Percutaneous heart valve interventions have emerged as an alternative in patients at high or prohibitive risk for surgery. Mitral transcatheter edge-to-edge repair (M-TEER) is currently a well-established treatment for functional mitral regurgitation (MR)1,2 and can also be considered a valid option in degenerative or acute MR for patients at high risk. M-TEER has, however, procedural limitations3 in complex anatomies, and no other specific reparative options are currently available. There have been some reports of the use of vascular plugs in combination with M-TEER for challenging anatomies,4 but the use of Amplatzer Vascular Plug III (AVP III) (Abbott, United States) has been less described. AVP III is specifically designed for paravalvular leak closure but, because of its asymmetrical shape with a thick neck, it is also appropriate for treating localized residual MR jets after M-TEER.5 We describe our experience of combined treatment with M-TEER and AVP III for challenging mitral anatomies.
Patients treated in our center with M-TEER were retrospectively reviewed to identify those needing a combined therapy with occluders. Patients signed the consented inform for the intervention and all reported data were anonymized.
Since 2012, 242 patients have been treated at our center with M-TEER (MitraClip [Abbott, United States] or PASCAL [Edwards Lifesciences, United States]). Throughout this period, 5 patients required implantation of an additional plug after M-TEER. In addition, although other options are available to treat recurrent MR after edge-to-edge therapy, such as the ELASTA-Clip, we chose this technique because of the presence of a localized MR and the lesser invasiveness of the plug implantation.
The clinical and procedural characteristics of the 5 patients are described in table 1. All of the patients had severe symptomatic MR at the moment of the plug implantation. The patients also had challenging anatomies for M-TEER: a) ischemic MR due to papillary muscle rupture with prolapse of the posterior leaflet initially treated with 2 MitraClip NT; b) mixed etiology MR with P1 and anterior commissure prolapse with severe calcification at that level; c) degenerative MR with a wide prolapse of the anterior leaflet (A2-A3); d) combined etiology MR with dilated cardiomyopathy and A2 prolapse with chordal rupture treated with 2 MitaClip NT, new heart failure onset (5.5 years later) due to new A3 prolapse with chordal rupture and interclip MR; e) myxomatous degeneration of the mitral valve with prolapse of the posterior leaflet due to chordal rupture.
Clinical and procedural characteristics of the treated patients
| Patient | #1 | #2 | #3 | #4 | #5 |
|---|---|---|---|---|---|
| Sex and age at 1st intervention | Man, 59 y | Woman, 77 y | Man, 82 y | Man, 70 y | Man, 84 y |
| Acute MR | Yes | Yes | Yes | Yes | No |
| Hemodynamic instability | Yes | No | Yes | Yes | No |
| MR mechanism | Ischemic, papillary muscle rupture | Degenerative, P1 and lateral commissure prolapse | Degenerative, A2-A3 prolapse | Mixed, functional+A2 prolapse | Degenerative, myxomatous degeneration+A2-A3 prolapse |
| Clips and position (1st intervention) | MitraClip NT x 2 (A2-P2) | MitraClip NT x 1 (A1-P1) | MitraClip XTx2+NTx1 (A2/A3-P2/P3) | MitraClip NT x 2 (A2-P2) | MitraClip NT x 2 (A2/A3-P2/P3) |
| Plug implantation (1st intervention) | no | no | AVP III 14x5mm Medial commissure | no | no |
| Intervention duration, min | 162 | 106 | 142 | 101 | 67 |
| Initial residual MR | Moderate | Severe | Mild to moderate | Mild | Moderate-severe |
| Mean gradient after the intervention, mmHg, and HR, bpm | 7 (117) | 6.5 (96) | 4.5 (110) | 2 (60) | 1.8 (75) |
| Time to reintervention, mo | 11 | 4 | - | 66 | 3 |
| Mechanism of residual MR | Interclip | Commissural prolapse (lateral) | - | A3 prolapse+interclip | Commissural (medial)+central |
| Clips and position (2nd intervention) | None | None | - | MitraClip NT (A3-P3) | None |
| Plug implantation (2nd intervention) | AVP III 14 x 5mm inter-clip | AVP III 14 x 5mm lateral commissure | - | AVP III 14 x 5mm inter-clip | AVP III 14 x 5mm medial commissure |
| 2nd intervention duration, min | 85 | 26 | - | 157 | 102 |
| Residual MR (2nd intervention) | Mild to moderate | Mild to moderate | - | Trace | Moderate (central) |
| Mean gradient after the 2nd intervention, mmHg and HR, bpm | 2.8 (59) | 4.1 (69) | - | 1.7 (68) | 5.5 (81) |
| Maximal follow-up after plug implantation, mo | 34 | 11 | - | 3 | 3 |
| Residual MR (follow-up) | Mild to moderate | Moderate | - | Mild | Moderate |
| Mean gradient at follow-up, mmHg and HR, bmp | 2.9 (60) | 2.4 (67) | - | 1.8 (65) | 6 (90) |
HR, heart rate, MR, mitral regurgitation.
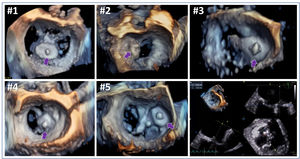
In all except 1 of the patients (n=4; 80%) AVP III implantation was delayed after M-TEER to promote clip stability after endothelization. Although 3 of these patients presented with acute MR (2 with hemodynamic instability), initial M-TEER was sufficient to stabilize and discharge them (one of them was stable for 5.5 years before requiring reintervention). For delayed interventions, AVP III was implanted (2 interclips and 2 commissural, figure 1) at least 3 months after the initial M-TEER. The intervention was planned with a baseline 3-dimensional measurement of the target area by 3-dimensional TEE (Figure 1 bottom right panel). All 4 interventions were successful with a good acute result that was maintained at the follow-up and with good clinical outcome and no hemolytic anemia (in 1 patient, #5, the residual MR was moderate but originated far from the plug implantation).
Three dimensional (3D) echocardiographic images of the mitral valve of the patients (#1 to #5) after AVP III implantation. Bottom right panel shows 3D measurements of the orifice to treat patient #2. Purple arrows point to the AVP III device. Pre- and postinterventional echocardiographic videos of patient #1 () and #2 () are available.
Patient #3 (n=1; 20%) presented with an acute MR secondary to massive flail of the posterior leaflet due to chordae rupture and cardiogenic shock. Although M-TEER was performed, severe residual MR in the medial commissure with hemodynamic instability required implantation of an additional AVP III during the same intervention. Despite initial technical and echocardiographic success, the device embolized in the left atrium within the first 24hours, requiring percutaneous extraction. The patient died during hospital admission due to hemodynamic instability and sepsis.
The longest interventions were those with clip and plug implantation during the same session (table 1).
In conclusion, the placement of an interclip or commissural AVP III occluder device after M-TEER may be a valid option for patients with challenging anatomies and significant symptomatic residual MR after M-TEER with no additional options. A 3-month delay between M-TEER and AVP III implantations seems to be reasonable to promote clip endothelization and avoid clip dislodgement or plug embolization. Further series will be needed to evaluate the short- and long-term results of these procedural alternative in complex mitral anatomies.
FUNDINGNo funding.
AUTORS’ CONTRIBUTIONSL. Sanchis and X. Freixa: conception and design. L. Sanchis, and C.I. Morr: data collection. L. Sanchis: drafting the manuscript. A. Regueiro, C.I. Morr, M. Sitges, X. Freixa: reviewing and editing the final version.
CONFLICTS OF INTERESTL. Sanchis, A. Regueiro, M. Sitges and X. Freixa are proctors for Abbott. M. Sitges has received consulting fees from Abbott. L Sanchis is associate editor of Rev Esp Cardiol. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2023.03.010