Myocardial injury after noncardiac surgery (MINS), the most frequent cardiovascular complication after a surgical intervention, has a major prognostic impact.1 Its effects can be powerfully illustrated using the following statistic: 1 in 10 patients with MINS will die within 30 days after surgery.2 Given that 200 million patients worldwide undergo noncardiac surgery every year3 and that the incidence of MINS varies between 15% and 18% according to the series consulted,4,5 MINS is one of the main conditions affecting mortality in this setting. This relatively “young” entity was defined for the first time by the researchers of the VISION study,6 which involved an international prospective cohort and evaluation of the major vascular complications in patients undergoing noncardiac surgery. They defined MINS as “all troponin elevations considered ischemic in origin, with prognostic relevance and occurring either during surgery or in the following 30 days”. The VISION study revealed that almost 85% of patients with MINS do not show symptoms compatible with myocardial ischemia and that about two-thirds have no detectable electrocardiographic changes. Accordingly, this complication is usually missed by clinicians. Consequently, both the universal definition of infarction7 and the main perioperative care guidelines now recommend the systematic and perioperative determination of troponin levels in patients with high cardiovascular risk.8,9
One of the most debated aspects, particularly within the cardiology community, is how patients with MINS should be managed. In terms of prevention, all attempts to extrapolate the robust advantages of drug therapies from nonsurgical cardiovascular medicine to the noncardiac surgery field have thus far failed. From the administration of beta-blockers10 to antiplatelet monotherapy,11 any hypothesized benefit has been rejected due to a lack of efficacy and even increases in severe postoperative complications such as stroke or bleeding. From the therapeutic point of view, no randomized studies have specifically attempted to answer this question. The available evidence has been observational and indicated that the use of aspirin and statins in patients who experience a perioperative infarction is associated with lower 30-day mortality.12 However, the results of the MANAGE study were recently published.13 This clinical trial is the first to attempt to determine whether administration of a direct anticoagulant (dabigatran) reduces the occurrence of cardiovascular complications in patients who experience MINS.
The MANAGE study is a multicenter, international clinical trial involving 84 hospitals in 19 countries around the world. The trial randomized 1754 patients in a factorial design to receive the following treatments for a maximum of 2 years or until the end of the study: dabigatran and omeprazole, dabigatran and placebo, placebo and omeprazole, or double placebo. The general hypothesis was that dabigatran would reduce cardiovascular complications and that omeprazole would minimize the risk of bleeding in patients who had undergone major noncardiac surgery and experienced MINS. Here, we report and discuss the results from the dabigatran group.
The inclusion criteria were as follows: patients aged ≥ 45 years who had undergone noncardiac surgery and met the universal definition of myocardial infarction valid at that time or had a postoperative troponin elevation with no explanation except myocardial ischemia (eg, sepsis, rapid atrial fibrillation, pulmonary embolism, or chronic troponin elevation).14 Notably, preoperative determination of troponin levels was not required because its measurement is not routine clinical practice.
In addition, individuals with a history of coagulopathy or major bleeding or requiring therapeutic anticoagulation (eg, those with a cardiac prosthesis) were excluded. Patients were also excluded if the following persisted beyond 35 days after MINS onset: the attending surgeon considered that anticoagulation initiation represented undue risk or a physician considered that the patient needed prophylactic-dose anticoagulation to avoid a thromboembolism due to insufficient physical measures; dual antiplatelet therapy was required or the estimated glomerular filtration rate was <35mL/min; and, finally, coronary angiography was considered necessary as a result of MINS.
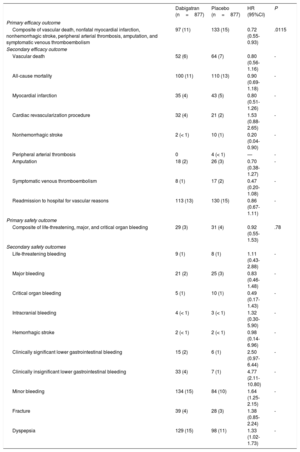
Once included, patients were randomized to receive dabigatran 110mg/twice daily or placebo. The primary efficacy outcome was a composite of vascular death, nonfatal myocardial infarction, nonhemorrhagic stroke, and peripheral arterial thrombosis. Given the low number of patients enrolled in the study, together with funding problems, the expected sample size (3200 patients) was reduced to 1750 patients. The protocol was performed in a blinded manner by an external committee, which added amputation and deep vein thrombosis to the initial composite outcome to maintain statistical power, based on the results of the COMPASS trial.15 The main safety outcome was a composite of life-threatening, critical organ, and major bleeding (defined as a hemoglobin drop of at least 4 points, the need for a transfusion of 3 or more units of red blood cells, or a percutaneous procedure or reoperation). Analyses were performed according to the intention-to-treat principle and the therapy was maintained for up to 2 years or until the end of the study.
Between January 2013 and June 2017, 1754 patients were included, 877 in each group; 90 came from Spain (Vall d’Hebron [45], Sant Pau [26], and Bellvitge [11] hospitals in Barcelona and Ramón y Cajal hospital in Madrid [8]). The typical clinical profile of a “MANAGE patient” was that of an individual aged about 70 years, whose reason for troponin elevation was mostly MINS (80% with an average troponin elevation of 82 ng/L vs 20% who met the infarction criteria), usually diagnosed within 48hours after surgery, and who could be randomized within the first 35 days after the MINS. Two-thirds were hypertensive, 25% were diabetic, almost 15% had a history of stroke, and 13% had a history of myocardial infarction. The most frequent surgery was orthopedic (38%), followed by general (28%) and vascular (14%). A mean 16-month follow-up was completed by 99% of the sample; the composite efficacy outcome was recorded in 97 patients (11%) in the dabigatran group vs 133 (15%) in the placebo group, giving a relative risk reduction of 28% (hazard ratio [HR]=0.72; 95% confidence interval [95%CI], 0.55-0.93; P=.0115). Although the disaggregated efficacy outcomes were also reduced in patients with dabigatran, the differences were not statistically significant (Table 1). The main safety outcome was observed in 29 patients (3%) in the dabigatran group vs 31 (4%) in the placebo group, indicating no significant risk difference (HR=0.92; 95%CI, 0.55-1.53; P=.78). However, there were significant increases in the incidences of minor bleeding, clinically insignificant lower gastrointestinal bleeding, and dyspepsia. During follow-up, 74% of patients (1296) also received antiplatelet monotherapy; 69% (1196), a statin; and 59% (1022), an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, with no significant differences between the 2 groups.
Efficacy and safety outcomes of the MANAGE study
| Dabigatran (n=877) | Placebo (n=877) | HR (95%CI) | P | |
|---|---|---|---|---|
| Primary efficacy outcome | ||||
| Composite of vascular death, nonfatal myocardial infarction, nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, and symptomatic venous thromboembolism | 97 (11) | 133 (15) | 0.72 (0.55-0.93) | .0115 |
| Secondary efficacy outcome | ||||
| Vascular death | 52 (6) | 64 (7) | 0.80 (0.56-1.16) | - |
| All-cause mortality | 100 (11) | 110 (13) | 0.90 (0.69-1.18) | - |
| Myocardial infarction | 35 (4) | 43 (5) | 0.80 (0.51-1.26) | - |
| Cardiac revascularization procedure | 32 (4) | 21 (2) | 1.53 (0.88-2.65) | - |
| Nonhemorrhagic stroke | 2 (< 1) | 10 (1) | 0.20 (0.04-0.90) | - |
| Peripheral arterial thrombosis | 0 | 4 (< 1) | — | - |
| Amputation | 18 (2) | 26 (3) | 0.70 (0.38-1.27) | - |
| Symptomatic venous thromboembolism | 8 (1) | 17 (2) | 0.47 (0.20-1.08) | - |
| Readmission to hospital for vascular reasons | 113 (13) | 130 (15) | 0.86 (0.67-1.11) | - |
| Primary safety outcome | ||||
| Composite of life-threatening, major, and critical organ bleeding | 29 (3) | 31 (4) | 0.92 (0.55-1.53) | .78 |
| Secondary safety outcomes | ||||
| Life-threatening bleeding | 9 (1) | 8 (1) | 1.11 (0.43-2.88) | - |
| Major bleeding | 21 (2) | 25 (3) | 0.83 (0.46-1.48) | - |
| Critical organ bleeding | 5 (1) | 10 (1) | 0.49 (0.17-1.43) | - |
| Intracranial bleeding | 4 (< 1) | 3 (< 1) | 1.32 (0.30-5.90) | - |
| Hemorrhagic stroke | 2 (< 1) | 2 (< 1) | 0.98 (0.14-6.96) | - |
| Clinically significant lower gastrointestinal bleeding | 15 (2) | 6 (1) | 2.50 (0.97-6.44) | - |
| Clinically insignificant lower gastrointestinal bleeding | 33 (4) | 7 (1) | 4.77 (2.11-10.80) | - |
| Minor bleeding | 134 (15) | 84 (10) | 1.64 (1.25-2.15) | - |
| Fracture | 39 (4) | 28 (3) | 1.38 (0.85-2.24) | - |
| Dyspepsia | 129 (15) | 98 (11) | 1.33 (1.02-1.73) | - |
95%CI, 95% confidence interval; HR, hazard ratio.
Data are expressed as No. (%).
Notably, 46% of the patients in the dabigatran group and 43% of those in the placebo group discontinued the study drug after a median of 80 days and 40 days, respectively, largely by patient request (56% and 60%, respectively).
The MANAGE study13 is thus far the first clinical trial designed to improve the prognosis of patients who experience MINS. The question now is whether we can directly apply the results of this study to our patients. The difficulties in reaching the expected sample size might indicate selection of the study population, as well as the high proportion of patients discontinuing treatment in both groups. We believe that both issues must be taken into account to correctly interpret the results. To maximize the statistical power, the researchers expanded the composite efficacy outcome, and significant statistical differences were detected in favor of dabigatran. It is also fair to point out that, nonetheless, the beneficial effects were maintained for both arterial and venous thrombotic events. In terms of the application of the MANAGE results,13 the authors acknowledge that, although no significant differences were detected in the composite safety outcome, dabigatran administration was associated with an increase in clinically insignificant bleeding (particularly gastrointestinal) and dyspepsia. Nonetheless, the definition of “minor” bleeding established by the authors was generous, and we believe that this point should also be taken into account when we apply the conclusions of the MANAGE study13 to our patients. It is possible that patients with high cardiovascular risk who undergo major surgery without relevant perioperative complications and with increased troponin levels during the first days will benefit the most from low doses of dabigatran after a careful evaluation of their bleeding risk.
The second major question that can be asked is how dabigatran modifies the prognosis of patients who have MINS. Based on the significant reduction in nonhemorrhagic stroke, some authors attribute the benefits to the early administration of anticoagulation therapy to patients with undetected paroxysmal atrial fibrillation.16 This hypothesis highlights the substantial gap in pathophysiological knowledge about the ultimate mechanisms underlying MINS. Classically, the pathophysiology of perioperative myocardial infarction can involve 2 potential pathways17: the first is the formation of a thrombus in the coronary artery due to the inflammatory state and hypercoagulability induced by the surgical stress and tissue injury; the second mechanism results from an imbalance between myocardial oxygen supply and demand. On the one hand, the physiological response to surgical stress, which may persist for days after the intervention, increases oxygen consumption and, on the other, relatively common events during surgery and the postoperative period, such as hypotension, anemia, hypoxia, and hypovolemia, decrease oxygen supply. However, the VISION6 and MANAGE13 studies remind us that most postoperative troponin elevations do not meet infarction criteria and are asymptomatic; consequently, they do not usually lead to careful cardiological assessment. Thus, clarification of the ultimate causes underlying MINS is certain to help to establish preventive, diagnostic, and therapeutic measures to improve prognosis in this population. The findings of the MANAGE study13 indicate that the prevailing pathophysiology may be more “thrombotic” (whether atherosclerotic or embolic) than a supply/demand mismatch. Our group, in collaboration with Vall d’Hebron Hospital, is performing a study (Perioperative Myocardial Ischemia: Troponin Monitoring, Cost-effectiveness, Insights Into Pathophysiology [PMI], NCT03438448) specifically designed to assess the mechanisms underlying the development of MINS in these patients. The work involves the systematic performance of a clinical cardiological assessment and is supported by a complete advanced cardiac imaging study with coronary computed tomography and magnetic resonance imaging.
Ultimately, the MANAGE study13 should be a wake-up call that jolts the cardiological community into actively addressing this frequent clinical entity with a major prognostic impact. In addition, its results provide valuable clues to the physiopathological mechanisms of MINS and an opportunity to consider how to improve the prognosis of patients who experience this heretofore largely unnoticed and poorly managed complication.
CONFLICTS OF INTERESTThe authors are researchers from the MANAGE study in Spain and declare that they have received funding to attend study meetings.