Quantification of cardiovascular risk has been based on scores such as Framingham, Framingham-REGICOR, SCORE or Life's Simple 7 (LS7). In vitro, animal, and randomized clinical studies have shown that polyphenols may provide benefits to the vascular system and reduce the inflammatory response. However, some clinical-epidemiological studies have yielded inconsistent results. Our aim was to assess the possible association between intake of the various polyphenol classes and established cardiovascular scores.
MethodsThis cross-sectional analysis involved 6633 PREDIMED-Plus study participants. Food polyphenol content was estimated by a semiquantitative food frequency questionnaire, adjusted for total energy intake according to the residual method. The association between polyphenol intake and cardiovascular risk was tested using linear regression analyses.
ResultsTotal polyphenol and flavonoid intake were directly and significantly associated only with the LS7 scale. Intake of lignans was directly and significantly associated with SCORE and LS7 scales, stilbene intake with SCORE, and phenolic acid intake with Framingham and Framingham-REGICOR scores. Other polyphenol classes were associated in a protective and significant manner in Framingham, SCORE and LS7 scores. In women, intake of all the polyphenol classes, except phenolic acids, showed a protective trend in the results of the Framingham, Framingham-REGICOR scores and LS7 scale.
ConclusionsAn inverse association was found between consumption of the ‘other polyphenols’ class and, especially among women, with estimated cardiovascular risk. The results were similar to those of Framingham, Framingham-REGICOR and LS7 (after eliminating the diet component) and differed from those of SCORE, but the predictors included were limited in the latter case.
Keywords
Cardiovascular disease (CVD) is the leading cause of death worldwide.1 It was estimated to cause 17.8 million deaths in 20172 and one third occurred in people younger than 70 years.1 There is clear evidence that intervention strategies have helped to reduce mortality trends but, despite this progress, CVD remains a public health challenge.3
The incidence of CVD is largely explained by several risk factors, mostly related to lifestyles, which are in turn potentially modifiable and susceptible to prevention. These includes cigarette smoking, low physical activity levels and unhealthy dietary patterns, all of which can contribute to high blood pressure, high body mass index (BMI), high total cholesterol levels, and high fasting plasma glucose levels.4 One of the dietary patterns which has shown benefits in relation to CVD is the Mediterranean diet.5 It is postulated that the beneficial effect of the Mediterranean diet is due to its richness in antioxidant and anti-inflammatory substances, especially polyphenols.5–11
Polyphenols are found in foods including fruits, cereals, vegetables, legumes and cocoa, and beverages such as coffee, tea, and wine.12 These compounds have been observed to show preventive properties against a wide variety of diseases, including CVD.13–15 In addition, many studies have shown that polyphenols may have protective effects in the vascular system and in reducing inflammatory responses.12,16
In epidemiological studies, the relationship between polyphenol intake and cardiovascular risk factors has been analyzed by various approaches.7,8,10,17 In almost all of these, an inverse relationship was observed between them, although results varied with regard to the polyphenol classes or subclasses. Nevertheless, the evidence is still too limited to lead to a recommendation for daily polyphenol intake.
The multifactorial nature of CVD events has led to the development of multivariable risk assessment tools or CVD risk scores,18 including Framingham,19 Framingham-REGICOR,20 and SCORE.21.The Life's Simple 7 (LS7)22 is an alternative to calculate optimal cardiovascular health and provide a new approach to the previous tools. There is wide variability between scores in terms of in the population on which they are based or in the traits they include, so they are not exempt from limitations and agreement problems.23
The aim of this study was to provide a new approach using different cardiovascular risk scores. Since the scores include cardiovascular risk factors (cholesterol, hypertension, smoking, diabetes, overweight/obesity, and other nonmodifiable factors such as age and sex), commonly gathered in the participants included in the PREDIMED-Plus trial, the aim was to assess the possible association between intake of different polyphenol classes and the Framingham, Framingham-REGICOR, SCORE and LS7 instruments.
METHODSStudy populationThis study was based on the cross-sectional analysis of the baseline data of participants included in PREDIMED-Plus. This is an ongoing 6-year multicenter, parallel-group, randomized trial, which is currently being conducted in 23 Spanish recruiting centers. The trial was registered at the International Standard Randomized Controlled Trial Registry (ISRCTN89898870). The study protocol includes more detailed information and is available in previous publications24–26 and at the ISRCT website.27
Participants consisted of women aged 60 to 75 years and men aged 55 to 75 years, with a BMI between 27.0 and 40.0kg/m2 and meeting at least 3 criteria for metabolic syndrome28 and with no CVD at enrolment. All participants provided written informed consent, and the study protocol and procedures were approved according to the ethical standards of the Declaration of Helsinki by all the participating institutions.
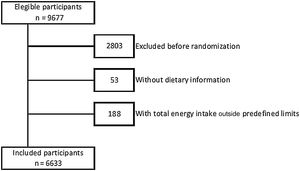
A total of 9677 people were contacted, of whom 6874 participants were eligible for the study, and were included in the trial. After exclusion of participants with missing data for the main variables and with implausible values for mean daily energy intake (< 500 and > 3500kcal/d for women, < 800 and > 4000kcal/d for men), 6633 participants were included in the present analysis (figure 1).
Variables and data collectionData on age, sex, educational level, anthropometric measurements, dietary habits, and lifestyle were collected at baseline. Anthropometric evaluations were measured according to the PREDIMED-Plus protocol. Physical activity was evaluated using the validated REGICOR Short Physical Activity Questionnaire,29 while the validated Spanish version of the Nurses’ Health Study questionnaire was used to assess sedentary behavior.30
Adherence to an energy-reduced Mediterranean diet was assessed with a 17-item questionnaire (17-item erMedDiet), which is a modified version of the previously validated questionnaire used in the PREDIMED trial.31
Information on sociodemographic and lifestyle habits, individual and family medical history, smoking status, medical conditions, and medication use was evaluated by self-reported questionnaires. Biochemical analyses were performed using overnight fasting blood samples by standard enzymatic methods. Low-density lipoprotein cholesterol was calculated using the Friedewald formula. Blood pressure was measured in triplicate with a validated semiautomatic oscillometer in a seated position.
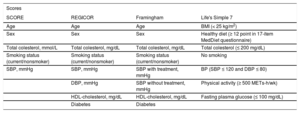
Variables included in the cardiovascular risk tools are shown in table 1, detailing their units. The LS7 scores each of 7 healthy habits favourably (plus 1 point).
Traits included in the estimation of the different cardiovascular risk scores
| Scores | |||
|---|---|---|---|
| SCORE | REGICOR | Framingham | Life's Simple 7 |
| Age | Age | Age | BMI (< 25 kg/m2) |
| Sex | Sex | Sex | Healthy diet (≥ 12 point in 17-item MedDiet questionnaire) |
| Total colesterol, mmol/L | Total colesterol, mg/dL | Total colesterol, mg/dL | Total colesterol (≤ 200 mg/dL) |
| Smoking status (current/nonsmoker) | Smoking status (current/nonsmoker) | Smoking status (current/nonsmoker) | No smoking |
| SBP, mmHg | SBP, mmHg | SBP with treatment, mmHg | BP (SBP ≤ 120 and DBP ≤ 80) |
| DBP, mmHg | SBP without treatment, mmHg | Physical activity (≥ 500 METs-h/wk) | |
| HDL-cholesterol, mg/dL | HDL-cholesterol, mg/dL | Fasting plasma glucose (≤ 100 mg/dL) | |
| Diabetes | Diabetes | ||
BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; HDL, high-density lipoprotein; SBP, systolic blood pressure.
Registered study dietitians assessed baseline diet with a semiuantitative 143-item food frequency questionnaire (FFQ),32 which has been previously validated in the Spanish population.33,34
Dietary intake of the aglycone forms of polyphenols was estimated from the European Phenol Explorer database.35This procedure standardizes the data of the results of different analytical methods and facilitates cross-study comparisons.36
Polyphenol intake was calculated in mg/d (without applying a retention factor) using food consumption data from the FFQ and the aglycone polyphenol content of each food contained in the Phenol Explorer database. The data from the Phenol Explorer contains information on polyphenol concentration obtained from both chromatography and chromatography after hydrolysis analytical methods.
Polyphenol intake values were adjusted for total energy according to the Willett residuals method37 to obtain intake of polyphenols, which is not correlated to total energy intake, and were categorized in sex-specific quintiles.
Statistical analysisDescriptive statistics were used to define participants’ baseline characteristics. Data are shown as mean and standard deviation (SD) and prevalence is expressed as frequency (No.) and percentage (%). The correlation between the scales was evaluated with Pearson pairwise correlations.
Linear regression models were carried out using CVD risk (Framingham, SCORE, Framingham-REGICOR and LS7) as the dependent variable and total polyphenol intake and the intake of their classes in quintiles as the independent variable.
The original risk equations were evaluated and, subsequently, the included CVD risk factors were eliminated from each equation one by one (total cholesterol, smoking status, BP, diabetes, and high-density lipoprotein cholesterol) and physical activity, BMI, healthy diet, and fasting plasma glucose were eliminated in the case of the LS7.
All regression models were stratified by sex and adjusted for recruiting center, intervention group, and cluster. Values are shown as beta coefficients and 95% confidence intervals (95%CI).
The analyses were performed with the Stata statistical software package version 15.1 (StataCorp LP, United States).
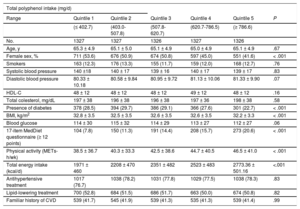
RESULTSTable 2 shows the main characteristics of the 6633 participants from the PREDIMED-Plus study according to quintiles of total dietary polyphenol intake. Participants included in the fifth quintile of polyphenol intake were mainly men, with the highest score in the 17-item MedDiet questionnaire and higher physical activity and energy dietary intake than in the other quintiles. In addition, participants in the fifth quintile had less diabetes and lower BMI than those in the other quintiles.
Baseline characteristics of the PREDIMED-Plus participants according to quintiles of polyphenol intake
| Total polyphenol intake (mg/d) | ||||||
|---|---|---|---|---|---|---|
| Range | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | P |
| (≤ 402.7) | (403.0-507.8) | (507.8-620.7) | (620.7-786.5) | (≥ 786.6) | ||
| No. | 1327 | 1327 | 1326 | 1327 | 1326 | |
| Age, y | 65.3 ± 4.9 | 65.1 ± 5.0 | 65.1 ± 4.9 | 65.0 ± 4.9 | 65.1 ± 4.9 | .67 |
| Female sex, % | 711 (53.6) | 676 (50.9) | 674 (50.8) | 597 (45.0) | 551 (41.6) | < .001 |
| Smokers | 163 (12.3) | 176 (13.3) | 155 (11.7) | 159 (12.0) | 168 (12.7) | .76 |
| Systolic blood pressure | 140 ±18 | 140 ± 17 | 139 ± 16 | 140 ± 17 | 139 ± 17 | .83 |
| Diastolic blood pressure | 80.33 ± 10.18 | 80.58 ± 9.84 | 80.95 ± 9.72 | 81.13 ± 10.06 | 81.33 ± 9.90 | .07 |
| HDL-C | 48 ± 12 | 48 ± 12 | 48 ± 12 | 49 ± 12 | 48 ± 12 | .16 |
| Total colesterol, mg/dL | 197 ± 38 | 196 ± 38 | 196 ± 38 | 197 ± 36 | 198 ± 38 | .58 |
| Presence of diabetes | 378 (28.5) | 394 (29.7) | 386 (29.1) | 366 (27.6) | 301 (22.7) | < .001 |
| BMI, kg/m2 | 32.8 ± 3.5 | 32.5 ± 3.5 | 32.6 ± 3.5 | 32.6 ± 3.5 | 32.2 ± 3.3 | < .001 |
| Blood glucose | 114 ± 30 | 115 ± 32 | 114 ± 29 | 113 ± 27 | 112 ± 27 | .06 |
| 17-item MedDiet questionnaire (≥ 12 points) | 104 (7.8) | 150 (11.3) | 191 (14.4) | 208 (15.7) | 273 (20.6) | < .001 |
| Physical activity (METs-h/wk) | 38.5 ± 36.7 | 40.3 ± 33.3 | 42.5 ± 38.6 | 44.7 ± 40.5 | 46.5 ± 41.0 | < .001 |
| Total energy intake (kcal/d) | 1971 ± 460 | 2208 ± 470 | 2351 ± 482 | 2523 ± 483 | 2773.36 ± 501.16 | <.001 |
| Antihypertensive treatment | 1017 (76.7) | 1038 (78.2) | 1031 (77.8) | 1029 (77.5) | 1038 (78.3) | .83 |
| Lipid-lowering treatment | 700 (52.8) | 684 (51.5) | 686 (51.7) | 663 (50.0) | 674 (50.8) | .82 |
| Familiar history of CVD | 539 (41.7) | 545 (41.9) | 539 (41.3) | 535 (41.3) | 539 (41.4) | .99 |
BMI, body mass index; CVD, cardiovascular disease; HDL-C, high-density lipoprotein cholesterol.
The data are expressed as No. (%) or mean ± standard deviation.
The 4 scores were statistically significantly correlated (P < .001): the coefficient was 0.849 for Framingham and Framingham-REGICOR, 0.731 for Framingham and SCORE, −0.309 Framingham and LS7 was, 0.602 for Framingham-REGICOR and SCORE, −0.333 for Framingham-REGICOR and LS7, and −0.249 for SCORE and LS7.
The associations between the energy-adjusted dietary intake of polyphenols and cardiovascular risk for the different risk equations are shown in table 3 and in the . Total polyphenol and flavonoid intake were only directly and significantly associated with the LS7 scale. Total polyphenol and flavonoid intake were only directly and significantly associated with the LS7 scale. Regarding Q1 of total polyphenol intake, the participants in Q5 showed an improvement in cardiovascular health of 10% (βQ5vs.Q1 = 0.10; 95%CI, 0.04-0.17). For those in Q5 of flavonoid intake, the improvement in cardiovascular health was 17% (βQ5vs.Q1 = 0.17; 95%CI, 0.10-0.24). Similarly, Q5 intake of lignans (in relation to Q1) was associated with an increase in the risk of cardiovascular death of 48% (SCORE: βQ5vs.Q1 = 0.48; 95%CI, 0.25-0.71) and with an increase in cardiovascular health of 23% (LS7: βQ5vs.Q1 = 0.23; 95%CI, 0.16-0.30). The Q5 intake in stilbenes was associated with a 38% increase in the risk of cardiovascular death (SCORE: βQ5vs.Q1 = 0.38; 95%CI, 0.15-0.62), Q5 intake of phenolic acids with a 191% increase in total CVD risk (Framingham: βQ5vs.Q1 = 1.91; 95%CI, 0.76-3.06) and with a 27% increase in coronary risk (Framingham-REGICOR: βQ5vs.Q1 = 0.27; 95%CI, 0.00-0.54). Intake of other polyphenols was significantly associated in Framingham (βQ5vs.Q1 = −1.22; 95%CI, −2.37 to −0.07) and SCORE (βQ5vs.Q1 = −0.32; 95%CI, −0.55 to −0.08), decreasing total CVD risk by 122% and coronary risk by 8%, respectively.
Association between polyphenol intake and cardiovascular risk scores stratified by sex in the PREDIMED-Plus trial
| Polyphenol intake | Framingham quintile 5 vs quintile 1 | Framingham-REGICOR quintile 5 vs quintile 1 | ||||
|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | |
| Flavonoids | −0.71 (−1.86; 0.43) (P = .222) | −0.02 (−1.61; 1.57) (P = .980) | −1.52 (−2.57; −0.47) (P = .005) | −0.13 (−0.39; 0.14) (P = .344) | 0.17 (−0.24; 0.57) (P = .418) | −0.45 (−0.71; −0.19) (P < .001) |
| Lignans | 0.56 (−0.59; 1.71) (P = .341) | 1.41 (−0.18; 3.00) (P = .083) | −0.31 (−1.37; 0.74) (P = .558) | 0.04 (−0.23; 0.31) (P = .773) | 0.40 (−0.01; 0.80) (P = .054) | −0.34 (−0.60; −0.08) (P = .009) |
| Stilbenes | 0.15 (−1.00; 1.30) (P = .798) | 0.97 (−0.62; 2.56) (P = .231) | −0.65 (−1.70; 0.41) (P = .230) | −0.1 (−0.36; 0.17) (P = .472) | 0.25 (−0.15; 0.66) (P = .218) | −0.47 (−0.73; −0.21) (P < .001) |
| Phenolic acids | 1.91 (0.76; 3.06) (P < .001) | 2.79 (1.20; 4.37) (P < .001) | 0.85 (−0.20; 1.90) (P = .114) | 0.27 (0.00; 0.54) (P = .047) | 0.38 (−0.02; 0.79) (P = .063) | 0.13 (−0.13; 0.39) (P = .340) |
| Other polyphenols | −1.22 (−2.37; −0.07) (P = .038) | −0.75 (−2.34; 0.84) (P = .353) | −1.79 (−2.84; −0.73) (P < .001) | −0.17 (−0.44; 0.09) (P = .202) | 0.08 (−0.32; 0.49) (P = .688) | −0.46 (−0.72; −0.20) (P < .001) |
| Total Polyphenols | −0.13 (−1.28; 1.02) (P = .823) | 0.97 (−0.62; 2.56) (P = .230) | −1.40 (−2.45; −0.35) (P = .009) | −0.02 (−0.29; 0.25) (P = .879) | 0.42 (0.01; 0.82) (P = .043) | −0.50 (−0.76; −0.24) (P < .001) |
| Polyphenol intake | SCORE quintile 5 vs quintile 1 | Life's Simple 7 quintile 5 vs quintile 1 | ||||
|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | |
| Flavonoids | 0.12 (−0.12; 0.35) (P = .328) | 0.31 (−0.05; 0.68) (P = .088) | −0.12 (−0.36; 0.12) (P = .335) | 0.17 (0.10; 0.24) (P < .001) | 0.18 (0.09; 0.27) (P < .001) | 0.23 (0.13; 0.33) (P < .001) |
| Lignans | 0.48 (0.25; 0.71) (P < .001) | 0.73 (0.37; 1.09) (P < .001) | 0.19 (−0.05; 0.43) (P = .128) | 0.23 (0.16; 0.30) (P < .001) | 0.23 (0.14; 0.33) (P < .001) | 0.28 (0.18; 0.38) (P < .001) |
| Stilbenes | 0.38 (0.15; 0.62) (P < .001) | 0.64 (0.28; 1.00) (P < .001) | 0.13 (−0.12; 0.37) (P = .314) | 0.03 (−0.04; 0.1) (P = .220) | −0.04 (−0.14; 0.05) (P = .366) | 0.13 (0.03; 0.24) (P = .009) |
| Phenolic acids | 0.02 (−0.22; 0.25) (P = .899) | −0.01 (−0.37; 0.35) (P = .949) | 0.03 (−0.21; 0.27) (P = .813) | −0.03 (−0.10; 0.03) (P = .191) | −0.06(−0.16; 0.03) (P = .169) | −0.03 (−0.13; 0.07) (P = .605) |
| Other polyphenols | −0.32 (−0.55; −0.08) (P = .008) | −0.30 (−0.66;0.06) (P = .102) | −0.32 (−0.56;−0.08) (P = .010) | 0.06 (−0.01; 0.12) (P < .001) | 0.11 (0.02; 0.21) (P = .015) | 0.19 (0.09; 0.29) (P < .001) |
| Total polyphenols | 0.10 (−0.13; 0.34) (P = .384) | 0.29 (−0.70; 0.65) (P = .114) | −0.13 (−0.37; 0.12) (P = .300) | 0.10 (0.04; 0.17) (P < .001) | 0.11 (0.01; 0.20) (P = .024) | 0.20 (0.10; 0.30) (P < .001) |
The table shows the adjusted mean difference in the cardiovascular risk scores for the 5th vs the 1st quintile of polyphenol intake and the P for trend. The data are expressed as beta coefficients and 95% confidence intervals. Results from multivariable linear regression models adjusted for recruiting center, intervention group, and cluster.
For the stratified analysis by sex, in women, the intake of all the polyphenol classes, except phenolic acids, showed an indirect association in the results of the Framingham and Framingham-REGICOR scores and a direct association in the LS7 scale. Other polyphenol intake also showed the same result for the SCORE equation. In men, total polyphenol intake was directly associated with the Framingham-REGICOR and LS7 equations. Intake of lignans was directly associated with SCORE and LS7 equations, stilbene intake with SCORE, and intake of other polyphenols with the LS7 scale.
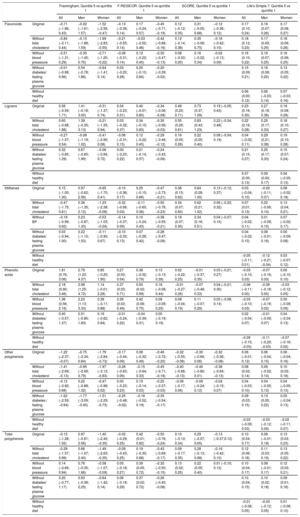
Table 4 shows the main results derived from linear regression models after removal of 1 risk factor at a time from each score. In general, for Framingham, Framingham-REGICOR and SCORE, the inverse associations were maintained even if some risk factors were not taken into account in the equations (for Framingham and Framingham-REGICOR in flavonoids and total polyphenols, and for the 3 equations in other polyphenols). The direct association was reversed in Framingham and Framingham-REGICOR equations when blood pressure was eliminated for lignans and, in Framingham for stilbenes when cholesterol, blood pressure and diabetes were removed. The best cardiovascular health (higher score on LS7 scale) was found when consumption of all polyphenol classes (except for phenolic acids) was highest, regardless of removing traits from the equation, except when a healthy diet was removed.
Sensitivity analyses for the association between polyphenol intake and cardiovascular risk scores stratified by sex
| Framingham. Quintile 5 vs quintile 1 | F-REGICOR. Quintile 5 vs quintile 1 | SCORE. Quintile 5 vs quintile 1 | Life's Simple 7. Quintile 5 vs quintile 1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | All | Men | Women | All | Men | Women | ||
| Flavonoids | Original | −0.71 (−1.86; 0.43) | −0.02 (−1.61; 1.57) | −1.52 (−2.56; −0.47) | −0.13 (−0.39; 0.14) | 0.17 (−0.24; 0.57) | −0.45 (−0.71; −0.19) | 0.12 (−0.12; 0.35) | 0.31 (−0.05; 0.68) | −0.12 (−0.36; 0.12) | 0.17 (0.10; 0.24) | 0.16 (0.07; 0.26) | 0.17 (0.08; 0.27) |
| Without total cholesterol | −0.84 (−2.11; 0.44) | −0.15 (−1.88; 1.59) | −1.69 (−2.83; −0.55) | −0.21 (−0.55; 0.14) | −0.03 (−0.52; 0.46) | −0.42 (−0.68; −0.16) | 0.12 (−0.14; 0.38) | 0.35 (−0.06; 0.75) | −0.16 (−0.42; 0.10) | 0.18 (0.12; 0.23) | 0.17 (0.09; 0.25) | 0.18 (0.09; 0.26) | |
| Without blood preassure | −0.51 (−1.31; 0.29) | −0.35 (−1.45; 0.76) | −0.71 (−1.20; −0.22) | −0.08 (−0.31; 0.14) | 0.12 (−0.22; 0.45) | −0.30 (−0.47; −0.13) | 0.08 (−0.03; 0.20) | 0.16 (−0.02; 0.34) | −0.02 (−0.13; 0.09) | 0.16 (0.10; 0.22) | 0.16 (0.07; 0.25) | 0.16 (0.06; 0.25) | |
| Without diabetes/ fasting plasma glucose | −0.01 (−0.98; 0.96) | 0.54 (−0.78; 1.86) | −0.64 (−1.41; 0.14) | 0.03 (−0.20; 0.26) | 0.25 (−0.10; 0.60) | −0.20 (−0.39; −0.02) | 0.15 (0.09; 0.21) | 0.16 (0.08; 0.25) | 0.13 (0.05; 0.22) | ||||
| Without healthy diet | 0.06 (0.00; 0.12) | 0.06 (−0.03; 0.14) | 0.07 (−0.03; 0.16) | ||||||||||
| Lignans | Original | 0.56 (−0.59; 1.71) | 1.41 (−0.18; 3.00) | −0.31 (−1.37; 0.74) | 0.04 (−0.23; 0.31) | 0.40 (−0.01; 0.80) | −0.34 (−0.06; −0.08) | 0.48 (0.25; 0.71) | 0.73 (0.37; 1.09) | 0.19 (−0.05; 0.43) | 0.23 (0.16; 0.30) | 0.27 (0.18; 0.36) | 0.18 (0.08; 0.28) |
| Without total cholesterol | 0.60 (−0.68; 1.88) | 1.39 (−0.35; 3.13) | −0.21 (−1.35; 0.94) | 0.03 (−0.32; 0.37) | 0.34 (−0.15; 0.83) | −0.30 (−0.56; −0.03) | 0.55 (0.29; 0.81) | 0.83 (0.43; 1.23) | 0.22 (−0.04; 0.48) | 0.22 (0.16; 0.28) | 0.25 (0.17; 0.33) | 0.18 (0.10; 0.27) | |
| Without blood preassure | −0.27 (−1.07; 0.54) | −0.08 (−1.19; 1.02) | −0.41 (−0.90; 0.08) | −0.08 (−0.31; 0.15) | 0.12 (−0.22; 0.45) | −0.29 (−0.46; −0.12) | 0.16 (0.05; 0.28) | 0.22 (0.05; 0.40) | 0.08 (−0.04; 0.19) | 0.04 (−0.02; 0.11) | 0.29 (0.21; 0.38) | 0.19 (0.10; 0.28) | |
| Without diabetes/ fasting plasma glucose | 0.32 (−0.65; 1.29) | 0.67 (−0.65; 1.99) | −0.06 (−0.84; 0.72) | 0.00 (−0.23; 0.22) | 0.21 (−0.14; 0.57) | −0.24 (−0.43; −0.06) | 0.21 (0.15; 0.27) | 0.25 (0.17; 0.33) | 0.15 (0.07; 0.24) | ||||
| Without healthy diet | 0.07 (0.00; 0.13) | 0.09 (0.00; 0.17) | 0.04 (−0.05; 0.13) | ||||||||||
| Stilbenes | Original | 0.15 (−1.00; 1.30) | 0.97 (−0.62; 2.56) | −0.65 (−1.70; 0.41) | −0.10 (−0.36; 0.17) | 0.25 (−0.15; 0.66) | −0.47 (−0.73; −0.21) | 0.38 (0.15; 0.62) | 0.64 (0.28; 1.00) | 0.13 (−0.12; 0.37) | 0.03 (−0.04; 0.10) | −0.02 (−0.11; 0.07) | 0.08 (−0.02; 0.18) |
| Without total cholesterol | −0.47 (−1.75; 0.81) | 0.38 (−1.35; 2.12) | −1.23 (−2.38; −0.08) | −0.32 (−0.66; 0.03) | −0.11 (−0.60; 0.38) | −0.50 (−0.76; −0.23) | 0.34 (0.07; 0.60) | 0.62 (0.21; 1.02) | 0.06 (−0.20; 0.32) | 0.07 (0.01; 0.13) | 0.02 (−0.06; 0.10) | 0.13 (0.04; 0.21) | |
| Without BP | −0.19 (−0.99; 0.62) | 0.23 (−0.87; 1.33) | −0.53 (−1.03; −0.04) | −0.14 (−0.37; 0.09) | 0.10 (−0.24; 0.43) | −0.38 (−0.55; −0.21) | 0.18 (0.07; 0.30) | 0.34 (0.16; 0.51) | 0.04 (−0.07; 0.15) | 0.04 (−0.02; 0.11) | 0.01 (−0.08; 0.10) | 0.07 (−0.02; 0.17) | |
| Without diabetes/ fasting plasma glucose | 0.03 (−0.94; 1.00) | 0.22 (−1.10; 1.53) | −0.11 (−0.90; 0.67) | −0.10 (−0.33; 0.13) | 0.07 (−0.28; 0.42) | −0.28 (−0.47; −0.09) | 0.04 (−0.02; 0.10) | 0.08 (−0.01; 0.16) | 0.00 (−0.09; 0.08) | ||||
| Without healthy diet | −0.05 (−0.11; 0.01) | −0.12 (−0.21; −0.04) | 0.03 (−0.07; 0.12) | ||||||||||
| Phenolic acids | Original | 1.91 (0.76; 3.06) | 2.79 (1.20; 4.37) | 0.85 (−0.20; 1.90) | 0.27 (0.00; 0.54) | 0.38 (−0.02; 0.79) | 0.13 (−0.13; 0.39) | 0.02 (−0.22; 0.25) | −0.01 (−0.37; 0.35) | 0.03 (−0.21; 0.27) | −0.03 (−0.10; 0.03) | −0.07 (−0.16; 0.03) | 0.00 (−0.10; 0.10) |
| Without total cholesterol | 2.18 (0.90; 3.46) | 2.98 (1.25; 4.72) | 1.14 (−0.01; 2.28) | 0.37 (0.03; 0.71) | 0.50 (0.02; 0.99) | 0.18 (−0.08; 0.44) | −0.01 (−0.27; 0.26) | −0.07 (−0.48; 0.33) | 0.04 (−0.21; 0.30) | −0.06 (−0.11; 0.00) | −0.08 (−0.16; 0.00) | −0.03 (−0.12; 0.05) | |
| Without blood preassure | 1.36 (0.56; 2.16) | 2.23 (1.13; 3.33) | 0.39 (−0.11; 0.88) | 0.26 (0.03; 0.49) | 0.42 (0.08; 0.75) | 0.08 (−0.09; 0.25) | 0.08 (−0.04; 0.19) | 0.11 (−0.07; 0.29) | 0.03 (−0.08; 0.14) | −0.03 (−0.10; 0.03) | −0.07 (−0.16; 0.02) | 0.00 (−0.09; 0.09) | |
| Without diabetes/ fasting plasma glucose | 0.40 (−0.57; 1.37) | 0.51 (−0.80; 1.83) | 0.16 (−0.62; 0.94) | −0.01 (−0.24; 0.22) | −0.04 (−0.39; 0.31) | 0.00 (−0.19; 0.19) | 0.02 (−0.04; 0.07) | −0.01 (−0.09; 0.07) | 0.04 (−0.04; 0.13) | ||||
| Without healthy diet | −0.09 (−0.15; −0.03) | −0.11 (−0.20; −0.03) | −0.07 (−0.16; 0.02) | ||||||||||
| Other polyphenols | Original | −1.22 (−2.37; −0.07) | −0.75 (−2.34; 0.84) | −1.79 (−2.84; −0.73) | −0.17 (−0.44; 0.09) | 0.08 (−0.32; 0.49) | −0.46 (−0.72; −0.20) | −0.32 (−0.55; −0.08) | −0.30 (−0.66; 0.06) | −0.32 (−0.56; −0.08) | 0.06 (−0.01; 0.12) | 0.06 (−0.04; 0.15) | 0.06 (−0.04; 0.16) |
| Without total cholesterol | −1.41 (−2.69; −0.13) | −0.95 (−2.69; 0.79) | −1.97 (−3.12; −0.83) | −0.28 (−0.63; 0.06) | −0.15 (−0.64; 0.33) | −0.45 (−0.71; −0.18) | −0.40 (−0.66; −0.13) | −0.40 (−0.80; 0.01) | −0.38 (−0.64; −0.13) | 0.08 (0.02; 0.14) | 0.06 (−0.02; 0.14) | 0.10 (0.02; 0.18) | |
| Without blood preassure | −0.12 (−0.92; 0.68) | 0.22 (−0.88; 1.32) | −0.47 (−0.96; 0.02) | 0.00 (−0.23; 0.23) | 0.19 (−0.14; 0.53) | −0.20 (−0.37; −0.03) | −0.06 (−0.17; 0.06) | −0.06 (−0.24; 0.12) | −0.04 (−0.15; 0.07) | 0.04 (−0.03; 0.10) | 0.04 (−0.05; 0.13) | 0.04 (−0.05; 0.13) | |
| Without diabetes / fasting plasma glucose | −1.62 (−2.59; −0.64) | −1.77 (−3.09; −0.45) | −1.51 (−2.29; −0.73) | −0.25 (−0.48; −0.02) | −0.16 (−0.52; 0.19) | −0.35 (−0.54; −0.17) | 0.09 (0.03; 0.15) | 0.13 (0.05; 0.22) | 0.05 (−0.04; 0.13) | ||||
| Without healthy diet | −0.03 (−0.09; 0.03) | −0.03 (−0.12; 0.05) | −0.02 (−0.11; 0.07) | ||||||||||
| Total polyphenols | Original | −0.13 (−1.28; 1.02) | 0.97 (−0.61; 2.56) | −1.40 (−2.45; −0.35) | −0.02 (−0.29; 0.25) | 0.42 (0.01; 0.82) | −0.50 (−0.76; −0.24) | 0.10 (−0.13; 0.34) | 0.29 (−0.07; 0.65) | −0.13 (−0.37;0.12) | 0.10 (0.04; 0.17) | 0.08 (−0.01; 0.18) | 0.13 (0.03; 0.23) |
| Without total cholesterol | −0.29 (−1.57; 0.99) | 0.66 (−1.07; 2.40) | −1.49 (−2.63; −0.35) | −0.09 (−0.43; 0.25) | 0.19 (−0.30; 0.68) | −0.43 (−0.69; −0.17) | 0.09 (−0.17; 0.35) | 0.28 (−0.13; 0.68) | −0.16 (−0.42; 0.10) | 0.12 (0.06; 0.18) | 0.11 (0.03; 0.19) | 0.13 (0.05; 0.22) | |
| Without blood preassure | 0.14 (−0.66; 0.94) | 0.76 (−0.35; 1.86) | −0.58 (−1.07; −0.09) | 0.05 (−0.18; 0.27) | 0.39 (0.05; 0.72) | −0.32 (−0.50; −0.15) | 0.13 (0.02; 0.25) | 0.22 (0.05; 0.40) | 0.01 (−0.10; 0.12) | 0.10 (0.04; 0.17) | 0.08 (−0.01; 0.17) | 0.12 (0.03; 0.21) | |
| Without diabetes/ fasting plasma glucose | 0.20 (−0.77; 1.17) | 0.93 (−0.38; 2.25) | −0.64 (−1.42; 0.14) | 0.06 (−0.16; 0.29) | 0.37 (0.02; 0.72) | −0.26 (−0.45; −0.08) | 0.10 (0.04; 0.15) | 0.10 (0.02; 0.18) | 0.09 (0.01; 0.18) | ||||
| Without healthy diet | −0.01 (−0.08; 0.05) | −0.03 (−0.12; 0.05) | 0.01 (−0.08; 0.10) | ||||||||||
The table shows the adjusted mean difference in the cardiovascular risk scores for the 5th vs the 1st quintile of polyphenol intake. The data are expressed as beta coefficients and 95% confidence intervals. Results from multivariable linear regression models adjusted for recruiting centre, intervention group and cluster.
In this cross-sectional study, we evaluated the relationship between intake of different polyphenol classes and estimated cardiovascular risk measured with different tools in the cohort of the PREDIMED-Plus trial.
Previous evidence, mainly from in vivo or in vitro studies, suggests that polyphenol intake reduces CVD probably due to their anti-inflammatory effect, since they lower blood pressure, protect pancreatic cells, improve insulin resistance, inhibit platelet aggregation, reduce very low-density lipoprotein, reduce plasma triglyceride levels, improve nitric oxide homeostasis, antagonize atherogenesis, and improve atherosclerosis.12,38
A few previous studies have evaluated the association between the Mediterranean diet39 and other dietary patterns40 with cardiovascular risk but none has evaluated the association between polyphenol intake and overall cardiovascular risk measured by risk equations. Previous reports were of associations with individual cardiovascular risk factors, mostly focused on the flavonoid family41 and on components of the metabolic syndrome.42–44
Our results are consistent with those already published from the PREDIMED-Plus trial9,10 in which intake of stilbenes and lignans showed a direct association, while intake of flavonoids and other polyphenols showed an inverse association with systolic and diastolic blood pressure. All polyphenol classes were directly associated with high-density lipoprotein cholesterol. The direct association between phenolic acids with the equations and their inverse association with LS7 could also be seen in the aforementioned study,10 in which this family showed a direct and significant association with fasting plasma glucose and, in another study, with higher levels of low-density lipoprotein cholesterol.45 However, another study reported that phenolic acids showed an inverse association with blood pressure, glucose and lipid metabolism, as well as a stronger independent association with metabolic syndrome.42 The main source of phenolic acids in our participants was coffee,10 and some studies have suggested a J-shape relationship between coffee and cardiovascular risk,45,46 which could partly explain the inconclusive results.
Other polyphenol intakes showed a tendency for a protective effect against CVD risk measured by all scores. One of the main sources of these polyphenols in our participants were olives and olive oil,10 which have shown health benefits, mainly attributable to their polyphenol content, which include improvements in lipid profile, insulin sensitivity and endothelial function, as well as antiatherosclerotic and antithrombotic properties.47,48
Interestingly, in the analyses stratified by sex a stronger protective trend was observed in women (except for the phenolic acid family) and, in most cases, results were statistically significant and in the opposite direction than for men. In general, the effects of the Mediterranean diet appear to be greater in men than in premenopausal women when cardiometabolic changes are considered,49 although in this trial the women were postmenopausal. However, the results of the present study are in line with those previously observed in the trial.10 Another study also reported that consumption of foods rich in flavonoids was inversely associated with cardiovascular risk factors in premenopausal women but not in men.50 As in the aforementioned publication, men's habits may have changed due to diagnosis of high cardiovascular risk. In fact, men showed higher CVD risks, measured with all scales, than women. Therefore, reverse causality may have taken place.
Regarding risk equations, the results were concordant for Framingham, Framingham-REGICOR, and LS7. The SCORE equation has shown direct associations with the intake of all the polyphenol classes (except for other polyphenols in all participants and flavonoids and total polyphenols in women).
Differences between polyphenol classes were assessed by a sensitivity analysis. The healthy diet (adherence to the Mediterranean diet) was eliminated from the LS7 scale to check whether the direct association was due to the correlation between diet and polyphenols. In many cases, the direct association was maintained, although in others (stilbenes, other polyphenols, total polyphenols) the association became inverse. The latter suggests that this scale was in harmony with the results shown in the rest of the scores.
In the present study, the 4 scales showed a significant correlation, in addition to showing similar results when they were related to polyphenol intake. Although no studies have been found that compared the equations in this way, those that compared them with each other have shown variation between these scores. The main differences or limitations of these equations are the variables included and the ages for which they were designed. In addition, the risks measured are different, since Framingham addresses total CVD risk, REGICOR addresses coronary risk, SCORE addresses cardiovascular mortality and LS7 measures cardiovascular health. Discrepancies in the detection of high risk have also been shown, specifically, SCORE and Framingham classify different patients as high risk51 and REGICOR classifies fewer individuals as high risk than SCORE.52 In general, most equations work similarly in terms of discrimination, but calibration can vary widely, depending mostly on the population to which it is applied.53
Limitations and strengthsWe acknowledge that our study may have some limitations. First, and given the cross-sectional design of the study, there is a problem in determining the temporal relationship of a presumed cause and effect. Moreover, our entire study population is at high cardiovascular risk due to the trial protocol. Furthermore, the outcome is not an event, but an estimate of cardiovascular risk and the equations take into account factors that cannot be influenced by polyphenol intake (eg, age, sex, smoking status) and others that have shown benefits (eg, total cholesterol, high-density lipoprotein cholesterol, blood pressure). SCORE is the equation that includes most of these factors. In addition, no adjustment for lifestyle or other dietary factors was made, to compare the results for the equations with others, although LS7 includes physical activity and the results between them were similar. Another limitation is that self-reported dietary information may have led to some misclassification. However, the FFQ used was previously validated in the adult Spanish population and showed good reproducibility and validity.29 Finally, other factors affecting polyphenol content could be a limitation: the estimation of their intake through the FFQ, the differences in their absorption and in their bioactivity,54 the synergies with other polyphenols, nutrients or compounds,55 factors related to climate stress, geography, and storage conditions or losses during cooking.56 In addition, polyphenols were grouped instead of considering only individual compounds and therefore important associations for individual compounds may have been missed.
On the other hand, our study also has important strengths, such as its multicenter design, the large sample size and the high-quality, detailed information collected by qualified interviewers. Second, our database was built including all available information on polyphenol content in Phenol Explorer, with a mixture of data extracted from chromatography and chromatography after hydrolysis data and this consumption was adjusted using the residuals method. In addition, 4 different scores were used to assess cardiovascular risk, since CVD is a multifactorial disease and we found similar results between the scores. The strength of these findings was reinforced by the results obtained from the sensitivity analysis. Another strength of this study is the analysis stratified by sex, allowing us to detect differences with the overall analysis. Finally, this is the first study to evaluate the influence of polyphenol intake on cardiovascular risk as measured by these 4 different risk equations. The lack of epidemiologic studies precluded us from comparing our results with those of other studies.
CONCLUSIONSThis study shows the association between polyphenol classes and global cardiovascular risk, showing an inverse association between the class of other polyphenols and especially among women. The results were similar for Framingham, Framingham-REGICOR and LS7 (after eliminating diet). SCORE showed different results, but the predictors considered in this equation are limited and do not include some important ones such as diabetes or high-density lipoprotein cholesterol, while it includes other traits with which polyphenols may have no associations.
FUNDINGThe PREDIMED-Plus trial was supported by the official funding agency for biomedical research of the Spanish government, ISCIII, through the Fondo de Investigación para la Salud (FIS), which is cofunded by the European Regional Development Fund (5 coordinated FIS projects led by J. Salas-Salvadó and J. Vidal, including the following projects: PI13/00673, PI13/00492, PI13/00272, PI13/01123, PI13/00462, PI13/00233, PI13/02184, PI13/00728, PI13/01090, PI13/01056, PI14/01722, PI14/00636, PI14/00618, PI14/00696, PI14/01206, PI14/01919, PI14/00853, PI14/01374, PI14/00972, PI14/00728, PI14/01471, PI16/00473, PI16/00662, PI16/01873, PI16/01094, PI16/00501, PI16/00533, PI16/00381, PI16/00366, PI16/01522, PI16/01120, PI17/00764, PI17/01183, PI17/00855, PI17/01347, PI17/00525, PI17/01827, PI17/00532, PI17/00215, PI17/01441, PI17/00508, PI17/01732, PI17/00926, PI19/00957, PI19/00386, PI19/00309, PI19/01032, PI19/00576, PI19/00017, PI19/01226, PI19/00781, PI19/01560, and PI19/01332), the Especial Action Project entitled: Implementación y evaluación de una intervención intensiva sobre la actividad física Cohorte PREDIMED-Plus grant to J. Salas-Salvadó, the European Research Council (Advanced Research Grant 2013–2018, 340918) to M.Á. Martínez-González, the Recercaixa Grant to J. Salas-Salvadó (2013ACUP00194), CICYT [AGL2016- 75329-R], a grant from the Generalitat Valenciana (APOSTD/2019/136 to RB) and Generalitat de Catalunya (SGR-2019 to RE), grants from the Consejería de Salud de la Junta de Andalucía (PI0458/2013, PS0358/2016, and PI0137/2018), grants from the Generalitat Valenciana (PROMETEO/2017/017), a SEMERGEN Grant, EU-COST Action CA16112, a grant of support to research groups no. 35/2011 from the Balearic Islands Government, Grants from Balearic Islands Health Research Institute (IDISBA), funds from the European Regional Development Fund (CIBEROBN CB06/03 and CB12/03) and from the European Commission (EAT2BENI-CE_H2020_SFS2016). The Spanish Ministry of Science, Innovation and Universities for the Formación de Profesorado Universitario (FPU17/06488 and FPU17/00785) contract. The funding sponsors had no role in the design of the study, in the collection, analyses, or interpretation of the data, in the writing of the manuscript, or in the decision to publish the results.
AUTHORS’ CONTRIBUTIONSConceptualization: M. Rubín-García, F. Vitelli-Storelli, E. Toledo and V. Martín. Methodology: M. Rubín-García, F. Vitelli-Storelli, E. Toledo, S. Castro-Barquero, A. Tresserra-Rimbau and V. Martín-Sánchez. Formal analysis: M. Rubín-García, E. Toledo and V. Martín-Sánchez. Drafting and preparation of the draft: M. Rubín-García. Review and edition; M. Rubín-García, F. Vitelli-Storelli, E. Toledo, S. Castro-Barquero, A. Tresserra-Rimbau, M.A. Martínez-González, J. Salas-Salvadó, D. Corella, A. Hernáez, J.A. Martínez, A.M. Alonso-Gómez, J. Wärnberg, J. Vioque, D. Romaguera, J. López-Miranda, R. Estruch, M.R. Bernal-López, J. Lapetra, L. Serra-Majem, A. Bueno-Cavanillas, J.A. Tur, L. Álvarez-Álvarez, X. Pintó, J.J. Gaforio, P. Matía-Martín, J. Vidal, C. Vázquez, L. Daimiel, E. Ros, A. Gea, J.J. Manzanares, J.V. Sorlí, H. Schröder, I. Abete, L. Tojal-Sierra, E. Crespo-Oliva, A. González-Botella, E. Rayó, A. García-Rios, A.M. Gómez-Pérez, J.M. Santos-Lozano, R. Bartolomé-Resano, M.M. Murphy, C. Ortega-Azorin, C. Medrano, M.A. Zulet, C. Sorto-Sanchez, N. Babio, M. Fitó, R.M. Lamuela-Raventós and V. Martín-Sánchez; Project management: E. Toledo, M.A. Martínez-González, J. Salas-Salvadó, D. Corella, J.A. Martínez, A.M. Alonso-Gómez, J. Wärnberg, J.Vioque, D. Romaguera, J. López-Miranda, R. Estruch, M.R. Bernal-López, J. Lapetra, J.L. Serra-Majem, A. Bueno-Cavanillas, J.A. Tur, X. Pintó, J.J. Gaforio, P. Matía-Martín, J. Vidal, C. Vázquez, L. Daimiel, E. Ros, H. Schröder, N. Babio, M. Fitó, R.M. Lamuela-Raventós, and V. Martín-Sánchez. Supervision: F. Vitelli-Storelli, E. Toledo, and V. Martín-Sánchez. Funding acquisition: E. Toledo, M.A. Martínez-González, J. Salas-Salvadó, D. Corella, J.A. Martínez, A.M. Alonso-Gómez, J. Wärnberg, J. Vioque, D. Romaguera, J. López-Miranda, R. Estruch, M.R. Bernal-López, J. Lapetra, J.L. Serra-Majem, A. Bueno-Cavanillas, J.A. Tur, X. Pintó, J.J. Gaforio., P. Matía-Martín, J. Josep Vidal, C. Vázquez, L. Daimiel, E. Ros, H. Schröder, N. Babio, M. Fitó, R.M. Lamuela-Raventós, and V. Martín-Sánchez. All authors have read and accepted the final version of the manuscript.
- -
Polyphenols have shown benefits in improving cardiovascular risk factors, but the evidence is still too limited to support a recommendation for daily polyphenol intake for cardiovascular disease prevention.
- -
So far, no study has been found that relates polyphenol intake with the cardiovascular risk scores used in this study.
- -
This is the first study to evaluate the relationship between the intake of different classes of polyphenols and cardiovascular risk measured by 4 different risk scores.
- -
The results obtained allowed comparison of these 4 equations with each other.
R. Estruch reports grants from Cerveza y Salud, Spain, and Fundación Dieta Mediterránea, Spain, as well as personal fees for lectures from Brewers of Europe, Belgium, Fundación Cerveza y Salud, Spain, Pernaud-Ricard, Mexico, Instituto Cervantes, Alburquerque, USA; Instituto Cervantes, Milan, Italy, Instituto Cervantes, Tokyo, Japan, Lilly Laboratories, Spain, and Wine and Culinary International Forum, Spain, nonfinancial support to organize a National Congress on Nutrition and feeding trials with products from Grand Fountain and Uriach Laboratories, Spain.
.
We thank all the volunteers for their participation and the medical professionals for their contribution to the PREDIMED-Plus trial. CIBEROBN, CIBERESP, and CIBERDEM are initiatives of the Instituto de Salud Carlos III (ISCIII), Madrid, Spain.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.06.013