A paradoxical protective effect of obesity has been previously reported in patients with atrial fibrillation (AF). The aim of this study was to determine the impact of nutritional status and body mass index (BMI) on the prognosis of AF patients.
MethodsWe conducted a retrospective population-based cohort study of patients with AF from 2014 to 2017 from a single health area in Spain. The CONUT score was used to assess nutritional status. Cox regression models were used to estimate the association of BMI and CONUT score with mortality. The association with embolism and bleeding was assessed by a competing risk analysis.
ResultsAmong 14 849 AF patients, overweight and obesity were observed in 42.6% and 46.0%, respectively, while malnutrition was observed in 34.3%. During a mean follow-up of 4.4 years, 3335 patients died, 984 patients had a stroke or systemic embolism, and 1317 had a major bleeding event. On univariate analysis, BMI was inversely associated with mortality, embolism, and bleeding; however, this association was lost after adjustment by age, sex, comorbidities, and CONUT score (HR for composite endpoint, 0.98; 95%CI, 0.95-1.01; P=.719). Neither obesity nor overweight were predictors of mortality, embolism, and bleeding events. In contrast, nutritional status—assessed by the CONUT score—was associated with mortality, embolism and bleeding after multivariate analysis (HR for composite endpoint, 1.15; 95%CI, 1.14-1.17; P<.001).
ConclusionsBMI was not an independent predictor of events in patients with AF in contrast to nutritional status, which showed a strong association with mortality, embolism, and bleeding.
The study was registered at ClinicalTrials.gov (Identifier: NCT04364516).
Keywords
Obesity and malnutrition are major health problems worldwide.1,2 The World Health Organization has listed both obesity and malnutrition among its top 10 causes of global mortality and disease.3 Obesity is an imbalance of calories, whereas malnutrition is an imbalance of nutrients.4
Obesity, which is epidemic in high-income countries, is well established as an independent risk factor for all-cause and cardiovascular mortality in the general population.5,6 However, among patients with certain established cardiovascular conditions, overweight and obesity are associated with a lower risk of death—a phenomenon known as the “obesity paradox”.7,8 A possible explanation is that when chronic cardiovascular disease develops, the body becomes catabolic and requires greater energy and calorie reserves than usual.9 However, if patients lack sufficient nutritional status, they may become malnourished despite their normal or high body mass index.10
In the setting of atrial fibrillation (AF), an increased body mass index (BMI) has been independently associated with a lower risk of stroke/systemic embolic events (SEE) and better survival.7 However, knowledge about the prognostic impact of nutritional status is scarce.11 To clarify the impact of nutritional status on the relationship between BMI and mortality and clinical outcomes in AF patients, we designed this community study in a large population of unselected AF patients.
METHODSData sourcesThe CardioCHUVI-AF registry (formerly known as Registry of Atrial Fibrillation of Vigo, Spain) is a retrospective community study of patients with AF.12 The medical records of all patients were reviewed, and AF diagnosis was confirmed by the presence of a compatible electrocardiogram. Clinical, laboratory and therapeutic data were collected in an encoded database. The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the local ethics committee (Autonomous Committee of Research Ethics of Vigo, code HAC-ACO-2018-01, registry 2018/258). Due to the retrospective nature of the study, informed consent was not required. The CardioCHUVI-AF registry is registered in ClinicalTrials.gov with the identifier NCT04364516
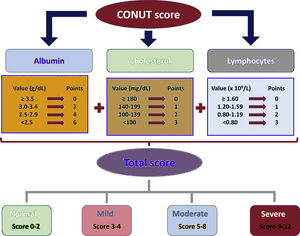
Study populationAll consecutive patients with a confirmed diagnosis of AF between January 2014 and January 2018 in the health area of Vigo (Galicia, Spain) were included (n=16 203). We excluded patients with missing baseline and follow-up data (n=146), and without data on weight/height (n=429) or nutritional status (n=779). The final cohort was composed of 14 849 AF patients. Patients were classified according to BMI in 4 groups: underweight (< 18.5kg/m2), normal weight (18.5-24.9kg/m2), overweight (25-29.9kg/m2), and obesity (≥ 30kg/m2). Subsequently, patients were classified according to nutritional status. For this purpose, the Controlling Nutritional Status (CONUT) score was employed.13 The score is derived from the values of serum albumin, total cholesterol, and lymphocyte counts. Albumin represents protein reserves, total cholesterol represents calorie depletion, and lymphocyte count represents immune defense. The CONUT score was calculated according to the original study (figure 1). This score has been used due to its simplicity and its prognostic validation in inpatients and outpatients with other cardiovascular diseases.14,15 A score of 0 to 1 was considered normal; scores of 2 to 4, 5 to 8, and 9 to 12 reflected mild, moderate, and severe malnutrition, respectively. Details of the creation of the cohort are shown in the supplementary data ().
OutcomesThe primary outcome was all-cause mortality during follow-up, while the secondary outcome was embolic and hemorrhagic events. Embolic events included ischemic stroke and SEE, defined according to cardiovascular and stroke endpoint definitions for clinical trials performed by the Standardized Data Collection for Cardiovascular Trials Initiative (SCTI) and the US Food and Drug Administration.16 Hemorrhagic events included major bleeding, defined according to the statement of the International Society on Thrombosis and Haemostasis.17 Two data managers independently reviewed the clinical history of each patient to identify events. All suspected events were independently reviewed by 2 specialists in the clinically relevant areas of cardiology and internal medicine. Both data managers and specialists underwent a study-specific training course on event definitions and the adjudication process. Finally, an independent clinical events committee revised and adjudicated all events.
Statistical analysesContinuous data are presented as the mean ±standard deviation and were compared using unpaired t tests. Categorical data are presented as counts (proportions) and were compared using chi-square tests. The incidences of all-cause mortality, embolic and hemorrhagic events were estimated using Kaplan-Meier curves. We used Cox proportional hazard regression models to estimate the association with all-cause mortality. For stroke/SEE and major bleeding, death served as a competing risk. Therefore, the incidence of each outcome was estimated using weighted cumulative incidence curves after the use of the Fine-Gray proportional subdistributions hazards model. The proportionality assumption was verified by testing for an interaction between the exposure variable and time, and no relevant violations were found. Three multivariate models were performed: a) adjusted for age and sex; b) adjusted for age, sex, statin therapy, anticoagulation therapy, Charlson index,18 HAS-BLED score,19 and CHA2DS2-VASc20 score; c) the same as model 2 but adding the CONUT score or BMI, as appropriate. Effect estimates from Cox models were reported as hazard ratios (HRs) while those from Fine-Gray models were reported as subdistribution HRs along with 95% confidence intervals (95%CIs).
Statistical analyses were conducted using STATA software, version 15 (Stata Corp, College Station, United States). A 2-sided P<.05 was considered statistically significant.
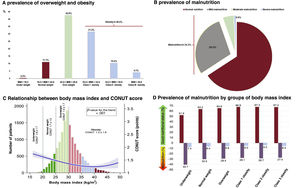
RESULTSStudy cohortA total of 14 849 patients (75.6 ±10.3 years, 50.9% women) were followed up for 4.4 ±1.8 years. The mean BMI value was 30.3±4.8, with overweight and obesity observed in 42.6% and 46.0%, respectively (figure 2A). The mean CONUT score was 1.4±1.7, with mild and moderate/severe malnutrition observed in 29.0% and 5.3%, respectively (figure 2B). The baseline characteristics of the study population and differences according to nutritional status and BMI are summarized in the supplementary data ().
Distribution of the study population according to body mass index (BMI) and nutritional status. Prevalence of overweight and obesity (A), and prevalence of malnutrition (B). The relationship between the CONUT score and BMI (C). The rate of malnutrition according to BMI groups (D).
As BMI increased, the CONUT score tended to decrease, but the relationship was not linear (figure 2C). Malnutrition rates were lower as BMI increased: from 48.1% in patients with underweight, to 36.8%, 35.1% and 33.0% in patients with normal weight, overweight, and obesity, respectively (P<.001 for trend; figure 2D).
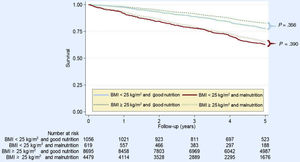
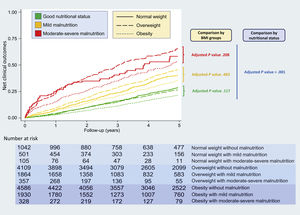
Body mass index, nutritional status, and mortalityDuring the follow-up, 3335 patients died (5.1 per 100 patients/y). The association between BMI and CONUT score with outcomes is detailed in table 1 and table 2. BMI was inversely associated with mortality (HR per 5kg/m2 0.76; 95%CI, 0.68-0.86; P<.001) in the univariate analysis; however, after various multivariate analyses including the CONUT score, BMI was not an independent predictor of mortality (table 1). The mortality rate was lower in patients with BMI ≥ 25kg/m2 (5.0 deaths per 100 patients/y) compared with those with BMI<25kg/m2 (6.2 deaths per 100 patients/y). However, when we adjusted for the presence of malnutrition (figure 3), those differences disappeared (HR for mortality comparing BMI ≥ vs <25kg/m2 [HR 0.97, 95%CI, 0.92-1.02; P=.176]. Neither obesity (HR, 0.91; 95%CI, 0.81-1.01; P=.088) nor overweight (HR, 1.04; 95%CI, 0.94-1.16; P=.438) were predictors of mortality in the multivariate analysis adjusted for nutritional status. The prognostic impact of overweight and obesity in patients with normal nutrition, mild malnutrition, and moderate-severe malnutrition is shown in figure 4a and . Regarding nutritional status, both mild and moderate-severe malnutrition were associated with higher mortality in all BMI groups (normal weight, overweight, and obesity) (). In patients with moderate-severe malnutrition, BMI was inversely associated with mortality, but not in those with mild or absent malnutrition (). However, we did not find statistical significance for the association between BMI and mortality after adjusting for age, sex, comorbidities and moderate-severe malnutrition (). The association between BMI and the CONUT score with mortality and composite endpoint (mortality, stroke/SEE and/or major bleeding) was maintained in various clinical subgroups ().
Univariate and multivariate analyses for mortality and clinical outcomes according to body mass index.
| Event | Analysis | BMI (per 5 kg/m2) | Discrimination C-index | ||
|---|---|---|---|---|---|
| HR | 95%CI | P | |||
| All-cause mortality | Univariate | 0.81 | 0.78-0.84 | <.001 | 0.561 |
| Adjusted only by CONUT | 0.98 | 0.94-1.02 | .278 | 0.758 | |
| Multivariate 1 | 0.97 | 0.94-1.01 | .208 | 0.728 | |
| Multivariate 2 | 0.96 | 0.92-1.00 | .048 | 0.754 | |
| Multivariate 3 | 0.97 | 0.93-1.01 | .117 | 0.774 | |
| Stroke/SEE | Univariate | 0.87 | 0.81-0.93 | <.001 | 0.547 |
| Adjusted only by CONUT | 0.93 | 0.87-1.00 | .052 | 0.637 | |
| Multivariate 1 | 0.93 | 0.87-0.99 | .044 | 0.574 | |
| Multivariate 2 | 0.91 | 0.85-0.98 | .011 | 0.594 | |
| Multivariate 3 | 0.92 | 0.85-0.98 | .017 | 0.652 | |
| Bleeding | Univariate | 0.94 | 0.88-0.99 | .021 | 0.514 |
| Adjusted only by CONUT | 1.00 | 0.94-1.06 | .902 | 0.615 | |
| Multivariate 1 | 0.99 | 0.94-1.05 | .848 | 0.541 | |
| Multivariate 2 | 0.94 | 0.89-1.01 | .054 | 0.604 | |
| Multivariate 3 | 0.95 | 0.89-1.01 | .086 | 0.654 | |
| Univariate | 0.87 | 0.84-0.90 | <.001 | 0.543 | |
| Adjusted only by CONUT | 0.99 | 0.96-1.03 | .792 | 0.703 | |
| Composite endpoint | Multivariate 1 | 0.99 | 0.96-1.02 | .628 | 0.671 |
| Multivariate 2 | 0.97 | 0.94-1.01 | .087 | 0.696 | |
| Multivariate 3 | 0.98 | 0.95-1.01 | .223 | 0.719 | |
95%CI, 95% confidence interval; BMI, body mass index; CONUT, Controlling Nutritional Status; HR, hazard ratio; SEE, systemic embolic event
Multivariate 1: adjustment by age and sex.
Multivariate 2: adjustment by age, sex, CHA2DS2-VASc score, HAS-BLED score, Charlson comorbidity index, anticoagulation therapy, and statin therapy.
Multivariate 3: adjustment equal as Multivariate Model 2 plus CONUT score.
Univariate and multivariate analysis for mortality and clinical outcomes according to CONUT score.
| Event | Analysis | CONUT (per 1 point) | Discrimination C-index | ||
|---|---|---|---|---|---|
| HR | 95%CI | P | |||
| All-cause mortality | Univariate | 1.26 | 1.24-1.28 | <.001 | 0.631 |
| Adjusted for BMI | 1.21 | 1.19-1.23 | <.001 | 0.758 | |
| Multivariate 1 | 1.21 | 1.19-1.23 | <.001 | 0.743 | |
| Multivariate 2 | 1.17 | 1.15-1.19 | <.001 | 0.763 | |
| Multivariate 3 | 1.17 | 1.15-1.19 | <.001 | 0.774 | |
| Stroke/SEE | Univariate | 1.13 | 1.09-1.17 | <.001 | 0.558 |
| Adjusted for BMI | 1.10 | 1.07-1-14 | <.001 | 0.637 | |
| Multivariate 1 | 1.10 | 1.06-1.14 | <.001 | 0.574 | |
| Multivariate 2 | 1.08 | 1.05-1.13 | <.001 | 0.592 | |
| Multivariate 3 | 1.09 | 1.05-1.13 | <.001 | 0.652 | |
| Bleeding | Univariate | 1.17 | 1.14-1.20 | <.001 | 0.586 |
| Adjusted for BMI | 1.15 | 1.11-1.18 | <.001 | 0.615 | |
| Multivariate 1 | 1.14 | 1.11-1.18 | <.001 | 0.592 | |
| Multivariate 2 | 1.11 | 1.08-1.15 | <.001 | 0.608 | |
| Multivariate 3 | 1.11 | 1.06-1.17 | <.001 | 0.654 | |
| Univariate | 1.23 | 1.21-1.25 | <.001 | 0.611 | |
| Adjusted for BMI | 1.19 | 1.17-1.21 | <.001 | 0.703 | |
| Net outcome | Multivariate 1 | 1.19 | 1.17-1.20 | <.001 | 0.688 |
| Multivariate 2 | 1.15 | 1.14-1.17 | <.001 | 0.706 | |
| Multivariate 3 | 1.15 | 1.14-1.17 | <.001 | 0.719 | |
95%CI, 95% confidence interval; BMI, body mass index; CONUT, Controlling Nutritional Status; HR, hazard ratio; SEE, systemic embolic event.
Multivariate 1: adjustment by age and sex.
Multivariate 2: adjustment by age, sex, CHA2DS2-VASc score, HAS-BLED score, Charlson comorbidity index, anticoagulation therapy, and statin therapy.
Multivariate 3: adjustment equal as Multivariate Model 2 plus body mass index.
Prognostic impact of overweight/obesity and malnutrition nutritional status. A: the risk of mortality and clinical outcomes for overweight/obesity according to nutritional status. B: the risk of mortality and clinical outcomes for malnutrition according to body mass index (BMI) groups. In view of small sample size (n=27), patients with underweight (body mass index <18.5kg/m2) were excluded from these analyses. 95%CI, 95% confidence interval; SEE, systemic embolic event.
A total of 984 patients had a stroke/SEE during follow-up, and 1317 had a major bleeding event. After we stratified by groups according to nutritional status (good nutrition, mild malnutrition, and moderate-severe malnutrition), neither overweight nor obesity were associated with embolic and hemorrhagic outcomes (figure 5). After various multivariate analyses including age, sex, comorbidities, and nutritional status, BMI was not associated with composite endpoint (mortality, stroke/SEE and/or major bleeding), in contrast with the CONUT score (table 1 and table 2).
DISCUSSIONIn this real-world observational study, we assessed the impact of nutritional status on the association between BMI and the prognosis of AF patients. We report 4 main findings: a) malnutrition is common in AF patients, even in those with overweight and obesity; b) malnutrition is a strong predictor of mortality in patients with AF; c) after adjustment for age, sex, comorbidities, and nutritional status, BMI was not associated with worse prognosis; d) the mortality rate in patients with overweight and obesity was similar to that patients with normal weight.
Malnutrition is systematically underdiagnosed in AF patients, and is therefore a long way from being corrected.21 Although impressions might be lower, 1 in 3 patients in our study had some degree of malnutrition. The work of physicians, nurses or dietitians is important in this field and could represent an invaluable tool for improving the quality of care given to AF patients. Moreover, in overweight and obese patients, the rate of malnutrition was also high, 35.1% and 33.0%, respectively. This conveys an important clear message: obesity and malnutrition are not mutually exclusive. This leads us to the concept of the double burden of malnutrition now facing many countries worldwide, characterized by the coexistence of undernutrition along with overweight or obesity.4
There are few data on malnourished AF individuals or on the relationship between malnutrition and medium-to long-term mortality outcomes in the AF population.22 Assessment of nutritional status in the AF setting can be challenging, which may explain the paucity of data on malnourished patients. We have previously shown that in elderly patients, the presence of malnutrition markedly altered the embolic-hemorrhagic trade-off, especially in anticoagulated patients.11 This, together with the impact of malnutrition on mortality found in this study, shows that malnutrition is a risk factor for mortality and clinical outcomes that are potentially modifiable. Given the means available to correct malnutrition, prospective interventional studies (such as evaluating the effects of different therapies on nutritional parameters or improving nutrition in these patients) are warranted.
Various studies have shown a conflicting association between obesity and outcomes in the AF patient population.7,8,23,24 Most prior studies used BMI alone as an indicator of obesity, without including body fat percentage, muscle mass, or functional status.25 Unfortunately, few studies have looked into nutritional status specifically in obese patients to study their outcomes. To our knowledge, our study is the first to analyze the impact of nutritional status on the relationship between BMI and mortality in AF patients. Multivariate analysis including age, sex, comorbidities, and nutritional status revealed that neither BMI nor obesity/overweight were associated with a better prognosis. However, malnutrition was a strong predictor of both death and embolic and hemorrhagic events independently from BMI in the 3 groups of patients with normal weight, overweight, and obesity. Our results suggest that obese individuals are not protected from the adverse effects of malnourishment. Therefore, we can affirm that a paradigm shift is taking place: from the obesity paradox to the malnutrition paradigm. This study opens new perspectives: instead of just weighing our patients, to speculate if they will be in a “good” or “bad” BMI class, we should probably evaluate their nutritional status. The true obesity paradox is that a person can be both overweight or obese and malnourished at the same time, as found in 30.2% of our patients.26 Further studies are needed to better qualify the nutritional status of AF patients and, above all, to assess which nutrition protocols may alter the prognosis of our patients, whether obese or not.
LimitationsThis study has the inherent limitations of a retrospective study. Nutritional status was assessed by a simple screening tool, the CONUT score. We did not use more complex comprehensive nutritional assessments. Although our analysis indicates that a diagnosis of malnutrition attenuates the survival advantage of obesity, our diagnosis of malnutrition may be confounded by severity-of-illness markers that may not be related to nourishment and factors that may be more closely linked to nourishment but may not be sensitive to the response to nourishment. Furthermore, since total cholesterol is a parameter of the nutritional scale, the CONUT score could be affected by statin treatment. For this reason, multivariate adjustment included both the Charlson comorbidity index and concomitant statin therapy. Given that nutritional status was evaluated only at a single time point, we did not investigate changes in nutritional status over time and their relationship with clinical outcomes. Moreover, we did not evaluate the association of nutritional status with inflammatory markers or with body composition. In our study, data are limited to white patients, without information on educational attainment, marital status, or socioeconomic characteristics that might help us understand the contributing causes of malnutrition. Confirmation of our findings by other investigators with different health care and social systems would be welcome.
CONCLUSIONMalnutrition is frequent in patients with AF and is a strong predictor of adverse events. In contrast, after adjustment for age, sex, comorbidities, and nutrition status, BMI was not associated with mortality in AF patients
The association between obesity and increased survival in patients with atrial fibrillation, described as the obesity paradox, is known. However, little is known about the prognostic impact of malnutrition in these patients, or whether nutritional status may influence the relationship between body mass index and events in patients with atrial fibrillation.
WHAT DOES THIS STUDY ADD?Malnutrition was common in patients with atrial fibrillation, even in those with high body mass indexes. After adjustment for age, sex, comorbidities, and nutritional status, the prognostic association between body mass index and mortality was lost in patients with atrial fibrillation. However, nutritional status remained a strong predictor of adverse events.
Unconditioned grant Daiichi, Pfyzer, Bayer and Boehringer.
AUTHORS’ CONTRIBUTIONSStudy design: S. Raposeiras-Roubín, E. Abu-Assi, B. Ibáñez, A. Íñiguez Romo. Data collection: A. Lizancos Castro, M. Melendo Viu, M. Cespón Fernández, S. Blanco Prieto. Statistical analysis: S. Raposeiras-Roubín, X. Rosselló, C. Barreiro Pardal, M. Melendo Viu, D. Filgueiras-Rama. Manuscript drafting: S. Raposeiras-Roubín, A. Lizancos Castro, M. Melendo Viu, M. Cespón Fernández. Manuscript revision: S. Raposeiras-Roubín, E. Abu-Assi, X. Rosselló, C. Barreiro Pardal, S. Blanco Prieto, B. Ibáñez, D. Filgueiras-Rama, A. Íñiguez Romo.
CONFLICTS OF INTERESTS. Raposeiras-Roubín has received support grants for research from Pfyzer, Daichii, Bayer and Boehringer and hononaria for presentations by Amgen, AstraZeneca, Daichii, Pfyzer, Bayer and Boehringer. None of the other authors have relevant relationships with industry. D. Filgueiras-Rama is associate editor of the Revista Española de Cardiología; the editorial procedure established in the journal has been followed to guarantee the impartial management of the manuscript.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2022.01.006