Percutaneous coronary intervention (PCI) for aorto-ostial chronic total coronary occlusion (CTO) can be a particularly challenging lesion subset. The aim of this study was to analyze the technical aspects and outcomes of aorto-ostial CTO PCI in a multicenter registry.
MethodsPatients undergoing aorto-ostial CTO PCI at 4 centers between February 2013 and December 2018 were included. Success rates, as well as procedural aspects and outcomes, were analyzed.
ResultsA total of 103 patients were included. Mean age was 64±10 years and the mean J-CTO score was 3.1±1.1. Thirty-one lesions (30.4%) were flush ostial CTOs. Technical and procedural success were achieved in 79 (76.7%) and 78 (75.7%) of the patients, respectively. The retrograde approach was the most frequent successful crossing technique (n=49; 62.0%), especially in flush vs nonflush aorto-ostial CTOs (82.6% vs 53.5%; P=.02). The only variable independently associated with technical failure was the absence of interventional collaterals (OR, 12.38; 95%CI, 4.02-38.15; P <.001). Coronary perforation occurred in 4 patients (3.9%) requiring covered stent implantation (without subsequent cardiac tamponade) and 2 patients (1.9%) had a stroke (one of which was a transient ischemic attack). During a median follow-up of 31 months, 3 (2.9%) patients died from cardiovascular causes and 13 (12.6%) required repeat target vessel revascularization.
ConclusionsAorto-ostial occlusions represent a challenging subset for PCI. However, an acceptable success rate with favorable outcomes during follow-up can be achieved by experienced operators. The presence of interventional collaterals allowing the use of the retrograde approach is key for achieving procedural success.
Keywords
Although the development of dedicated devices and the growing experience of operators have significantly increased procedural success rates, chronic total coronary occlusions (CTO) are still considered the most complex lesion subset for percutaneous coronary intervention (PCI).1,2 In this setting, special subgroups confer additional challenges.3–5 Aorto-ostial CTOs are often associated with unfavorable anatomic characteristics such as proximal cap ambiguity and unclear vessel course.6,7 This type of lesions hampers coronary engagement with the guide catheter, limiting the success of antegrade crossing strategies.7 Consequently, the technical options to recanalize the occluded vessel are usually limited, with a primary or secondary retrograde approach often being required in these cases. There are limited published data on PCI for aorto-ostial CTOs.8,9
The aim of this study was to analyze the technical aspects, as well as the acute and long-term outcomes of aorto-ostial CTO PCI in a large retrospective multicenter registry.
METHODSPatientsPatients undergoing attempted aorto-ostial CTO PCI at 4 high-volume centers with specialized CTO PCI programs, between February 2013 and December 2018, were included in this study. Two centers only enrolled patients during part of the study period. All procedures were indicated according to the presence of angina, evidence of ischemia, or both, and were performed electively10 by experienced operators. Clinical, angiographic, procedural, hospitalization and follow-up data were recorded. All participants gave informed consent for the procedure and for data analysis and publication.
ProcedureCTO PCI was performed in all patients using the femoral or radial approach, at the operator's discretion, using simultaneous double injection, with the exception of patients with only ipsilateral collateral filling.
The patients were pretreated with dual antiplatelet therapy. In the cardiac catheterization laboratory, weight-adjusted heparin was administered to maintain an activated clotting time for> 300seconds and was monitored every 30minutes to determine whether an additional bolus of unfractionated heparin was necessary. After the procedure, all patients received 81 to 100mg of aspirin daily indefinitely and a maintenance dose of clopidogrel (75mg/d), prasugrel (10mg/d) or ticagrelor (90mg twice daily) for 6 to 12 months.
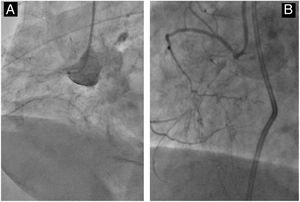
DefinitionsCTO was defined as an occlusive (100% stenosis) coronary lesion with antegrade Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 for at least 3months.11 A CTO was considered to be aorto-ostial if the proximal cap was within 5mm of the aortocoronary ostium.8 Flush aorto-ostial occlusion was defined as the complete absence of a stump at the aortocoronary junction (figure 1). The J-CTO (Japanese-Chronic Total Occlusion) score12 and the PROGRESS-CTO score13 were calculated for each lesion.
Technical success was defined as residual stenosis <30% with TIMI 3 flow in the CTO vessel.10 Procedural success was defined as technical success plus the absence of in-hospital adverse events (all-cause death, Q-wave myocardial infarction, stroke, recurrent angina requiring target vessel revascularization with PCI or coronary artery bypass graft, tamponade requiring pericardiocentesis or surgery).10 Procedural complications and in-hospital adverse events included death, stroke, periprocedural type 4a myocardial infarction,14 need for urgent revascularization, major bleeding (bleeding requiring transfusion, vasopressors, surgery, or percutaneous intervention), vascular complications, coronary perforation requiring intervention (coil embolization, covered stent implantation, pericardiocentesis, and/or surgery), and contrast-induced nephropathy (increase in serum creatinine> 25% or> 0.5 mg/dL at 48hours postprocedure). Major adverse cardiac events (MACE) on follow-up were defined as a composite of cardiac death, myocardial infarction, and clinically-driven target lesion revascularization.
Follow-up studyClinical follow-up was performed with scheduled visits and telephone calls. Patients with symptom recurrence or with inducible ischemia were recommended to undergo angiographic evaluation.
Statistical analysisContinuous variables are expressed as the mean±standard deviation or median [IQ25-75]. Categorical variables are presented as counts and percentages. Independent predictors of recanalization failure were studied using a backward stepwise logistic regression model. Variables with a P-value of ≤ .1 in univariate analyses and those previously linked with technical failure were introduced into the model. The final model included the following variables: flush ostial CTO, blunt stump/proximal cap ambiguity, moderate-severe calcification, moderate-severe tortuosity, occlusion length> 20mm, in-stent CTO and the absence of interventional collaterals. A P value of <.05 was considered statistically significant. Model fit was evaluated with the Hosmer-Lemeshow goodness-of-fit test. Statistical analyses were performed using SPSS, version 20 (IBM Corp., United States).
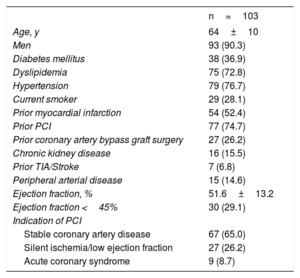
RESULTSClinical characteristicsDuring the study period, 1371 patients underwent CTO PCI at the 4 participating centers. Of these, 103 (7.5%) patients had an aorto-ostial CTO and were included in this registry. Clinical characteristics of the study population are shown in table 1. Mean age was 64±10 years and 90.3% of the patients were men. The prevalence of cardiovascular risk factors was high: half of the study population had prior myocardial infarction, three quarters prior PCI, and one quarter prior coronary artery bypass grafting. The most frequent indication for CTO PCI was angina despite optimal medical treatment.
Baseline clinical characteristics
| n=103 | |
|---|---|
| Age, y | 64±10 |
| Men | 93 (90.3) |
| Diabetes mellitus | 38 (36.9) |
| Dyslipidemia | 75 (72.8) |
| Hypertension | 79 (76.7) |
| Current smoker | 29 (28.1) |
| Prior myocardial infarction | 54 (52.4) |
| Prior PCI | 77 (74.7) |
| Prior coronary artery bypass graft surgery | 27 (26.2) |
| Chronic kidney disease | 16 (15.5) |
| Prior TIA/Stroke | 7 (6.8) |
| Peripheral arterial disease | 15 (14.6) |
| Ejection fraction, % | 51.6±13.2 |
| Ejection fraction <45% | 30 (29.1) |
| Indication of PCI | |
| Stable coronary artery disease | 67 (65.0) |
| Silent ischemia/low ejection fraction | 27 (26.2) |
| Acute coronary syndrome | 9 (8.7) |
PCI, percutaneous coronary intervention; TIA: transient ischemic attack.
Data are expressed as No. (%) or mean±standard deviation.
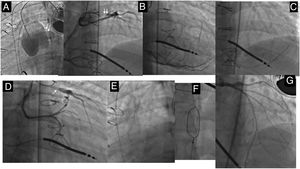
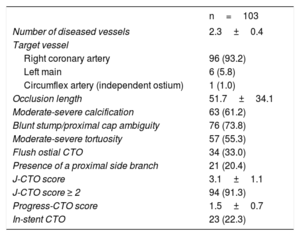
The angiographic features of the target lesions are presented in table 2. The most frequent target CTO vessel was the right coronary artery (n=96, 93.2%). Six patients (5.8%) underwent PCI of an occluded left main coronary (figure 2) and 1 patient (1%) had a CTO of a circumflex artery with a separate ostium. The mean J-CTO score was 3.1±1.1. Most CTOs had moderate or severe calcification (n=63; 61.2%) and proximal cap ambiguity (n=76; 73.8%). Additionally, flush ostial CTOs were present in 34 (33.0%) of the patients.
Angiographic characteristics
| n=103 | |
|---|---|
| Number of diseased vessels | 2.3±0.4 |
| Target vessel | |
| Right coronary artery | 96 (93.2) |
| Left main | 6 (5.8) |
| Circumflex artery (independent ostium) | 1 (1.0) |
| Occlusion length | 51.7±34.1 |
| Moderate-severe calcification | 63 (61.2) |
| Blunt stump/proximal cap ambiguity | 76 (73.8) |
| Moderate-severe tortuosity | 57 (55.3) |
| Flush ostial CTO | 34 (33.0) |
| Presence of a proximal side branch | 21 (20.4) |
| J-CTO score | 3.1±1.1 |
| J-CTO score ≥ 2 | 94 (91.3) |
| Progress-CTO score | 1.5±0.7 |
| In-stent CTO | 23 (22.3) |
CTO, chronic total coronary occlusion.
Data are expressed as No. (%) or mean±standard deviation.
Left main CTO after Jatene surgery. Ostial left main CTO after Jatene surgery. Contralateral filling from the RCA and LCx (anomalous origin of the LCx from the RCA) (arrows) (A, B). A retrograde approach was chosen (C). A Sion guidewire (Asahi Intecc, Japan) was advanced through a microcatheter from the RCA to the diagonal branch, reaching the distal cap of the occlusion (arrow) (D). A Pilot 200 (Abbott, United States) passed into the aorta (arrows) (ER). The externalization guidewire was snared to create the circuit (F). Final result after drug-eluting stent implantation (G). CTO, chronic total coronary occlusion; LCx, left circumflex coronary artery; RCA, right coronary artery.
The procedural data of this cohort are shown in table 3. The access site was bifemoral or radial-femoral in most of the patients (n=89; 86.4%). A single guide catheter was used in 12 (11.6%) patients. The retrograde approach was the initial crossing strategy in most patients (n=62; 60.2%), as well as the final successful strategy: retrograde wire escalation in 17 (21.5%) patients and reverse controlled antegrade and retrograde tracking in 32 (40.5%). In flush ostial CTOs, retrograde strategies were the successful crossing techniques in an even higher proportion of cases (n=19/23, 82.6% vs n=30/56, 53.6%, in flush vs no flush ostial CTO; P=.02). However, in patients with in-stent CTO, antegrade techniques were the most common successful recanalization strategies (n=12/18, 66.7% vs n=18/61, 29.5%; P=.01).
Procedural data
| n=103 | |
|---|---|
| Contralateral injection | 91 (88.3) |
| Access site | |
| Bifemoral | 57 (55.3) |
| Femoral – Radial | 32 (31.1) |
| Biradial | 2 (1.9) |
| Single femoral | 9 (8.7) |
| Single radial | 3 (2.9) |
| Crossing strategies attempted | |
| AWE | 42 (40.1) |
| ADR | 19 (18.4) |
| Retrograde approach | 81 (78.6) |
| Initial crossing strategy attempt | |
| AWE | 33 (32.0) |
| ADR | 8 (7.8) |
| Retrograde approach | 62 (60.2) |
| Final successful crossing technique | |
| AWE | 20 (25.3) |
| ADR | 10 (12.6) |
| RWE | 17 (21.5) |
| RDR | 32 (40.5) |
| None | 24 (23.3) |
| Externalization technique | |
| Externalization wire into guiding catheter | 30 (61.2) |
| Snaring in aorta | 8 (16.3) |
| Tip-in | 10 (20.4) |
| Rendez-vous | 1 (2.1) |
| Type of stent: | |
| Second generation DES | 97 (94.2) |
| Bioresorbable scaffolds | 6 (5.8) |
| Diameter of largest stent, mm | 3.34±0.49 |
| Stent length, mm | 72±31 |
| IVUS | 42 (40.7) |
| Contrast volume, mL | 307±246 |
| Fluoroscopy time, min | 70±32 |
| Radiation dose, Gy/cm2 | 312±246 |
ADR, antegrade dissection reentry; AWE, antegrade wire escalation; DES, drug-eluting stents; IVUS, intravascular ultrasound; RDR, retrograde dissection and reentry; RWE, retrograde wire escalation.
Data are expressed as No. (%) or mean±standard deviation.
Guidewire externalization after retrograde crossing was commonly performed using the conventional technique using a long externalization wire (n=30/49, 61.2%).
Technical and procedural success were achieved in 79 (76.7%) and 78 (75.7%) of the patients, respectively. In our series, the success rate of nonaorto-ostial CTOs was significantly higher (89.8% vs 76.7%, P <.001). Moreover, there was a trend toward a lower technical success rate in the flush ostial CTOs in comparison with no flush CTOs (23/34, 67.6% vs 56/69, 81.2%; P=.13). The reasons for failed recanalization were the following: absence of interventional collaterals in 14/24 patients (58.3%), presence of an impenetrable proximal cap in 7 (29.2%), and inability to advance the microcatheter through the collaterals after successful wiring in the remaining 3 patients (12.5%).
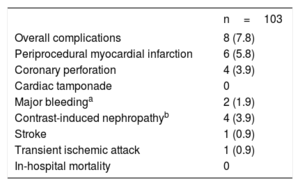
In-hospital and follow-up outcomesIn-hospital complications are presented in table 4. Periprocedural MI was diagnosed in 6 (5.8%) patients, and was associated with a coronary perforation requiring intervention in 2 of them. In the remaining patients, this was an asymptomatic event with no clinical consequences. We observed 4 coronary perforations (3.9%), which were all successfully treated with covered stent implantation, without subsequent cardiac tamponade. Vascular complications were observed in 6 (5.8%) patients, mainly minor complications consisting of local hematoma (n=4, 3.9%). Two patients had a major bleeding at the puncture site (1.9%). Other complications included contrast-induced nephropathy (n=4; 3.9%) without the need for dialysis, transient ischemic attack (n=1; 0.9%) and stroke (n=1; 0.9%).
In-hospital adverse events
| n=103 | |
|---|---|
| Overall complications | 8 (7.8) |
| Periprocedural myocardial infarction | 6 (5.8) |
| Coronary perforation | 4 (3.9) |
| Cardiac tamponade | 0 |
| Major bleedinga | 2 (1.9) |
| Contrast-induced nephropathyb | 4 (3.9) |
| Stroke | 1 (0.9) |
| Transient ischemic attack | 1 (0.9) |
| In-hospital mortality | 0 |
Data are expressed as No. (%).
During a median follow-up of 31 months [16.5-44], the MACE rate was 15.5%. Five (4.8%) patients died, 3 of them (2.9%) from cardiovascular causes and 2 (1.9%) due to noncardiac causes (end stage chronic kidney disease and pulmonary disease). Thirteen patients (12.6%) required repeat target vessel revascularization due to focal restenosis in 4 patients (30.8%), diffuse in 6 (46.1%) and reocclusion in the remaining 3 patients (23.1%). Twelve patients had been previously treated with second generation drug-eluting stents and 1 patient with a bioresorbable scaffold.
With regard to the patients with successfully treated in-stent CTO, only 1 of them needed repeat target vessel revascularization because of a new reocclusion.
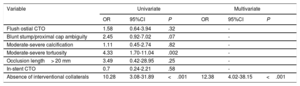
Factors associated with technical failureFactors associated with technical failure are presented in table 5. The absence of interventional collaterals was the only factor associated with a higher risk of technical failure (OR, 12.38; 95% confidence interval, 4.02-38.15; P <.001).
Predictors of technical failure
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Flush ostial CTO | 1.58 | 0.64-3.94 | .32 | - | ||
| Blunt stump/proximal cap ambiguity | 2.45 | 0.92-7.02 | .07 | - | ||
| Moderate-severe calcification | 1.11 | 0.45-2.74 | .82 | - | ||
| Moderate-severe tortuosity | 4.33 | 1.70-11.04 | .002 | - | ||
| Occlusion length> 20 mm | 3.49 | 0.42-28.95 | .25 | - | ||
| In-stent CTO | 0.7 | 0.24-2.21 | .58 | - | ||
| Absence of interventional collaterals | 10.28 | 3.08-31.89 | <.001 | 12.38 | 4.02-38.15 | <.001 |
95%CI, 95% confidence interval; CTO, chronic total coronary occlusion; OR: odds ratio.
This study sought to analyze the clinical and angiographic characteristics, procedural aspects, and outcomes of a particularly challenging CTO PCI subset, aorto-ostial occlusions. The main findings of our registry are as follows: a) aorto-ostial CTOs have high complexity, often requiring the use of the retrograde approach; b) the PCI success rate of aorto-ostial CTOs was lower than those reported in the literature in all-comers with CTOs, although with a reasonably low incidence of complications; d) as a retrograde approach is usually required to cross the occluded segment, the presence of interventional collaterals seems to be key for achieving procedure success; d) the incidence of MACE on follow-up was reasonably low and similar to that of other contemporary series.
To the best of our knowledge, this is the first study exclusively focused on aorto-ostial CTO PCI. In line with previous studies including side branch ostial and aorto-ostial CTOs,8,9 these occlusions were found in patients with an extensive comorbidity burden, with a high prevalence of cardiovascular risk factors and comorbidities. Likewise, the angiographic characteristics were also fairly unfavorable, as reflected by a mean J-CTO score of approximately 3. Among them, a blunt/ambiguous stump (arguably the most adverse feature in a CTO) was observed in most of the patients (n=76, 73.8%) and a flush ostial occlusion in about one third of our series.15 Additionally, only 20% of the patients had a proximal side branch allowing an anchoring technique or the use of intravascular ultrasound to guide the proximal cap puncture.16
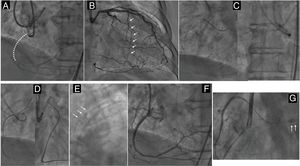
An aorto-ostial occlusion hampers coronary engagement with the guide catheter (figure 3). Moreover, guide support is often poor. As a consequence, a primary retrograde approach can be the most effective alternative to cross the occluded segment. In fact, in our study, a retrograde approach was attempted in most patients (n=81, 78.6%) and was the most common final successful crossing technique (n=49, 62%). Additionally, in flush aorto-ostial CTOs, retrograde techniques were required in an even higher proportion of the patients. These percentages are well above the figures provided by large contemporary registries,1,17–21 in which antegrade techniques were predominant. In fact, the specific angiographic complexity features of this subset of CTOs often induce the operator to choose a retrograde approach, which is sometimes the only feasible revascularization strategy (particularly in stumpless aorto-ostial occlusions).1,17–19 In this regard, we found that the absence of “interventional” collaterals was the only factor independently associated with recanalization failure, underlining the importance of a retrograde access to improve the success rate. Although “interventional collaterals” are usually defined as collaterals that appear suitable for being crossed with a guidewire and a microcatheter according to the operator's judgemen,13 that criterion is subjective and highly dependent on operator skills and experience: collaterals initially considered to be interventional, later prove to be uncrossable. Additionally, “invisible” (CC0)22 collaterals can often be successfully crossed using the “surfing” technique.23
Flush ostial occlusion of the right coronary artery (RCA) recanalized with a retrograde approach. Flush ostial RCA occlusion (dotted line) with distal filling by contralateral collaterals (A). The total absence of stump hampered coronary engagement with the guide catheter. As a consequence, a retrograde approach was planned as the first option through a septal channel (arrows) (B). The retrograde wire crossed the occluded segment in what was thought to be the aorta. However, this possibility was ruled out by a contralateral projection (C). Finally, and after several attempts, a Confianza Pro 12 (Asahi Intecc, Japan) crossed through the ostium retrogradely and passed into the aorta (D). After confirmation of the correct position of the wire in the aorta lumen, the retrograde microcatheter was advanced. Then, the externalization guidewire was introduced into an antegrade multipurpose catheter (arrows) creating a circuit (E). Final result after 2 overlapping drug-eluting stents (F). Small contained perforation (arrows) caused by the exit of the retrograde guidewire (G).
The adoption of the hybrid algorithm along with the development of new specialized wires and microcatheters have allowed high success rates to be achieved in CTO PCI.24,25 In the present study, these rates were acceptable, but slightly lower than those reported in large contemporary all-comers CTO PCI registries.1,17–19 That finding could be explained by the anatomic complexity of these occlusions, a factor clearly associated with the probability of recanalization, together with the limited technical options available in some cases. Accordingly, we observed a trend toward a lower technical success rate in the most complex subgroup, represented by flush ostial CTOs.
Although the risk for complications is related to the use of advanced crossing techniques, commonly required in more complex occlusions,1 the overall complication rate was relatively low in our series, which is likely related to the experience of the operators involved in the study. Indeed, a stiff guidewire can be required to cross through the ostium retrogradely to pass into the aorta. In such setting, the risk of a subintimal pathway is nonnegligible and this could be associated with aortic root injury (dissection). To avoid these complications, the operator should not advance the retrograde microcatheter until the correct position of the wire in the aorta lumen is confirmed (figure 3).
Moreover, the retrograde approach is associated with a risk of perforation, donor vessel injury, ischemia, and equipment entrapment. Proximal cap ambiguity is also associated with a risk of perforation when an antegrade approach is undertaken.26–28
LimitationsThis was a retrospective registry without core laboratory assessment of the study angiograms and adjudication of clinical events by a clinical events committee. Moreover, the procedures were performed in high-volume CTO centers by experienced operators: as a consequence, our study findings might therefore not be generalizable to other less experienced operators. Finally, the sample size was relatively small and comparison with a group of nonaorto-ostial CTOs was not possible.
ConclusionsAorto-ostial occlusions represent a particularly challenging subset of CTO PCI. In the hands of experienced operators, an acceptable success rate can be achieved, with an acceptable incidence of complications, considering the complexity of the lesions and unfavorable anatomic characteristics for PCI. As the only option for recanalization is frequently a retrograde approach, the existence of interventional collaterals, as well as mastering the retrograde, approach seems to be key in procedural success. During long-term follow-up, the incidence of adverse events is reasonably low and should not discourage recanalization attempts.
CONFLICTS OF INTERESTS. Ojeda received horaria from Terumo and Philips. M. Pan received horaria from Terumo, Abbott Vascular, and Philips. E.S. Brilakis received consulting/speaker honoraria from Abbott Vascular, American Heart Association (associate editor Circulation), Boston Scientific, Cardiovascular Innovations Foundation (Board of Directors), CSI, Elsevier, GE Healthcare, InfraRedx, and Medtronic; research support from Regeneron and Siemens; is a shareholder of MHI Ventures; and is on the Board of Trustees of the Society of Cardiovascular Angiography and Interventions. L. Azzalini received honoraria from Abbott Vascular, Guerbet, Terumo, and Sahajanand Medical Technologies; and research support from ACIST Medical Systems, Guerbet, and Terumo. The other authors have no disclosures.
- -
The anatomic characteristics of aorto-ostial CTOs can confer additional challenges for PCI and the technical options to recanalize the occluded vessel are usually limited.
- -
There are scarce data on experience with percutaneous revascularization of this lesion subset.
- -
This multicenter registry shows that, in these complex CTOs, an acceptable success rate can be achieved with a low incidence of complications.
- -
As a retrograde approach is usually required, the existence of interventional collaterals seems to be key in procedural success.
- -
On long-term follow-up, the incidence of adverse events is reasonably low.