Resistant hypertension is a clinical problem because of its difficult management and increased morbidity and mortality. Catheter-based renal denervation has been demonstrated to improve control in these patients. The results of establishing a multidisciplinary unit for the implementation of renal denervation in the management of resistant hypertension are described.
MethodsA team of nephrologists and cardiologists created a protocol for patient selection, intervention, and follow-up. One hundred and ninety-seven patients with poorly controlled essential hypertension, despite taking 3 or more drugs, were included. The ablation technique previously described was supported by a navigator based on rotational angiography. Blood pressure at baseline and after follow-up was compared using the Wilcoxon test for paired samples.
ResultsOne hundred and eight patients (55%) with pseudo-resistant hypertension were excluded. The other 89 were given antialdosteronic drugs, to which 60 patients (30%) responded. The remaining 29 patients (15%) were candidates for denervation. Eleven patients, with blood pressure 164/99mmHg and taking 4.4 antihypertensive drugs, were ablated. After 72 days of follow-up, systolic and diastolic blood pressure fell by 25 mmHg (P=.02) and 10 mmHg (P=.06), respectively. In 10 patients (91%) at least 1 drug was discontinued.
ConclusionsRenal denervation performed by a multidisciplinary team led to an improvement in blood pressure similar to previous studies, with a greater reduction of antihypertensive drugs.
Keywords
.
INTRODUCTIONHypertension is a public health problem of the first magnitude because of its high prevalence and the significant increase in cardiovascular morbidity and mortality involved.1 Currently, the treatment of hypertension is based on 2 factors: modifying certain lifestyle habits and the use of antihypertensive drugs.2 Blood pressure (BP) control continues to be poor in almost 50% of hypertensive patients3,4 due to poor adherence to treatment and/or the inefficacy of the available drugs.
In this setting, resistant hypertension (RH) is defined as a situation in which the BP values are >140/90 mmHg despite the patient taking 3 or more drugs, including a diuretic, at appropriate doses.5 The prevalence of RH remains unclear, but it is estimated at around 13% of the patients in treatment. The presence of RH entails an increase in mortality and increased disease in target organs compared to the rest of the hypertensive population.6
The sympathetic nervous system plays an important role in the persistence and progression of hypertension. Sympathetic innervation reaches the kidney through the adventitia of the renal artery. Efferent sympathetic nerve activity produces renal vasoconstriction and increases renin production and sodium retention, leading to increased blood volume and thus increased BP; in turn, afferent renal sympathetic nerves, in response to hypoperfusion, modulate the systemic sympathetic response to produce vasoconstriction and an increase in BP.7,8
Recently, catheter-based renal denervation (RD) has been developed, a procedure based on the application of radiofrequency energy within renal arteries to modulate the mechanisms described above. After a promising preclinical study9 in animal models, the efficacy and safety of this therapy in humans was supported by the Symplicity studies. The nonrandomized Symplicity HTN-1 study10 demonstrated the feasibility and safety of RD, without ablation-associated complications in renal arteries. Subsequently, the Symplicity HTN-2 trial,11 which included 106 patients randomized to conventional treatment or RD, showed a decrease in office blood pressure measurements (OBPM) of 30/11 mmHg at 6 months, with a reduction in drug treatment in 20% of denervated patients. The longer-term follow-up of patients from the Symplicity HTN-1 study showed that the benefit of this therapy was sustained for at least 2 years of follow-up.12
Currently, little information is available on the clinical setting in which this therapy is provided, the specialists who perform it, and the results it can offer outside the context of clinical trials.
The aim of this study was to describe the creation of a multidisciplinary RD unit integrated within the hospital's nephrology and cardiology services and the implementation and outcomes of the RH management program designed for this unit.
METHODSCreation of the Renal Denervation UnitA multidisciplinary team was created for implementing RD. The team consisted of nephrologists from the hypertension unit who were responsible for selecting and following up the patients and interventional cardiologists from the arrhythmia and cardiac catheterization units who were trained in RD and performed the procedures. The team created a clinical protocol for patient selection, intervention and follow-up. A specific informed consent form was designed, approved by the quality control committee.
Study PopulationBetween June 2011 and June 2012, the team preselected 197 patients with essential hypertension who had systolic OBPM values>140mmHg or diastolic OBPM values>90 mmHg despite taking 3 or more drugs (including a diuretic). The patients also met the following criteria: estimated glomerular filtration rate>45 mL/min/1.73 m2; the absence of coronary or cerebrovascular events in the last 6 months; absence of renal stenosis documented by Doppler ultrasonography; and no contraindications for femoral catheterization.
OBPM was measured in all patients at least 3 times per visit, taking the average of the last 2 measurements to minimize white-coat syndrome. All potential candidates also underwent 24-h ambulatory blood pressure monitoring (ABPM).
Prior to ablation, all the patients selected for RD underwent computed tomography angiography (CTA) of the abdominal aorta to exclude patients with small renal arteries (diameter<4 mm and length<20 mm) and to check for stenosis or anatomical variants relevant to the ablation procedure.
ProcedureThe design of the intervention was partly guided by information from the Symplicity study and the manufacturer's recommendations. A new tool was added to support the procedure: rotational angiography with a fluoroscopic navigation system for renal artery reconstruction (Allura 3D Rotational Angiography, Philips Medical Systems Inc.; Best, The Netherlands).
The procedure consisted of rotational aortography using a pigtail catheter introduced via the femoral artery and the selective canalization of each renal artery using a guide catheter to introduce a specific ablation catheter (Symplicity Catheter System, Ardian/Medtronic Inc.; California, United States) advancing it to the distal portion of the artery.
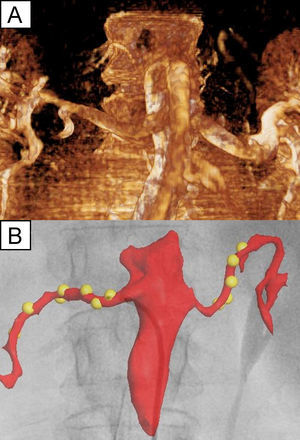
Rotational angiography was performed with the automatic synchronized injection of 70 mL of contrast medium at 14 mL/s during a 220° rotation of the C-arm over 4.4 s using a pigtail catheter placed in the abdominal aorta. This type of angiography provides a 3-dimensional cast of the renal arteries for its projection on the X-ray screen making it possible to know the position of the catheter relative to the renal artery at all times and to mark each application point of radiofrequency energy on the cast. Figure 1 shows an example of an image obtained by aortography and the screen-shot obtained by the navigation system after lesion ablation.
A, Rotational angiography of the abdominal aorta and both main renal arteries of 1 patient. B, fluoroscopic navigation system screenshot showing an anatomical reconstruction based on the fluoroscopic image superimposed on the previous image, as well as the radiofrequency lesions (yellow spheres) created by the catheter, which is located near the ostium of the right renal artery.
Radiofrequency energy was applied for 2min at 8 W in each artery after heparinization; correct contact was monitored radiologically and by using temperature and impedance curves provided by the radiofrequency source. The aim of the procedure was to deliver as many applications as possible, 0.5 cm apart, to a maximum of 8 applications per artery. Before and after ablation, selective angiography was performed in each renal artery following the administration of intraarterial nitroglycerine to prevent spasm, making it possible to correctly assess the vessel.
The procedures were performed under conscious sedation administered by the operators. Midazolam and fentanyl were administered according to the protocol used in our electrophysiology laboratory during other painful ablation procedures: an initial bolus of midazolam (1 mg or 2 mg) and fentanyl (0.05 mg) and additional boluses of fentanyl (0.03 mg to 0.05 mg) were administered depending on the response.
Follow-upFollow-up was conducted in the office of the hypertension unit, with scheduled visits in the first week and 1, 3, and 6 months after ablation. During each visit, the patients underwent clinical assessment and their OBPM was measured. ABPM and Doppler ultrasonography of the renal arteries were performed at 1 month and 6 months. Blood tests were performed 24 h after the procedure and at 1 month to monitor renal function.
Treatment with antihypertensive drugs was adjusted during each visit at the discretion of the nephrologist, depending on BP values and the patient's symptoms.
Statistical AnalysisContinuous variables are expressed as mean (standard deviation) and discrete variables as percentages.
BP values before and after ablation were compared using the nonparametric Wilcoxon test for paired samples, given the small sample size. We used the two-tailed version using a P value of <.05 as a cutoff for statistical significance in all comparisons.
SPSS 14.0 for Windows was used for data analysis.
RESULTSCandidate SelectionABPM was performed in the 197 patients with elevated OBPM; average BP values were<140/90 mmHg in 108 of the patients (55%) during the activity period and these patients were classified as having pseudoresistant hypertension.
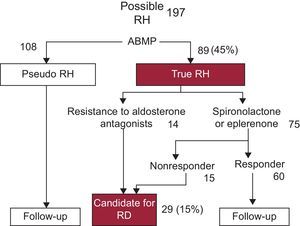
In the remaining 89 patients, aldosterone antagonists (spironolactone or eplerenone) were administered to counter the risk of secondary hyperaldosteronism. Spironolactone (50 mg/day and 100 mg/day) or eplerenone (25 mg/day and 50 mg/day) were administered at the discretion of the nephrologist. During follow-up, 60 patients (30%) had improved systolic or diastolic BP values by at least 20 mmHg or 10 mmHg, respectively. A total of 29 patients (15%) who did not respond to aldesterone antagonists or with intolerance to them were selected as candidates for RD. Figure 2 shows a diagram of the selection protocol used.
Management of patients with possible resistant hypertension in the study. Note that ambulatory blood pressure monitoring excluded the majority of patients with pseudoresistant hypertension and indicated their observed response to aldosterone antagonists, which led to only 15% of patients being selected as candidates for renal denervation. ABPM, ambulatory blood pressure monitoring; RD, renal denervation; RH, resistant hypertension.
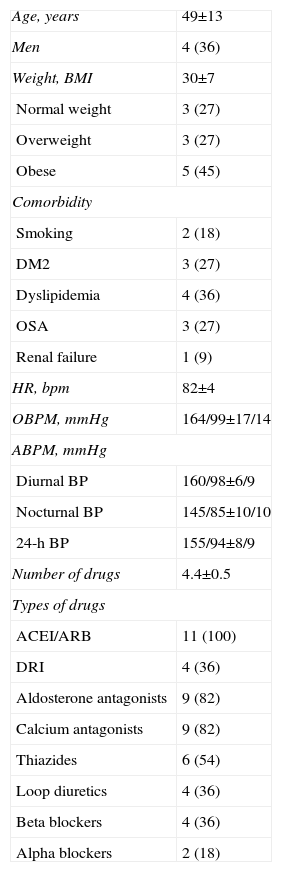
This paper describes the first 11 patients treated in our center between February 2012 and June 2012 who met the selection criteria described. Table 1 shows the baseline characteristics of these patients.
Baseline Characteristics of Patients Undergoing Renal Ablation
| Age, years | 49±13 |
| Men | 4 (36) |
| Weight, BMI | 30±7 |
| Normal weight | 3 (27) |
| Overweight | 3 (27) |
| Obese | 5 (45) |
| Comorbidity | |
| Smoking | 2 (18) |
| DM2 | 3 (27) |
| Dyslipidemia | 4 (36) |
| OSA | 3 (27) |
| Renal failure | 1 (9) |
| HR, bpm | 82±4 |
| OBPM, mmHg | 164/99±17/14 |
| ABPM, mmHg | |
| Diurnal BP | 160/98±6/9 |
| Nocturnal BP | 145/85±10/10 |
| 24-h BP | 155/94±8/9 |
| Number of drugs | 4.4±0.5 |
| Types of drugs | |
| ACEI/ARB | 11 (100) |
| DRI | 4 (36) |
| Aldosterone antagonists | 9 (82) |
| Calcium antagonists | 9 (82) |
| Thiazides | 6 (54) |
| Loop diuretics | 4 (36) |
| Beta blockers | 4 (36) |
| Alpha blockers | 2 (18) |
ABPM, ambulatory blood pressure monitoring; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; BMI, body mass index; BP, blood pressure; DM2, diabetes mellitus 2; DRI, direct renin inhibitors; HR, heart rate; OBPM, office blood pressure measurement; OSA, obstructive sleep apnea.
Data are expressed as no (%) or mean±standard deviation.
The procedure was performed without incident in all patients. Preprocedural CTA identified anatomical variants or renal artery lesions in 2 patients (a polar artery in 1 patient and a moderate stenosis proximal to the ostium of one of the renal arteries in the other). Aortography and selective catheterization revealed 4 additional variants not identified by CTA (2 polar arteries, 1 double-barrelled bifurcation of the renal artery and 1 anastomosis of the renal artery with the phrenic artery).
Each renal artery received between 4 and 8 applications of radiofrequency energy, avoiding its application to the anatomical variants and lesions described above. Each patient received an average of 12.1 (1.3) applications. The mean total procedure time was 92 min; mean fluoroscopy time was 16 min. A mean of 171 (42) mL contrast agent was administered.
During the application of radiofrequency energy, 2 patients (18%) presented bradycardia<45 bpm in response to pain as a complication of the ablation procedure, which was resolved by administering atropine and interrupting the application. There were no cases of arterial spasm. Two patients presented femoral-puncture associated complications some hours after surgery: 1 inguinal hematoma due to percutaneous closure device failure, which was controlled by manual compression and 1 psoas muscle hematoma that caused pain during the afternoon following the procedure but resolved itself. In no case was transfusion or reoperation needed.
Follow-up of Denervated PatientsAll patients were discharged 24 h after surgery, except for the patient with a retroperitoneal hematoma who was discharged 72 h after surgery. A predischarge blood test was performed in all patients; none suffered deteriorated renal function after ablation.
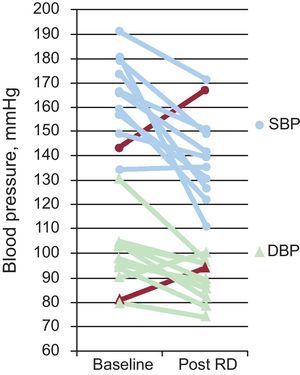
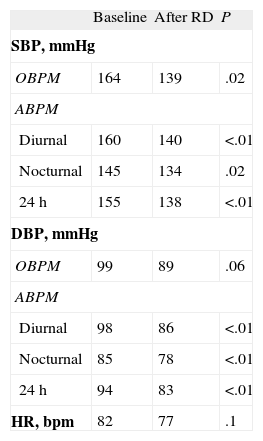
Mean follow-up time in the denervated patients was 72 days. During this period, there was a mean decrease in OBPM values of 25/10 mmHg. The ABPM showed decreases in diurnal BP of 20/10 mmHg, in nocturnal BP of 11/7 mm Hg, and in 24-h BP of 17/11 mmHg. All the decreases in BP were statistically significant (P<.05), with the exception of diastolic OBPM (P=.06). Table 2 shows a summary of the BP values and heart rate obtained at baseline and at the end of follow-up. Figure 3 provides detailed information on OBPM values at baseline and at the end of follow-up in each denervated patient.
Measurements of Blood Pressure at Baseline and at Follow-up in Denervated Patients
| Baseline | After RD | P | |
| SBP, mmHg | |||
| OBPM | 164 | 139 | .02 |
| ABPM | |||
| Diurnal | 160 | 140 | <.01 |
| Nocturnal | 145 | 134 | .02 |
| 24 h | 155 | 138 | <.01 |
| DBP, mmHg | |||
| OBPM | 99 | 89 | .06 |
| ABPM | |||
| Diurnal | 98 | 86 | <.01 |
| Nocturnal | 85 | 78 | <.01 |
| 24 h | 94 | 83 | <.01 |
| HR, bpm | 82 | 77 | .1 |
ABPM, ambulatory blood pressure monitoring; DBP, diastolic blood pressure; HR, heart rate; OBPM, blood pressure measured in office; RD, renal denervation; SBP, systolic blood pressure.
A P-value of <.05 was used as a cutoff for statistical significance for all comparisons.
Changes in systolic blood pressure and diastolic blood pressure obtained at baseline and after follow-up in the 11 who underwent renal denervation. DBP, diastolic blood pressure; RD, renal denervation; SBP, systolic blood pressure. The red line indicates the progress of the patient considered to be a nonresponder.
At least 1 drug was discontinued in 10 (91%) of the 11 patients and an average of 1.4 (0-3) drugs were discontinued per patient.
Doppler ultrasonography performed during follow-up showed that no patient had experienced complications.
DISCUSSIONThe RD program implemented in our center obtained results that confirm the scientific evidence regarding the role of renal ablation in improving BP control, as shown by the reduction in both OBPM and ABPM values.
Candidate selection was based on the exclusion of pseudoresistent hypertension by clinical assessment, ABPM, and response to treatment with aldosterone antagonists. In this sense, it differs from the Symplicity trial, which used the systolic BP value (>160 mmHg) alone to select candidates for ablation. Observational studies have shown that aldosterone antagonists significantly improve BP control in resistant patients,13–16 bearing in mind the possible occurrence of secondary hyperaldosteronism. The only randomized trial currently available also demonstrated a favorable, although moderate, effect of spironolactone vs placebo in RH control.17 Despite this evidence, it is noteworthy that 17% of the patients included in the Symplicity trial were treated with aldosterone antagonists compared to 82% of the patients in our series, all nonresponders who were maintained on these drugs before ablation. Although it is unknown whether treatment with aldosterone antagonists can improve the response to RD, in our series the administration of aldosterone antagonists improved BP control in 60 of 89 patients (67%) with true RH, indicating that once the pseudoresistant population is excluded, therapeutic treatment with aldosterone antagonists can reduce the need for renal ablation in a large number of patients.
The decrease in OBPM values by 25/10 mmHg after 72-day follow-up is similar to that reported in the Symplicity HTN-2 trial11 (24/8 mmHg at 3 months). However, the reduction in the use of antihypertensive drugs was much greater in our series than was described in that study (91% vs 20% of patients, respectively). However, reducing the number of drugs was not formally included in the clinical trial, whereas this was an aim in our protocol, which may partly explain the difference found. The only reduction that did not reach statistical significance was diastolic OBPM; this is probably explained by white-coat syndrome having a relatively stronger effect on these values than it does on systolic BP values or ABPM pressures. The diastolic OBPM values were demonstrated as only having a tendency to decrease, which may have reached statistical significance had more patients been included in the sample.
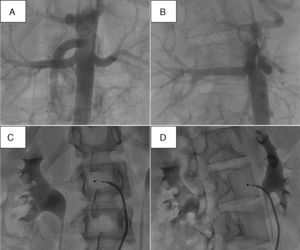
The RD procedure is characterized by the absence of a specific target other than completing a specific number of lesions in each artery. Currently, the optimal number of applications remains unknown; both Symplicity trials10,11 administered between 4 and 6 applications. Given the uncertainty about a potential dose-response effect, the procedure designed in our center is based on the idea of creating as many lesions as possible (up to 8 per artery). Thus, the maximum number of lesions possible depends on the length of artery treated and whether or not there are anatomical variants. In this sense, preoperative rotational aortography has proved very useful, since the projection in which the artery is longest can be selected, which facilitates a greater number of applications (Fig. 4).
Illustration showing how rotational angiography may be used to select the oblique projection in which the length of the artery is at its greatest. A and B, images acquired by rotational angiography in different right oblique views of the right renal artery; note how the length of the vessel is shown at its longest in B. C and D, working projections equivalent to image A and B, respectively. D, projection that allows the retraction of the catheter while performing a greater number of applications than in the projection shown in C.
Anatomical variants or lesions were identified in 6 of 11 patients, either by CTA or, more often, during the operation itself. The presence of nonsignificant stenosis or polar arteries was not an exclusion criterion for RD, whereas this was a criterion in the Symplicity studies. In the 3 patients with polar arteries, ablation was performed in the main renal artery alone. A more conservative approach would be to perform RD in the kidney without abnormalities or anatomical variants, but it is currently unknown which of the two has the better risk-benefit ratio. The presence of bifurcations, secondary branches, or renal artery stenosis highlights the need for careful anatomical assessment of the vessel during the procedure to ensure safety.
The manufacturer recommends creating lesions in a spiral pattern along the arterial wall to achieve a higher proportion of sympathetic innervation and avoid potential complications such as vessel stenosis. Since conventional fluoroscopy is a 2-dimensional imaging technique, it cannot accurately determine the actual position of the catheter relative to the artery wall. In this sense, fluoroscopic navigation makes it easier to create the spiral pattern, since the position of the previous applications can be marked (Fig. 1). Another potential benefit is provided if a second ablation procedure is needed in a nonresponder patient, since a map of the previous applications is available.
One of the patients presented normal BP at the first follow-up visit. After presenting symptoms of orthostasis, antihypertensive treatment was reduced and as a result OBPM was elevated in the final follow-up (the red line shown in Fig. 2 corresponds to this patient). The ABPM values were similar or slightly lower after ablation (24-h ABPM changed from 152/88 mmHg to 147/86 mmHg), indicating a white-coat syndrome component in the OBPM). This patient was the only one considered to be a nonresponder, as the other patients had decreased systolic and/or diastolic OBPM pressures. This patient was one of the 2 patients with a polar artery in one of the kidneys and the oldest in the series (65 years). The percentage of nonresponders was similar to that reported in the Symplicity HTN-2 trial.11
The results of the program were made possible by the close collaboration of physicians from different areas of expertise. The vital role of nephrologists from the hypertension unit in patient selection and management is indisputable. All the denervation procedures were performed by 2 cardiologists specializing in different areas: an interventional cardiologist and electrophysiologist. However, the participation of both specialists may not be necessary. With the aim of increasing experience and ensuring the best results, we recommend that in each center the technique should be performed by specialists who have been introduced to the technique and have performed it since its implementation. However, it seems important that potential candidates should be studied by hypertension specialists (nephrologists, cardiologists, and internists, depending on the center), in centers with experience, as recommended by the European Society of Hypertension.18
LimitationsWe have only presented the first 11 patients treated with RD out of the 29 patients accepted for the procedure, which may represent a selection bias. No comparative data are available regarding the patients who were not denervated. The selection procedure was based on a systolic BP>140 mmHg confirmed by ABPM and following a response to aldosterone antagonists and thus was different to what has demonstrated efficacy in previous studies (systolic BP>160 mmHg)10,11 and cannot be adequately validated due to the absence of a control group. For the same reason, a placebo effect may occur in response to denervation or this may have led to increased adherence to the low-sodium diet and drug therapy. Rotational angiography and the navigation system were systematically used in all patients without comparison to the conventional approach. Thus, their possible impact on the amount of contrast medium used and the efficacy or safety of the procedure remains unknown. For this, it would be necessary to randomize the use of rotational angiography vs the technique performed under conventional fluoroscopic guidance. As this was the first group of patients treated in our center, the learning curve, though relatively short, could have interfered with the results of the program. The low number of denervated patients is the main limitation of the study and makes it impossible to draw conclusions about the variables that are associated with a better or worse response to therapy.
CONCLUSIONSThe protocol designed in our center for the selection of candidates for RD excludes most patients with poorly controlled hypertension and who are taking 3 or more drugs due to pseudoresistence or improvement after the use of aldosterone antagonists. This highlights the importance of adequate clinical assessment of patients with suspected RH before RD is indicated.
Patient selection and the procedure performed in the first denervated patients led to improved OBPM values in a number of cases and in similar numbers to those reported in previous studies, but with greater reductions in the use of antihypertensive drugs.
FUNDINGThe authors thank the Fondation pour la prevention des maladies cardiovasculaires (Geneva, Switzerland) for financing the ablation catheters used in the study.
CONFLICTS OF INTERESTNone declared.