More than one-third of patients with ST-segment elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI) have significant coronary lesions in vessels other than the infarct-related artery.1–3 These patients have a worse prognosis, including a two-fold higher risk of mortality compared with patients with single-vessel disease. This higher mortality may be due to a number of factors, including a worse clinical risk profile, with more diabetes and previous infarction, and a higher incidence of heart failure, cardiogenic shock, and mechanical complications.1,2
It has been known for several years that PCI improves symptoms and reduces revascularization rates compared with medical therapy in patients with coronary artery disease. What is less well established is whether PCI reduces the hard endpoints of death or myocardial infarction (MI).4 The article by Galvão Braga et al. published in Revista Española de Cardiología is an insightful observational study evaluating whether patients with STEMI and multivessel disease should undergo culprit-only or complete revascularization with PCI.5 Their study suggests that complete revascularization improves clinical outcomes, with reduced long-term mortality. One strength of this study is the long-term follow-up of patients, during which time the benefits of complete revascularization would be more likely to emerge.
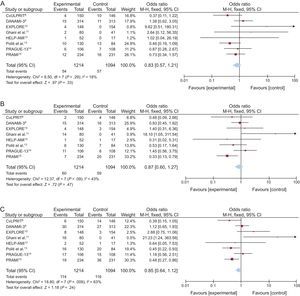
The question is whether the study by Galvão Braga et al. should change our clinical practice or the way we view nonculprit lesion PCI. The rationale for nonculprit lesion PCI in patients with STEMI and multivessel disease is that it will reduce events that may be related to plaque rupture at the site of the nonculprit lesion.6 Some have argued that there is pan-coronary inflammation and that PCI may help to stabilize nonculprit lesions, relieve ischemia, and improve the contractility of the myocardium subtended by these lesions.7 Although there is some evidence to support these mechanisms, there are limited data from randomized trials. To date, 8 randomized trials have compared culprit-only and complete revascularization in patients with STEMI and multivessel disease (Figure). Several meta-analyses have shown that complete revascularization reduces the incidence of major adverse cardiovascular events, mostly by reducing the need for repeat (urgent, nonurgent, or ischemia-driven) revascularization. A reduction in mortality or MI has not been clearly demonstrated.16–18 Although some of the individual trials have suggested a benefit on death or MI,8–15 others have shown absolutely no benefit on these outcomes.9,10,14
Thus, the observational study by Galvão Braga et al. is of interest because it suggests that a staged complete revascularization strategy may reduce major adverse cardiovascular events and, importantly, mortality. However, because it is a single-center, retrospective, nonrandomized observational study with a relatively small number of patients and events, we have to interpret these findings cautiously.5 Although these data may agree with the perceptions of many on the value of complete revascularization, the data would best be viewed as hypothesis generating.
The ongoing COMPLETE trial will help to clarify whether we should treat only the culprit-vessel or all significant coronary stenoses.19 This study has several key characteristics. First, it was designed to be powered to detect modest, but clinically important, differences in hard outcomes, including the composite of cardiovascular death or MI and the composite of cardiovascular death, MI or ischemia-driven revascularization (co-primary outcomes). Second, follow-up will be for several years in order to detect a potential long-term clinical benefit of complete revascularization. Third, it is a contemporary trial with high rates of use of newer generation antiplatelet drugs, drug-eluting coronary stents, and fractional flow reserve for intermediate lesions. Until the results of the COMPLETE trial are known, it is recommended that physicians individualize the care of these patients by optimizing medical management and thoughtfully balancing the potential benefits and risks of a nonculprit lesion PCI strategy.
CONFLICTS OF INTERESTNone declared.