Up to 40% of patients treated with transcatheter aortic valve implantation (TAVI) have at least moderate mitral regurgitation (severe in 15.9%), and its persistence after prosthesis implantation (7.9% of patients) negatively affects prognosis.1 In almost half of the patients, mitral regurgitation is reduced, mainly in patients with functional etiology, nondilated annulus, and noncalcified valves.1,2 If the regurgitation is not reduced and the patient continues to have limiting symptoms, one option that has been proposed is the use of percutaneous repair techniques with the MitraClip device; there are already published case series of solution in Europe.3 In Spain, the use of the MitraClip has become more widespread since 2011, mainly for patients with functional mitral regurgitation.4,5 The technique requires adequate mitral valve anatomy to allow MitraClip implantation, although it has been proposed that the selection criteria be relaxed in centers with experience.6 In patients with TAVI, the mitral annulus and/or mitral leaflets are often calcified, which can limit the treatment indication, and therefore the valve must be assessed in detail.
This study combines the experience of the first 5 cases of severe mitral regurgitation after percutaneous treatment with TAVI performed in 3 hospitals in Spain (2015 to 2016), with particular emphasis on patient selection.
Below we present the characteristics at baseline, those related to the previous TAVI, to MitraClip implantation, and at follow-up. Mitral regurgitation was present prior to TAVI in all 5 patients and persisted without reduction until MitraClip implantation, an average of 16.2 months later.
In patients 1, 2, and 5, and particularly in 5, the valve had abnormalities (degenerative etiology), which the clinician must take into account when deciding whether the procedure is indicated:
- •
The free edge of the anterior mitral valve must have at least 1 free 7-mm segment6 that does not interfere with the TAVI. The presence of a previous dysfunctional bioprosthesis treated with TAVI (valve-in-valve), as in patient 1, did not present anatomical obstacles to treatment with MitraClip. Similarly, patient 3 had a double TAVI valve (both implanted in the same procedure because the first was too deep at 13mm), although this did not interfere with the MitraClip device. The average depth of the valves was 7.25 mm.
- •
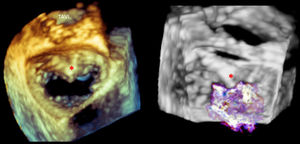
Calcification and flexibility of leaflets: in patients with calcified degenerative aortic stenosis, the calcification often extends to the posterior mitral annulus and to the “mitral-aortic curtain”, as in patient 5 (Figure). Once again, at least 7mm of noncalcified tissue is required in each of the valves to allow device implantation. In patient 5, the regurgitation jet originated on either side of the calcified area, and it was possible to implant the devices avoiding this (Figure). The presence of calcified areas is only compatible with treatment with MitraClip if there is a good valve area in general (> 4 cm2) and the rest of the valve is sufficiently flexible.
Figure.Three-dimensional transesophageal echocardiogram with a view of the mitral valve from the left atrium in patient 5. The asterisk indicates an area of calcification along the mitral-aortic curtain. The regurgitation originates mainly on either side of the calcified area. TAVI, transcatheter aortic valve implantation.
(0.11MB). - •
Valve area: ideally, the available area should be > 4 cm2, although a smaller area can be tolerated (up to 3 cm2) provided the valves are flexible and not thickened or calcified. In the patient series presented, the average valve area was 4.14cm2, and it was possible to implant 2 MitraClip devices without producing stenosis in 4 of the 5 patients.
The outcomes of MitraClip implantation were successful in both reducing mitral regurgitation and producing clinical improvement; mean follow-up was 9.6 months. All patients had an initial improvement in functional class to at least grade II, although at follow-up, 3 patients with severe ventricular dysfunction had deteriorated in functional status. In one of them, mitral regurgitation progressed to grade II-III.
In conclusion, MitraClip may be an option for patients with mitral regurgitation after TAVI, although complex valvular anatomies can be expected; therefore, it is advisable to perform the treatment in centers with a high patient volume. Registries are needed to define the clinical profile of the patients that may benefit most from this treatment.
CONFLICTS OF INTERESTF. Carrasco-Chinchilla, R. Estévez-Loureiro, and X. Freixa declare a possible conflict of interest due to collaboration with Abbott vascular.