There are several techniques for the palliative treatment of patients with single-ventricle physiology, ventriculoarterial discordance and subaortic stenosis. The Fontan procedure relies on optimal initial palliation to avoid the development of subaortic stenosis (as well as ventricular hypertrophy and diastolic dysfunction).
MethodsWe present seven patients with single-ventricle physiology, transposition of the great arteries and subaortic stenosis, with low systemic output and high pulmonary flow, aged 21 to 383 days (median, 75) and weighing between 3.4 and 9.6kg (median, 4.2). All were treated with a palliative arterial switch, thus “switching” their subaortic stenosis to subpulmonary stenosis. Six patients also underwent aortic arch surgery, 4 an atrial septectomy, and 1 a subaortic membrane resection.
ResultsOne patient died after surgery, another developed recoarctation, which was treated with an angioplasty, 3 patients reached the Glenn stage and 2 the Fontan stage. All had good ventricular function.
ConclusionsA palliative switch is an effective initial treatment for single-ventricle physiology with transposition of the great arteries and subaortic stenosis. This complex initial technique produces good results and allows the patient to progress to the Glenn or Fontan stage.
Keywords
There are several techniques for the palliative treatment of patients with single-ventricle physiology, ventriculoarterial discordance and subaortic stenosis. The Fontan procedure relies on optimal initial palliation to avoid the development of subaortic stenosis (as well as ventricular hypertrophy and diastolic dysfunction). We report a series of 7 patients with single-ventricle physiology, transposition of the great arteries and subaortic stenosis, with low systemic output and high pulmonary flow, who were all treated with a palliative arterial switch, thus “switching” their subaortic stenosis to subpulmonary stenosis. We discuss alternatives to this initial palliative treatment and the effects of this technique on patient progression to the Fontan stage.
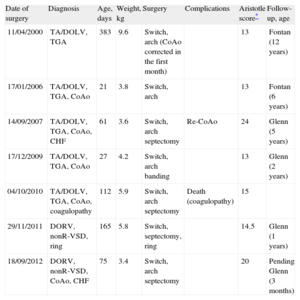
METHODSPatient age ranged from 21 to 383 days (median 75) and patient weight from 3.4 to 9.6kg (median 4.2). The oldest patient had previously undergone surgery at another aortic coarctation unit at 7 days of life. The initial diagnosis was tricuspid atresia/double outlet left ventricle and transposition of the great arteries (tricuspid atresia/double outlet left ventricle) in 5 patients, and double outlet right ventricle with unrelated ventricular septal defect (nonR-VSD) in 2; 5 patients had aortic coarctation and 1 also had a subaortic ring; 2 patients had moderate/severe ventricular dysfunction (congestive heart failure) and another had severe coagulopathy due to hepatic impairment. The patients’ comprehensive Aristotle score ranged from 13 to 24 (median 14.5). All had subaortic stenosis, caused in the first 5 patients by a restrictive VSD (bulboventricular foramen) (Table).
Follow-up of Study Patients
| Date of surgery | Diagnosis | Age, days | Weight, kg | Surgery | Complications | Aristotle score* | Follow-up, age |
| 11/04/2000 | TA/DOLV, TGA | 383 | 9.6 | Switch, arch (CoAo corrected in the first month) | 13 | Fontan (12 years) | |
| 17/01/2006 | TA/DOLV, TGA, CoAo | 21 | 3.8 | Switch, arch | 13 | Fontan (6 years) | |
| 14/09/2007 | TA/DOLV, TGA, CoAo, CHF | 61 | 3.6 | Switch, arch septectomy | Re-CoAo | 24 | Glenn (5 years) |
| 17/12/2009 | TA/DOLV, TGA, CoAo | 27 | 4.2 | Switch, arch banding | 13 | Glenn (2 years) | |
| 04/10/2010 | TA/DOLV, TGA, CoAo, coagulopathy | 112 | 5.9 | Switch, arch septectomy | Death (coagulopathy) | 15 | |
| 29/11/2011 | DORV, nonR-VSD, ring | 165 | 5.8 | Switch, septectomy, ring | 14.5 | Glenn (1 years) | |
| 18/09/2012 | DORV, nonR-VSD, CoAo, CHF | 75 | 3.4 | Switch, arch septectomy | 20 | Pending Glenn (3 months) |
CHF, congestive heart failure; CoAo, coarctation of the aorta; DORV, double outlet right ventricle; nonR-VSD, unrelated ventricular septal defect (not related to aortic or pulmonary valves); TA/DOLV, tricuspid atresia/double outlet left ventricle; TGA, transposition of the great arteries.
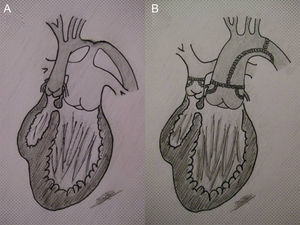
A midline sternotomy incision was made with the patient on extracorporeal circulation. First, the aortic coarctation was corrected by widening the arch using an autologous pericardial patch. Then, the arterial switch was performed using the standard method, with reconstruction of the new pulmonary artery by using an autologous pericardial patch (Figure). All patients had a type A coronary branching pattern. The Lecompte manoeuver was performed in the first 5 patients (anteroposterior position of the great arteries) but not in the last 2 (side-to-side position, as with a Taussig-Bing anomaly). Four patients required widening of the atrial septal defect (septectomy). In another, a subaortic ring was removed. The intraoperative ultrasound scan showed that the abnormality had been successfully corrected in all patients, with a slight dysfunction in 2 patients with preoperative heart failure. One patient required pulmonary artery banding during the procedure. No additional shunts were required. The surgery was performed by LM at Vall d’Hebron Hospital (Barcelona) in 2 patients and by JMGJ in 5 (the first at the same center, and the remaining 4 at Carlos Haya Hospital in Malaga).
A: left ventricle connected to the pulmonary artery (high flow) and right ventricle (rudimentary) connected to the aorta (single-ventricle physiology with transposition of the great arteries); restrictive ventricular septal defect (subaortic stenosis) and aortic coarctation. B: repaired arch plus palliative switch, connecting the left ventricle with the neoaorta and creating subpulmonary stenosis (pulmonary flow regulated by the restrictive ventricular septal defect).
One patient died following the procedure due to uncontrollable coagulopathy (present prior to the surgery). Another patient developed recoarctation (requiring percutaneous dilatation before the Glenn procedure).
Follow-upAll patients had good ventricular function with no subaortic stenosis or residual pressure gradient in the arch after a mean follow-up period of 57 months (3-148) at their respective centers. The two oldest patients (currently aged 12 and 6 years) have undergone the Fontan procedure and 3 others (aged 1, 2, and 5 years) have reached the Glenn stage. The hemodynamic analysis prior to the Glenn and Fontan techniques showed that pulmonary and end-diastolic pressures were normal in 5 patients.
DISCUSSIONThe value of initial palliative treatment in patients with single-ventricle physiology, transposition of the great arteries and subaortic stenosis is controversial, especially when the diameter of the VSD is less than that of the aortic valve. Correcting the coarctation with the addition of pulmonary banding can aggravate the subaortic stenosis and compromise the future success of the Fontan procedure (similar to the first patient in our study with prior coarctation surgery). Widening the restrictive VSD is a complicated and risky approach (complete block). Norwood or Damus-Kaye-Stansel type procedures offer effective palliation but produce considerable morbidity and mortality in Spain.
The first palliative switch was reported by Freedom et al.1 in 1980. Subsequently, Karl et al.2 (in 1991) and Lacour-Gayet et al.3 (in 1992) reported their results in neonates, as an alternative to the Norwood and other techniques. These authors argued the benefits of autologous, valved, non-shunt-dependent pulmonary artery flow. Despite good results, they questioned the viability of a palliative switch as an initial technique prior to the Fontan procedure. The first Spanish case was published by a group in Valencia in 1996.4 Other authors5,6 have highlighted the following theoretical benefits of a palliative switch vs the Norwood procedure:
- •
Creation of laminar flow through a correct left ventriculoarterial connection.
- •
Better distortion of the semilunar valves (neoaorta).
- •
Disappearance of the subaortic stenosis.
- •
Avoidance of the need for a systemic to pulmonary artery shunt (and its complications).
- •
Natural protection of the pulmonary vascular bed (regulated by the subpulmonary stenosis instead of by a shunt).
- •
Lesser degree of stenosis in the left pulmonary artery.
- •
Lower mortality, both during hospital admission and between procedures.
Two possible complications have also been predicted5: the long-term complications inherent to any arterial switch (fundamentally relating to the coronary arteries), and the difficulty of controlling pulmonary flow (self-regulated by the restrictive VSD) which in some cases may require banding or an associated shunt.2,3,5,6
In 2008, Ceresnak et al.5 published the first series of palliative switches (9 patients) who reached the Fontan stage (6 patients). These authors highlighted the lower initial mortality than that produced by other palliative techniques and concluded that such patients are suitable candidates for a future Fontan procedure.
Recently, Fraser6 has reported 10 patients, of which 4 reached the Fontan stage. He compares his results (100% survival) with those of other techniques and concludes that there is a need for more “aggressive” initial palliation to avoid potential complications (due to subaortic stenosis and ventricular hypertrophy).
Our initial series produced good results, with 1 death and 1 recoarctation. The first 5 patients had a similar anatomy and the surgical approach described above was used (Figure). The last 2 patients had undergone variants of a double outlet right ventricle with nonR-VSD. Previous experience led us to treat them in the same way and we obtained a result similar to that achieved with a Taussig-Bing anomaly correction, but leaving the VSD open. All patients had a high surgical risk score.7 The only death was caused by complications relating to a preexisting coagulopathy. Only 1 patient required banding, compared with other reports that describe associated banding and shunts. During the follow-up, 3 patients reached the Glenn stage and 2 the Fontan stage. There are very few reports that describe the initial technique and follow-up of such patients. There is also a shortage of Spanish publications on this topic.8
CONCLUSIONSA palliative arterial switch is a good initial option in patients with single-ventricle physiology with transposition of the great arteries and subaortic stenosis, which is converted to subpulmonary stenosis. Although a complicated and aggressive procedure, the resulting physiopathology preserves the patient's ventricular function and avoids any diastolic dysfunction or hypertrophy. The few publications on this topic show that the Glenn and Fontan stages can be achieved by using this strategy.
CONFLICTS OF INTERESTNone declared.