet in the Spanish Population Aged 18 Years or Older in 2008-2010 (n=11 149)
| Prevalence, % (95%CI) | |
| Smoking | |
| Smokers | 20.4 (18.6-22.2) |
| Exsmokers | 16.1 (14.6-17.7) |
| Never smoked | 16.2 (15.0-17.4) |
| Physical activity | |
| Inactive | 19.5 (17.8-21.1) |
| Moderately inactive | 17.7 (16.3-19.2) |
| Moderately active | 16.1 (14.4-17.8) |
| Active | 12.7 (10.7-14.7) |
| Alcohol consumption | |
| Exdrinkers | 15.3 (12.1-18.6) |
| Nondrinkers | 18.5 (17.2-19.8) |
| Moderate drinkers | 15.9 (14.4-17.3) |
| Excessive drinkers | 17.1 (15.2-18.8) |
| Total carbohydrates ≥50% of energy intake | |
| Yes | 15.9 (13.8-18.0) |
| No | 17.4 (16.5-18.4) |
| Total fats ≤35% of energy intake | |
| Yes | 16.0 (14.7-17.3) |
| No | 17.9 (16.9-19.1) |
| Saturated fats ≤7% of energy intake | |
| Yes | 14.7 (11.6-17.9) |
| No | 17.5 (16.4-18.3) |
| Monounsaturated fats ≤20% of energy intake | |
| Yes | 17.0 (16.1-17.9) |
| No | 19.0 (16.6-21.5) |
| Polyunsaturated fats ≤5% of energy intake | |
| Yes | 17.0 (15.5-18.5) |
| No | 17.3 (16.3-18.3) |
| Proteins ≤15% of energy intake | |
| Yes | 16.7 (14.7-18.7) |
| No | 17.3 (16.4-18.3) |
| Fiber ≥25 g/d | |
| Yes | 16.7 (15.5-18.0) |
| No | 17.5 (16.4-18.6) |
| Sodium <2300 mg/d | |
| Yes | 15.7 (14.3-17.1) |
| No | 17.9 (16.9-19.0) |
| Cholesterol ≤300 mg/d | |
| Yes | 15.3 (13.9-16.4) |
| No | 18.9 (17.7-20.0) |
| MEDAS≥9 | |
| Yes | 15.1 (13.0-17.1) |
| No | 17.5 (16.6-18.6) |
95%CI, 95% confidence interval; MEDAS, Mediterranean Diet Adherence Screener.
Data were adjusted by age and sex.
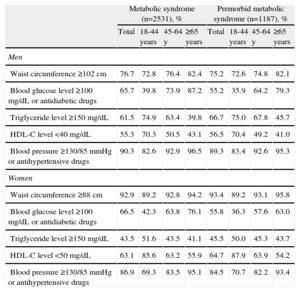
Abdominal obesity and high blood pressure were the 2 most frequent components of MS and PMS, although high blood pressure and obesity predominated among men and women, respectively. The frequency with which high blood pressure and blood glucose were components of MS and PMS increased with age, whereas the opposite occurred with dyslipidemia (Table 3).
Percentage of Cases of Metabolic Syndrome and Premorbid Metabolic Syndrome Showing Each of the Component Factors in the Spanish Population Aged 18 Years or Older in 2008-2010, According to Sex and Age
| Metabolic syndrome (n=2531), % | Premorbid metabolic syndrome (n=1187), % | |||||||
| Total | 18-44 years | 45-64 y | ≥65 years | Total | 18-44 years | 45-64 y | ≥65 years | |
| Men | ||||||||
| Waist circumference ≥102cm | 76.7 | 72.8 | 76.4 | 82.4 | 75.2 | 72.6 | 74.8 | 82.1 |
| Blood glucose level ≥100 mg/dL or antidiabetic drugs | 65.7 | 39.8 | 73.9 | 87.2 | 55.2 | 35.9 | 64.2 | 79.3 |
| Triglyceride level ≥150 mg/dL | 61.5 | 74.9 | 63.4 | 39.8 | 66.7 | 75.0 | 67.8 | 45.7 |
| HDL-C level <40 mg/dL | 55.3 | 70.3 | 50.5 | 43.1 | 56.5 | 70.4 | 49.2 | 41.0 |
| Blood pressure ≥130/85mmHg or antihypertensive drugs | 90.3 | 82.6 | 92.9 | 96.5 | 89.3 | 83.4 | 92.6 | 95.3 |
| Women | ||||||||
| Waist circumference ≥88cm | 92.9 | 89.2 | 92.8 | 94.2 | 93.4 | 89.2 | 93.1 | 95.8 |
| Blood glucose level ≥100 mg/dL or antidiabetic drugs | 66.5 | 42.3 | 63.8 | 76.1 | 55.8 | 36.3 | 57.6 | 63.0 |
| Triglyceride level ≥150 mg/dL | 43.5 | 51.6 | 43.5 | 41.1 | 45.5 | 50.0 | 45.3 | 43.7 |
| HDL-C level <50 mg/dL | 63.1 | 85.6 | 63.2 | 55.9 | 64.7 | 87.9 | 63.9 | 54.2 |
| Blood pressure ≥130/85mmHg or antihypertensive drugs | 86.9 | 69.3 | 83.5 | 95.1 | 84.5 | 70.7 | 82.2 | 93.4 |
HDL-C, high-density lipoprotein cholesterol.
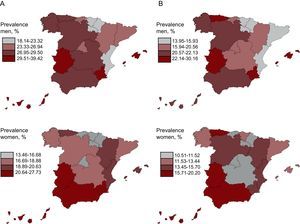
The prevalence of MS and PMS in the autonomous community with the highest prevalence was approximately twice that of the community with the lowest prevalence (Figure 2). The autonomous communities of the Region of Murcia, Balearic Islands, Extremadura, and Canary Islands showed the highest prevalence of MS among men, whereas those regions with the highest prevalence among women were Extremadura, Region of Murcia, Canary Islands, and Andalusia (Figure 2). For PMS, the Principality of Asturias and Extremadura showed the highest prevalence in both sexes, together with the Region of Murcia and Balearic Islands in men and Andalusia and the Canary Islands in women (Figure 2).
Prevalence of metabolic syndrome (A) and premorbid metabolic syndrome (B) in the Spanish population aged 18 years or older from 2008 to 2010, by autonomous community. Autonomous communities were classified into quartiles of prevalence. The analysis was standardized by sex and age.
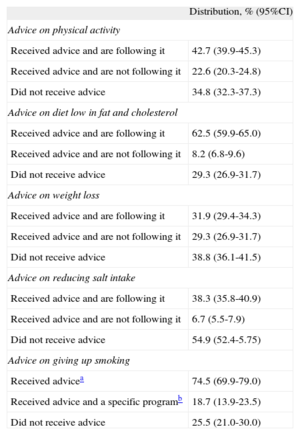
Approximately one third of patients with PMS stated that they had not received health care recommendations to improve their lifestyles, such as to increase physical activity, reduce fat and cholesterol intake, lose weight, reduce dietary salt, and quit smoking (for smokers). Moreover, only 18.7% of smokers with PMS received advice on stopping smoking that was accompanied by a specific program supporting smoking cessation. Among those who received advice, adherence was low, particularly for weight loss (31.9%) and salt intake reduction (38.3%) (Table 4).
Health Advice on Lifestyle for Patients With Premorbid Metabolic Syndrome in Spain, 2008-2010 (n=1887)
| Distribution, % (95%CI) | |
| Advice on physical activity | |
| Received advice and are following it | 42.7 (39.9-45.3) |
| Received advice and are not following it | 22.6 (20.3-24.8) |
| Did not receive advice | 34.8 (32.3-37.3) |
| Advice on diet low in fat and cholesterol | |
| Received advice and are following it | 62.5 (59.9-65.0) |
| Received advice and are not following it | 8.2 (6.8-9.6) |
| Did not receive advice | 29.3 (26.9-31.7) |
| Advice on weight loss | |
| Received advice and are following it | 31.9 (29.4-34.3) |
| Received advice and are not following it | 29.3 (26.9-31.7) |
| Did not receive advice | 38.8 (36.1-41.5) |
| Advice on reducing salt intake | |
| Received advice and are following it | 38.3 (35.8-40.9) |
| Received advice and are not following it | 6.7 (5.5-7.9) |
| Did not receive advice | 54.9 (52.4-5.75) |
| Advice on giving up smoking | |
| Received advicea | 74.5 (69.9-79.0) |
| Received advice and a specific programb | 18.7 (13.9-23.5) |
| Did not receive advice | 25.5 (21.0-30.0) |
95%CI, 95% confidence interval.
This study shows that almost a quarter of Spanish adults has MS and almost a fifth has PMS. Our results also reveal marked geographical differences in the distribution of these syndromes and substantial opportunities for improving the clinical management of PMS.
The frequencies of MS and PMS in the ENRICA study were lower than those found in the DARIOS study, which reached 31% and 34%, respectively, in persons aged 35 to 74 years.5 However, these data are not directly comparable because they correspond to different age groups and because the DARIOS study only included data from 10 autonomous communities. Our prevalence rates were also lower than those of the di@bet.es study, which reported an MS prevalence of 42% in men and 32.3% in women6; the higher prevalence of MS in the di@bet.es study may be due to the use of lower cutoff values for waist circumference (>94.5 cm for men and >89.5 cm for women) and because the mean age of the participants in the di@bet.es study was about 5 years higher than in the present study. Finally, the prevalence of MS in our study was also lower than that in the United States, which was 36.1% in men and 32.4% in women according to the harmonized definition.19 This rate is in line with the higher prevalence of general obesity in the United States, which was 34% in the United States in 2007-2008,20 and compares to 23% in Spain in 2008-2010.8
The distribution of MS by age, sex, and socioeconomic status (education or occupation) is because the MS epidemic is largely the result of the obesity epidemic. Accordingly, as for general obesity, the frequency of MS in individuals younger than 65 years was higher in men than in women.8 The predominance of obesity and MS in young and middle-aged men is due to a greater increase in obesity among men than women in Spain in recent decades.21 In contrast, as for general obesity, the socioeconomic gradient of MS was higher in women than in men.8,22 The reasons for this disparity are not well known, although the desire to be slim may be greater for women, particularly in higher social classes; in addition, a larger body size may be an indicator of masculinity and physical power for men, independent of social status.23 Our results on the distribution of MS by age and sex are consistent with previous results from Spain6 and the United States,20 like those observed for the socioeconomic gradient.5,6,20
PMS was associated with unhealthy lifestyles, particularly smoking, poor quality diet, and physical inactivity. This association was expected because some of these lifestyle habits, such as diet and physical activity, contribute to the pathogenesis of obesity. Our results also support the preferential use of lifestyle management in the control of PMS.
The 2 most common components of MS and PMS were abdominal obesity and high blood pressure. This finding is due to the high prevalence of abdominal obesity, which was 36%,8 and hypertension (≥140/90mmHg or antihypertensive treatment), which was 33%,10 among persons aged 18 years or older in 2008 to 2010 in Spain. This result also indicates that central obesity could play a major role in the pathogenesis of MS. Moreover, the higher frequency of altered blood glucose as a component of MS with an increase in age reflects the progressive deterioration of pancreatic function as well as the increase in insulin resistance due to age-associated fat infiltration of the muscle and liver.
Our study is the first to completely characterize the variations in the frequency of MS and PMS among autonomous communities. As expected, in the age- and sex-standardized analyses, the regional frequency of MS strongly correlated with that of general abdominal obesity (Pearson's correlation, r=0.4 in men and r=0.73 in women). Moreover, the communities of the south of Spain and the Balearic and Canary Islands have shown a higher frequency of obesity and higher cardiovascular risk for many decades.24,25 Some factors associated with lifestyle (such as sedentary behavior, poor diet quality, and greater tobacco consumption) and, in particular, a lower socioeconomic level are a likely cause of the higher cardiovascular risk in these regions.26 The marked geographical variations in the frequency of PMS in Spain reveal a huge potential for prevention that has remained unexploited for many years. The current economic difficulties should not impede public authorities from promoting socioeconomic development and health interventions aimed at reducing health inequalities in Spain.
Finally, our study showed considerable deficiencies in lifestyle interventions, which are key to the clinical management of patients with PMS. Other studies in Europe, which also included Spanish patients, showed shortcomings in behavioral interventions for cardiometabolic risk in primary prevention.27 The good news is that there is evidence that patient education and reorientation of health care systems (eg, enhancement of electronic medical records, teamwork, clinical follow-up) can reduce blood glucose, blood pressure, and cholesterol in patients at high cardiometabolic risk.28
Strengths and LimitationsThis study has a number of limitations and strengths. One limitation is a possible underestimation of the prevalence of MS and PMS because we omitted the institutionalized population, a group that usually has a greater number of cardiometabolic RFs. Another limitation is that the information concerning health advice on lifestyles was based on patient reports, which may be subject to errors in interpretation and memory. Among the strengths of the study are the large sample size and its representativeness of the adult population of an entire country. In this regard, the response rate in the ENRICA study was among the highest of the surveys monitoring population health performed in Europe.29 In addition, the age, sex, and socioeconomic structure of the sample mirrors that of the Spanish population.7 Moreover, similar results were found for variables covered by comparable questions in both the ENRICA study and the European Health Survey in Spain 2009.30 For example, the prevalences of diagnosed DM, diagnosed hypertension, and smoking in the ENRICA study and in the European Health Survey in Spain 2009 were 5.5% and 5.9%, 19.8% and 17.5%, and 27.5% and 29.9%, respectively. Other strengths are that the anthropometry and blood pressure measurements were performed under standardized conditions and that all analytical measurements were done in the same laboratory with appropriate quality controls.
CONCLUSIONSThis study shows a high proportion of Spanish adults with MS and PMS, conditions that carry a high relative risk of DM and CVD in the short- and medium-term. Unless the obesity epidemic is controlled and action is taken on unhealthy lifestyles through clinical strategies and public health, the high frequency of MS and PMS could threaten the achievements made in recent decades in the control of coronary heart disease in Spain.31 Our results also illustrate the need to improve lifestyle interventions in patients with MS and PMS in primary health care.
FUNDINGThe data for this analysis came from the ENRICA study, which was financed by Sanofi-Aventis. Specific funding for this analysis came from the FIS PI12/1166 and PI11/01379 projects and from the “UAM Chair in Epidemiology and Control of Cardiovascular Risk”. This study was directed by an independent scientific committee.
CONFLICTS OF INTERESTM. Teresa Aguilera is an employee of Sanofi-Aventis. However, Sanofi-Aventis does not currently market any product for the treatment of MS.