Cardiovascular disease remains the main cause of morbidity and mortality in the 21st century,1 and the situation is not expected to change in the next 2 decades.2 This epidemic could be contained or even decreased if there were a social change in favor of a healthier lifestyle and diet, such as the Mediterranean diet (MedD). Several years ago, the low incidence of morbidity and mortality from coronary heart disease in Mediterranean countries created great interest. In fact, the number of PubMed publications on this topic increased from fewer than 10 in 1985 to about 300 in 2012. Many of these were observational studies (ecological, cohort, or case-control) in which increased adherence to the MedD was accompanied by reduced cardiovascular risk. In addition, numerous small clinical trials have observed the effects of this diet or its main components on intermediate variables of cardiovascular risk such as blood pressure, blood lipids, insulin resistance, or endothelial function,3 adding plausibility to epidemiological studies by demonstrating possible mechanisms by which the MedD provides cardiovascular protection. However, in the era of evidence-based medicine, nutritional recommendations should be based on randomized interventional studies that analyze “hard” variables such as cardiovascular death, myocardial infarction, or stroke.
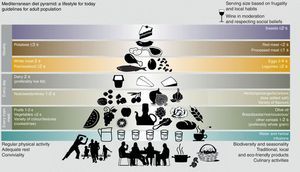
MEDITERRANEAN DIETThe MedD is defined as a dietary pattern typical of the early 1960s in Mediterranean countries where olive trees grow (Greece, southern Italy, and Spain). Although there is no single MedD, its main features are as follows: a) high fat consumption (more than 40% of the total energy intake), mainly in the form of olive oil; b) high consumption of unrefined cereals, fruit, vegetables, legumes, and nuts; c) moderate to high consumption of fish; d) moderate to low consumption of white meat (poultry and rabbit) and dairy products, mainly yogurt or fresh cheese; e) low consumption of red meat and meat products, and f) moderate consumption of wine with meals.4 This pattern and the proportions of the foods that comprise it are shown as a “food pyramid” (Fig. 1).4 Two major changes have been made in the last update. These changes refer to cereals and dairy products; in general, these should be whole-grain and skimmed, respectively. Other lifestyle habits have also been added, such as physical exercise, socializing, and sharing meals with family and friends.
Mediterranean Diet Pyramid Created by the Fundación Dieta Mediterránea de Barcelona (Mediterranean Diet Foundation of Barcelona [2010 edition]). s: serving. The use and promotion of this pyramid is recommended without any restriction. Reprinted with permission from Bach-Faig et al.4
A great deal of scientific evidence has shown that the vast majority of chronic diseases, including cardiovascular diseases, are largely preventable by lifestyle and dietary measures; hence the recommendations of many scientific societies and government bodies in this regard. However, both in primary care and specialist settings, “preventive” treatment usually involves prescribing lipid-lowering, antihypertensive, and other drugs rather than giving priority to educational interventions aimed at changing unhealthy lifestyles. Without denying the efficacy of these drugs, the postponement of primary prevention in the form of lifestyle and dietary changes means that, in addition to enormously increasing pharmaceutical expenditures, these measures are largely ineffective because they are usually applied too late.5
The results of large prospective cohort studies based on “hard” clinical events (incident cases of cardiovascular disease, cancer, or diabetes mellitus [DM]) justify the recommendation for a healthy diet. These studies provide sufficient evidence that diets like the MedD prevent cardiovascular disease. Thus, the results of different meta-analyses indicate that a 2-point increase in adherence to a traditional MedD is associated with a significant reduction in total mortality (relative risk [RR]=0.92; 95% confidence interval [95%CI], 0.90-0.94), cardiovascular incidence or mortality (RR=0.90; 95%CI, 0.87-0.93), cancer incidence or mortality (RR=0.94; 95%CI, 0.92-0.96), and neurodegenerative diseases (RR=0.87; 95%CI, 0.81-0.94).6 Furthermore, a systematic review of the literature found that the MedD was the most likely nutritional candidate to have a protective effect on the cardiovascular system out of 32 candidate diets and healthy foods.7
However, although the current period is marked by evidence-based medicine, it is paradoxical that further reduction in the consumption of all fats, saturated and unsaturated, is advocated in many population dietary guidelines and in clinical practice as a paradigm of a healthy diet, as promoted by the US National Cholesterol Education Program. This remains the case despite the results of one of the most important clinical trials, the Women's Health Initiative Dietary Modification Trial.8 This clinical trial included 48 835 women who were randomly assigned to a low-fat diet (LFD) or control group and followed up for a mean of 8.1 years. The intervention focused on the use of complete dietary patterns. The result was not as expected. After observing 3445 major cardiovascular events, there was no evidence that an LFD significantly reduced the risk of coronary disease, stroke, and total cardiovascular disease, and so it follows that the key to cardiovascular risk reduction does not lie in a reduction of total fat intake. Thus, another paradigm of a “healthy diet”, such as a Mediterranean dietary pattern, required investigation. This dietary pattern is rich in vegetable oils and in theory is an excellent model of a healthy diet; it is much more palatable and easier to maintain over time. It is also worth recalling that a LFD may even be counterproductive. If fat intake is excessively reduced, the main energy source becomes carbohydrates, and diets rich in these carry an increased risk of insulin resistance and DM, which are two very important cardiovascular risk factors.
RANDOMIZED CLINICAL TRIALS OF NUTRITIONAL INTERVENTION USING A MEDITERRANEAN DIETFollowing observational studies, the next step in evidence-based medicine is to conduct randomized interventional studies, which provide the highest level of evidence possible. In this regard, it might be thought that the French Lyon Diet Heart Study9 had already demonstrated the effectiveness of this dietary pattern. However, despite being a randomized trial that has been widely cited, it suffered serious methodological limitations that restrict its usefulness as a basis for public health recommendations. These limitations are as follows: a) it only applies to secondary prevention, as it analyzed reinfarction and coronary deaths in patients who had already experienced a coronary event; b) the fat source employed (linolenic acid obtained from a canola-based margarine) was unusual and is not available to the general public; c) the control group's diet was richer in fat than that of the intervention group, and d) the sample size was small (14 observed endpoints in one group and 44 in another).
On the other hand, the PREDIMED trial,10 with a much larger sample than the Lyon study, analyzed MedD effects on the incidence of a composite endpoint that included cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke. The study included 7447 participants aged between 55 years and 80 years (men) and between 60 years and 80 years (women) without clinical manifestations of cardiovascular disease at the time of inclusion, but at a high risk of this disease due to having 3 or more risk factors or DM. They were randomly assigned to 3 groups: MedD supplemented with extra virgin olive oil (n=2487); MedD supplemented with nuts (n=2396); and a LFD (n=2349). All participants took part in individual and group sessions with a dietitian every 3 months and were evaluated every year. The study ended in late 2010 with a mean follow-up of 5 years.
All participants underwent a complete clinical examination at baseline, including blood pressure, weight, and waist circumference; they also completed a validated food frequency consumption questionnaire and a physical activity questionnaire. Subsequently, every 3 months, all participants underwent a personalized dietary intervention designed to increase adherence to the MedD or an LFD, depending on the group to which they had been assigned. With this aim, the 14-point MedD questionnaire proved very useful because the results formed the basis for personalized advice on changes the participant should make to acquire a traditional MedD or LFD dietary pattern. In the MedD+olive oil group, the goal was the daily consumption of over 40 g virgin olive oil; this is the average consumption that appears to confer a protective effect in countries with a low incidence of cardiovascular disease. The participants in the MedD+nuts group received 30g of nuts per day (15 g of walnuts and 7.5 g of hazelnuts and almonds). The olive oil was donated by the Patrimonio Comunal Olivarero de España (Spanish Olive Grove Authority), walnuts were provided by the California Walnut Commission, and hazelnuts and almonds by Morella Nuts SA and Borges SA, respectively. As there is evidence that foods rich in alpha-linolenic acid have a cardioprotective effect, walnuts were given in larger amounts because they contain high levels of this acid. Although short-term nutritional field studies have used a dose of 50 g/day or even more, an average intake of 30 g/day appears to be more acceptable for long-term consumption over a period of 4 to 6 years. The added beneficial effects of a long-term intake at comparable or lower doses probably account for the decreased risk of ischemic heart disease observed in epidemiological studies.11
The same measurements and examinations performed at the initial visit were repeated each year. The main objective of the study was to assess the effects of the MedD on a composite endpoint including cardiovascular death, myocardial infarction, and stroke. Secondary endpoints included the incidence of cancer, DM and all-cause death. The effects on blood pressure, weight gain, blood glucose, blood lipids, and systemic markers of cardiovascular disease were also evaluated.
MEDITERRANEAN DIET AND DIABETES MELLITUSAs DM is one of the epidemics of the 21st century, the effects of the MedD in preventing this disease were assessed. Thus, 418 nondiabetic participants were studied. At 5 years, the incidence of DM in the 3 study groups (MedD+olive oil, MedD+nuts, and LFD) was 10.1% (95%CI, 5.1-15.1), 11.0% (95%CI, 5.9-16.1), and 17.9% (95%CI, 11.4-24.4), respectively. The adjusted hazard ratios (aHR) were aHR=0.49 (95%CI, 0.25-0.97) and aHR=0.48 (95%CI, 0.24-0.96) in the MedD+olive oil and MedD+nuts group, respectively, compared to LFD. In other words, the incidence of DM in the 2 MedD groups decreased by 52% (95%CI, 27-86) compared to the LFD group. These changes were observed in the absence of variations in body weight and without significant changes in physical activity. Thus, a nutritional intervention based on the MedD appears to be a highly effective tool in the prevention of DM in subjects at high cardiovascular risk.12
MEDITERRANEAN DIET AND OTHER CARDIOVASCULAR RISK FACTORSAt the beginning of the PREDIMED trial, a pilot nutritional intervention study was conducted with 772 participants. After 3 months, the MedD+olive oil+nuts led to decreased blood pressure, improved blood lipids (increased high-density lipoprotein cholesterol and decreased low-density lipoprotein cholesterol), and decreased markers of inflammation associated with atherosclerosis.13 In addition, there was an increase in apolipoprotein (Apo) A1, a decrease in ApoB, and a decrease in the apoB/ApoA1 ratio. In subsequent studies, it was found that this intervention also decreased plasma levels of oxidized low-density lipoprotein cholesterol and other systemic markers of oxidation, as well as serum and cellular markers of inflammation associated with the onset and progression of arteriosclerosis. One year after the intervention, it was found that the MedD+olive oil or nuts, in addition to decreasing blood pressure in participants with hypertension, induced changes in lipid composition and the structural properties of erythrocyte membranes. There was also a decreased incidence of metabolic syndrome.14
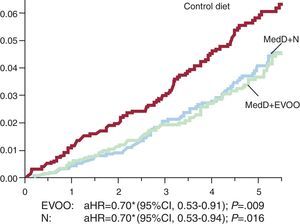
MEDITERRANEAN DIET AND THE INCIDENCE OF CARDIOVASCULAR COMPLICATIONSHaving observed the effects of the MedD intervention on all cardiovascular risk factors compared to the effect of an LFD, it would be reasonable to expect that this intervention would have a protective effect on the incidence of cardiovascular events. Indeed, this was demonstrated in another study15 in which the groups that followed the MedD supplemented with olive oil or nuts had an absolute risk reduction of about 3 major cardiovascular events per 1000 person/years, for a RR reduction of approximately 30%. Specifically, the group assigned to the MedD+olive oil and MedD+nuts groups had a aHR=0.70 (95%CI, 0.54-0.92) and aHR=0.72 (95%CI, 0.54-0.96), respectively, vs the control group (Fig. 2). The results of the PREDIMED study conclusively demonstrate the effect of the MedD in preventing cardiovascular disease.
Incidence of cardiovascular events in the 7447 PREDIMED study participants. Primary endpoint was a composite of cardiovascular death, myocardial infarction, and/or stroke. 95%CI, 95% confidence interval; aHR, adjusted hazard ratio; EVOO, extra virgin olive oil; MedD, Mediterranean diet; N, nuts. *Stratified by center (Cox model). Modified with permission from Estruch et al.15.
Given the demonstrated effectiveness of the MedD in preventing cardiovascular disease and its major risk factors, more attention should be devoted to lifestyle and dietary measures. Few drugs are able to match the 30% reduction in the incidence of major cardiovascular events achieved by an intervention with the MedD. Therefore, the implementation of a cardiovascular disease prevention program using a dietary intervention similar to that used in the PREDIMED study is recommended in medical practice. Dietitians and/or nurses could educate patients to follow a traditional MedD supplemented by an active intervention aimed at increasing physical activity. The more widespread use of lifestyle and dietary measures may not only decrease health costs, but could also lead to reductions in comorbidities and adverse drug effects.
CONFLICTS OF INTERESTNone declared.
SEE RELATED ARTICLE: http://dx.doi.org/10.1016/j.rec.2013.05.025

![Mediterranean Diet Pyramid Created by the Fundación Dieta Mediterránea de Barcelona (Mediterranean Diet Foundation of Barcelona [2010 edition]). s: serving. The use and promotion of this pyramid is recommended without any restriction. Reprinted with permission from Bach-Faig et al.4 Mediterranean Diet Pyramid Created by the Fundación Dieta Mediterránea de Barcelona (Mediterranean Diet Foundation of Barcelona [2010 edition]). s: serving. The use and promotion of this pyramid is recommended without any restriction. Reprinted with permission from Bach-Faig et al.4](https://static.elsevier.es/multimedia/18855857/0000006600000010/v1_201309220015/S1885585713001801/v1_201309220015/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6ImRPTHJMNGJ4SzkwZ2h1Y1ozUCs3emc9PSIsInZhbHVlIjoiY0ZCOVgyZ21ETDVyZ24vLzRnZHl4dEhnRmVpVzV5TXg5TXRuRUFVbDFQND0iLCJtYWMiOiI2ZjIyMmFhM2QxNTgwOGRkMGNmOTJmYWQyMjQ2NzgzMWU3ZmM5YWE3MTdmYjE1YmE5Mzk1ZDc0ODMzNzVhYmIwIiwidGFnIjoiIn0=)
