Patients presenting with chest pain or other symptoms consistent with myocardial ischemia are a common problem throughout the world. In the United States alone, there are over 8 million visits to the emergency department (ED) for chest pain annually, such that it is the second most frequent cause of adult ED visits.1 The presence of hemodynamic stability or ischemic electrocardiogram (ECG) changes identifies a high risk cohort; in the absence of these, the majority of the remaining patients are at lower risk for an acute coronary syndrome (ACS), and can be further risk stratified based on symptoms and history of coronary disease. The challenge to clinicians is rapidly and accurately identifying patients from this group who actually have unsuspected ACS. Failure to detect ACS patients can lead to inadvertent ED discharge, a situation associated with significantly increased morbidity and mortality, with resultant substantial liability.2
In an effort to improve risk stratification and identification of ACS and other serious conditions in the ED, a wide array of new imaging techniques have been applied, each with potential advantages and disadvantages. With all of these modalities, clinical judgment is essential for optimal application and interpretation.
The simplest test for evaluating chest pain patients is the exercise treadmill test without imaging. Although very early exercise stress testing (ETT), prior to complete exclusion of myocardial infarction (MI), has been applied in some centers successfully,3,4 most would be reluctant to exercise a patient without serial markers and symptom resolution. Additional limitations of an ETT alone strategy include baseline ECG changes precluding the ability to interpret the ECG, and exercise tolerance insufficient to exclude ischemia with high confidence.
In contrast to ETT, acute imaging is typically applied to patients with and without ongoing symptoms, frequently with only one set of cardiac markers. Advantages of acute imaging include more effective triage and disposition, such that high risk patients are rapidly identified, allowing early treatment initiation and admission, while low risk patients can be discharged quickly. If accurately applied, costs should be reduced through improved efficiency. Techniques that have been used include rest echocardiography, rest myocardial perfusion imaging (MPI), computed tomographic angiography (CTA) of the coronary arteries, and to a lesser extent, cardiac magnetic resonance imaging (cMRI).
EchocardiographyEchocardiography was one of the first imaging tools applied to acute chest pain patients.5 Because regional wall motion abnormalities induced by ischemia are detected by echocardiography almost immediately after their onset, they proceed ECG alterations and symptoms and offer the potential for rapid diagnosis.6 Diagnostic accuracy of acute echocardiography for detection of ACS has varied, although most studies have found a high sensitivity and negative predictive value.5,7,8 Similar to rest MPI, a finite amount of myocardium must be ischemic before wall motion abnormalities can be detected. In comparative studies, diagnostic accuracy for echocardiography was similar to rest MPI;9 however, it is more logistically difficult to perform, which limits its use on a routine basis.
Other variables affecting sensitivity include the timing of the study in relation to symptoms and image quality. Imaging technology, especially the introduction of harmonic imaging, has advanced significantly since initial studies were performed. Image quality can be further improved by the use of myocardial contrast agents, which improve left ventricular opacification, decreasing the number of suboptimal studies. Echocardiographic contrast can also be used to assess myocardial perfusion. After intravenous injection, the contrast agent is taken up by the myocardium in proportion to regional coronary blood flow, with areas of significant stenosis demonstrating inadequate perfusion.8 Limited studies, performed primarily in single centers with expertise, have demonstrated increased sensitivity for detection of ischemia compared to rest echocardiography alone.8 Because this technique is technically demanding, it is likely to achieve only limited use in the near future.
Acute Rest Myocardial Perfusion ImagingThe development and wide-spread use of the technetium agents in the 1990s led to use of acute rest MPI for ED chest pain evaluation. The technetium agents do not redistribute, so that patients can be injected during symptoms and imaged 1–4h later, with the images representing a “snap shot” of blood flow at the time of injection. Normal perfusion is associated with very low clinical risk, so that patients can be discharged with further outpatient rest/stress MPI, if indicated.10 Simultaneous assessment of wall motion is obtained, so that perfusion defects resulting from artifacts or soft tissue attenuation can be differentiated from those occurring as a result of ischemia.11 Left ventricular ejection fraction can be calculated, providing quantitative determination of systolic function.
Numerous studies have demonstrated that rest MPI can accurately identify low and high risk patients.10,11,12 Importantly, in an era of cost containment, rest MPI significantly increases both diagnostic and prognostic information beyond that of the ECG and clinical variables. These advantages were confirmed in a prospective multicenter trial of 2,475 patients who presented to the ED with chest pain and non-ischemic ECG12 in which a strategy of performing rest MPI in conjunction with clinical assessment was compared to usual care alone. The sensitivity of the two strategies for identifying patients with ACS was similar (96% and 97%, respectively) but patients in the MPI arm had a significantly lower hospitalization rate (42% vs. 52%, p<0.01) which translated into an estimated savings of $70 per patient. In addition to decreased admission, other mechanisms of cost reduction include better selection of patients for further diagnostic procedures, with reduced rates of coronary angiography in low risk patients.10 Given the substantial evidence, rest MPI has a class 1 indication from the ACC/AHA for evaluating patients with a non-ischemic ECG.
Acute rest MPI has several limitations. A perfusion defect can result from acute ischemia, acute MI or old MI; the first two represent a high risk state which requires admission. To differentiate prior infarction from ischemia, repeat imaging during a pain-free state can be performed. Resolution of a perfusion defect indicates that the initial defect was secondary to acute ischemia; if the defect persists, prior MI is more likely. Another limitation is that small areas of ischemic myocardium (3–5% of the left ventricle) may not be detected. Therefore, optimal use is typically in conjunction with at least one set of cardiac injury markers, which offer complementary information to MPI. The availability of imaging during all hours may be logistically difficult. A potential solution was demonstrated in one study in which patients presenting from 12 midnight to 6 am were injected with isotope and imaged first thing in the morning; they found no difference in diagnostic accuracy.13
Computed Tomographic AngiographyUnlike ETT, MPI, and echocardiography, CTA provides anatomic rather than functional information regarding coronary anatomy. Feasibility and diagnostic accuracy have improved as 64-slice multidetector CT (computed tomography) scanners have become routine. Current systems afford clear visualization of the major coronary arteries and branch vessels, with spatial resolution that approaches but still remains less than that of conventional angiography. Newer 128 and even 320 slice scanners are being tested, which can decrease imaging time with improved accuracy, albeit at a cost of increased radiation.
A number of studies have explored the utility of CTA in low risk ED chest pain populations with the goal of determining the utility of this triage method. Initial small studies, followed by larger single center studies, have shown that CTA is promising. In a randomized trial of early CTA compared to standard care (rule out protocol followed by stress MPI), CTA decreased time to diagnosis (15.0 vs. 3.4 h), and was associated with fewer repeat evaluations for chest pain and lower cost14. However, 46% of patients initially screened were not eligible for CTA, patients in the CTA arm were significantly more likely to undergo coronary angiography, and 24% required subsequent stress MPI to assess intermediate coronary lesions.12
Based on initial information that grows substantially each year, CTA has the potential to impact significantly on the triage of selected low to intermediate risk patients presenting to the ED with chest pain. Obstructive coronary artery disease (CAD) can be excluded reliably in many patients, and discharge from the ED following a normal or non-obstructive CTA appears safe.12
Like all imaging techniques, limitations of CTA need to be considered. Current protocols typically require acquisition of data over 10–20seconds during breath holding while contrast is injected (approximately 80ml). As noted above, as many as 45–50% of patients presenting to the ED with chest pain may not be candidates for this technique because of obesity, contrast allergy, intolerance to β-blockade that is required to decrease heart rate for optimal resolution, arrhythmia, renal insufficiency, or history of CAD. A significant minority will have suboptimal coronary artery visualization, coronary calcium that obscures vessels, or moderate stenosis; this typically requires further non-invasive evaluation in approximately 25% of patients.14
Although it is non-invasive, there are risks associated with CTA, including allergy to iodinated contrast medium and the risk from radiation exposure. The average radiation dose of a 64-slice CTA varies widely depending on sex, body size, imaging protocol and scanner type. Radiation exposure is similar to or higher than rest-stress Tc-99m MPI,15 depending on variables noted above; however, the effective dose to breast and lung tissue is roughly 3-fold higher, increasing the estimated lifetime attributable risk of malignancies to these tissues, particularly in younger female patients.16
The concern about radiation with coronary CTA has led to progressive advances that have substantially reduced radiation exposure without affecting image quality. However, given the potential long-term cancer risk, CTA is less appropriate in the younger, particularly female, patient. There is also the concern that wide-spread use will lead to inappropriate coronary angiography in patients who have intermediate stenoses that are not related to symptoms. Thus, larger, multi-center studies are required to demonstrate its cost effectiveness before this technology can be considered widely applicable.
Cardiac Magnetic Resonance ImagingUse of cMRI for chest pain assessment is similar to rest MPI, as it can provide information on perfusion and function, but a much higher image resolution than MPI. In addition, cardiac morphology is obtained, and stress imaging can be performed in the same setting. These advantages indicate its potential; however, cMRI has the least data on acute chest pain evaluation. A recent single center randomized trial found that a strategy of early rest/stress cMRI was associated with significant cost reductions compared to standard care.17 Important limitations/contraindications to cMRI include prior pacemaker or intra-cardiac defibrillator placement, and significant claustrophobia (seen in about 5% of patients). Given its limited availability, its use will likely be limited to centers with large volumes of patients, with expertise in cMRI, and require the development of specific institutional protocols.
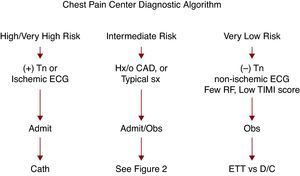
Appropriate UtilizationA potential strategy for incorporating imaging in the chest pain evaluation process is outlined in Figure 1, Figure 2. Patients who are high risk (ischemic ECG, (+) initial troponin) are admitted (Figure 1). Very low risk patients (absence of ischemic ECG changes, atypical chest pain, and other factors defining low risk) who have a good exercise tolerance and an ECG that is either normal or has only minor, non-specific changes, would undergo a rapid MI exclusion protocol (Figure 1). With more sensitive troponins, that likely can be accomplished within 3h after presentation. If negative, early ETT is performed or the patient is directly discharged from the ED.
Figure 1. Proposed diagnostic algorithm for chest pain patients. CAD, coronary artery disease; Cath, catheterization; ECG, electrocardiogram; ETT, exercise stress test; D/C, discharge; obs, observation; RF, risk factors; sx, symptoms; TIMI, thrombolysis in myocardial infarction; Tn, troponin.
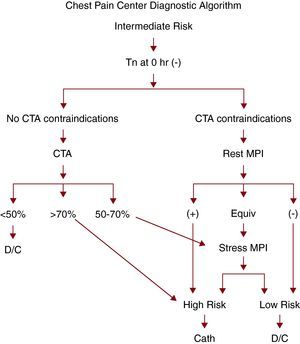
Figure 2. Proposed diagnostic algorithm for intermediate chest pain patients. Cath, catheterization; Equiv, equivocal; MPI, myocardial perfusion imaging; CTA, computed tomographic angiography; MPI, myocardial perfusion imaging; D/C, discharge; Tn, troponin.
For intermediate risk chest pain patients (more prolonged typical chest pain, history of coronary disease, inability to exercise), imaging is performed as part of the acute evaluation (Figure 2). First, the patient is assessed for contraindications to CTA. These include those noted above, as well as a history of coronary disease, and older age (due to likely concomitant asymptomatic CAD or extensive coronary calcium). If none are present, CTA is performed. For those who have contraindications to CTA, acute rest MPI is performed as an alternative imaging choice. Further evaluation is dependent on the results of imaging. It should be emphasized the success of such a protocol is dependent on accurate initial risk stratification using the initial ECG and presenting symptoms.
ConclusionsAcute imaging in the low risk chest pain patient has promise for better risk stratification of patients, potentially reducing costs while decreasing missed MI. No one test will be appropriate for all patients, and the choice will be dependent on an institution's logistical capabilities and expertise. To date, current studies are limited to primarily observational data, with few randomized trial data available. An important consideration when evaluating any new imaging technique is that diagnostic accuracy is no longer sufficient to demonstrate a test's utility; instead, improving clinical outcomes is required. Further studies, preferably randomized trials that are focused on patient centered outcomes, will be necessary to better identify which, if any, of the advanced imaging techniques are appropriate for the evaluation of low risk chest pain patients.
Conflict of interestDr. Kontos has received research funding from Bracco and serves as a consultant to Molecular Pharmaceuticals, Inc.
Corresponding author: Room 285 Gateway Building, Second Floor. PO Box 980051, 1200 E Marshall St, Richmond, VA 23298-0051, USA. mkontos@mcvh-vcu.edu