Keywords
INTRODUCTION
One century after its description, Chagas disease remains one of the most prevalent infectious diseases in Latin America, and has become a health problem in the United States and Europe because of inmigration.1,2 The chronic dilated cardiomyopathy constitutes a severe clinical manifestation of the disease and one of the main causes of heart failure (HF).3
Dilated cardiomyopathy is a common and largely irreversible form of heart muscle disease, with an estimated prevalence of 1:2500; it is the third most common cause of heart failure and the most frequent cause of heart transplantation.4 The dilated cardiomyopathy phenotype with sporadic occurrence may derive from a particularly broad range of primary (and secondary) causes, including Chagas disease. Dilated forms of cardiomyopathy are characterized by ventricular chamber enlargement and systolic dysfunction. Although Chagas dilated cardiomyopathy has some peculiar characteristics, clinical manifestation is similar to idiopathic dilated cardiomyopathy.
The accurate assessment of prognosis in patients with cardiomyopathy is critical. Decisions regarding therapy are to be made on the basis of knowledge of the prognosis of affected patients.5 Previous studies addressing the influence of Chagas disease on mortality in patients with HF are limited by the heterogeneity of patient populations.6-11 In addition, several studies focused on univariate predictors of death, and included only left ventricular (LV) systolic function, and thus can not be considered definitive.12
Recently, we have demonstrated the prognostic value of right ventricular (RV) dysfunction13 and increased LV filling pressures14 in patients with Chagas cardiomyopathy. However, few data are available addressing the influence of the underlying cause of dilated cardiomyopathy on prognosis.15 The role of Chagas etiology as an independent predictor of mortality in patients with cardiomyopathy is unknown. For this reason, we hypothesized that Chagas disease as a cause of dilated cardiomyopathy would be a predictor an adverse outcomes.
To address this issue, we performed this study to identify mortality risk factors in a large series of patients with dilated cardiomyopathy and to analyze the prognostic impact of Chagas etiology on other echocardiographic parameters predictors of outcome in dilated cardiomyopathy.
METHODS
Selection of Patients
The study enrolled 291 consecutive patients with dilated cardiomyopathy who were referred to our institution from June 1999 until July 2008. Four patients were excluded; two patients were lost to follow up and the other two patients were excluded because of the association of systemic diseases which, by themselves, could reduce survival. A total of 287 patients fulfilled inclusion criteria and were included in the study. The study protocol was approved by the institutional ethics committee, and all enrolled patients gave informed written consent.
Inclusion criteria were the diagnosis of dilated cardiomyopathy, characterized by the echocardiographic finding of a dilated left ventricle with impaired ventricular systolic function. Patients were eligible if they had a left ventricular diastolic diameter/body surface area ≥31 mm and left ventricle ejection fraction <55%.
Patients were grouped into 2 categories according to the underlying cause of cardiomyopathy: a) Chagas dilated cardiomyopathy (CDC), characterized by the dilated cardiomyopathy secondary to Chagas disease, which required at least two positive serologic tests for antibodies against Trypanosoma cruzi; b) idiopathic dilated cardiomyopathy (IDC) defined by the presence of left ventricular dilatation and left ventricular systolic dysfunction in the absence of significant coronary artery disease or other specific heart muscle diseases.4,16 In all patients with IDC, Chagas disease was excluded by negative serologic testes.
Patients who had other associated heart diseases were excluded. At the time of enrollment, all patients underwent clinical examination and NYHA functional class was established. Standard laboratory tests, 12-lead ECG and a comprehensive Doppler echocardiogram with color flow mapping were performed in all patients. Brain natriuretic peptide (BNP) levels were also obtained.
Medical treatment for HF was optimized according to current practice guidelines17 at the time of enrollment and follow-up visits. Treatment with ACE inhibitors, beta-blockers, or both, was tailored according to clinical status up to the maximal tolerated dosage.
Heart transplantation was considered as a therapeutic option in patients who met standard criteria for this procedure. All heart transplantation procedures and hospital admissions resulting in urgent transplantation occurred at our institution.
Echocardiography
Images were acquired using a Sonos 5500 (Hewlett-Packard, Andover, MA, USA) equipment with 2.5 to 3.5 MHz transducers. All echocardiograms were performed by one investigator who was blinded to the clinical evaluation of the patients. The echocardiographic measurements were performed according to the recommendations of the American Society of Echocardiography. LV ejection fraction was calculated according to the modified Simpson's rule.18
Global RV function was quantitatively assessed using the RV myocardial performance index (Tei index).19 RV diastolic area was measured in the apical 4-chamber view. Pulmonary artery pressure was estimated by the tricuspid regurgitation velocity.
Diastolic function was assessed by pulsed-wave Doppler examination of mitral, pulmonary venous inflow and tissue Doppler imaging (TDI).20,21 TDI at the medial border of the mitral annulus was obtained from the apical 4-chamber view and systolic velocity (S), early (E'), late (A') and the ratio between peak mitral E and E' were calculated (E/E'). Left atrial volume was assessed by the biplane area-length method from the apical 4- and 2-chamber views.22
Analysis of Follow-up Data
Follow-up visits were conducted on an outpatient basis at least every 6 months, or more often, according to the patients' clinical status. Detailed information about symptoms, clinical history, use of medication, and therapeutic interventions were obtained at each follow-up visit.
Primary end points for follow-up were cardiac death or heart transplantation, or the end of the study. For the purpose of the analysis, patients who died or underwent cardiac transplantation were considered as a single group. Death was classified as sudden if it occurred within one hour after a change in symptoms, was unwitnessed in a patient whose condition had been stable, or occurred during sleep. It was due to progressive heart failure if it occurred after a documented period of symptomatic or hemodynamic deterioration. Cardiac death was defined as death caused by any cardiovascular disease and noncardiovascular death was due to any other cause.
Statistics Analysis
Categorical data were presented as numbers and percentages, and continuous data were expressed as means (SD) (standard deviation) or the median and interquartile range (25%-75%). The significance of baseline differences between patients with CDC and IDC was determined using the chi-square test or the unpaired t-test, as appropriate.
Further estimations of risk were performed using Cox proportional-hazards modeling. Potential independent predictors of outcome were identified initially by univariate analyses. All univariate predictors were then entered in a stepwise procedure into a survival multivariate model, with entry and remove set to a significance level of 0.05.
Variables with low prevalence or exhibiting multicollinearity did not enter into the multivariate model. Collinearity between E/E' ratio and left atrial volume was present, and the latter was included in the final multivariate models. Similarly, covariates considered as having potential prognostic impact were entered into the model.
Proportional hazards model and interaction assumptions were tested and no violation was observed. A significant improvement in model prediction was based on the likelihood ratio statistic, which follows a chi-square distribution, and the p-value was based on the incremental value compared with the previous model. Because multivariate analysis requires a complete set of variables for each patient, missing data from one or more variables restricted the final analysis to 239 patients (83%).
Cumulative survival curves for the occurrence of the study end points were performed by the Kaplan- Meier method and compared by the log-rank test. A value of P<.05 was considered significant. SPSS version 13 (SPSS Inc., Chicago, Illinois) was used for all analyses.
RESULTS
Baseline Patient Characteristics
A total of 287 consecutive patients with dilated cardiomyopathy were prospectively enrolled. Two hundred twenty-four patients (78%) had CDC, and 63 (22%) had IDC. The mean age was 48.6 (12.9) years, and 39 % were women. Most patients (75%) were in NYHA functional class I and II at the time of enrollment into the study. Thirty patients had a pacemaker at inclusion.
The baseline clinical characteristics of patients, according to the presence or absence of Chagas etiology are presented in Tables 1 and 2. There was substantial homogeneity between the groups with regard to age, gender, and functional class. History of a previous stroke was more frequent in CDC group.
Right bundle-branch block was the most frequent ECG abnormality in the CDC group, but it was not associated with outcome. Likewise, left bundle-branch block was more frequent in the IDC group (Table 1). The proportion of patients with pacemakers and premature ventricular contractions was higher in Chagas patients. No difference regarding other ECG variables was observed.
Compared to patients with Chagas disease, BNP levels were significantly higher in non-chagasic patients (Table 1). LVEF was significantly higher in the CDC group compared with the IDC group (36.2% vs 28.5%; P<.001) (Table 2). Echocardiographic parameters to assess RV function were similar between the two groups, although pulmonary artery systolic pressure was significantly lower in the CDC group. Indexes of elevated LV filling pressures did not show statistical difference between patients with CDC and IDC. LV apical aneurysm was found only in Chagas patients.
Follow-up
During a mean follow-up of 39.5 months (median, 32.6; range, 7 days to 9.1 years), 104 patients died and 9 patients underwent cardiac transplantation. Survivors were followed for a mean of 47.9 (33.3) months. Mean survival in patients who had an adverse outcome was 27.2 (25.8) months (P<.001). Seventeen patients (6%) did not complete total follow-up and were censored at the time of their last visit. Median follow-up time was 31.5 months in those lost to follow up; the interquartile range (25%-75%) was 6.7-51.6 months.
At the end of follow-up, 233 patients (81%) were on angiotensin-converting enzyme inhibitors, 194 (68%) on diuretics, 113 (39%) on amiodarone, 105 (37%) on digoxin, 67 (23%) on anticoagulants, and 71 (25%) on beta-blocking agents. Medication use at the end of follow up was similar between groups, with the exception of beta blocking agents and digitalis, which were more frequently used in the IDC, whereas amiodarone was prescribed in nearly half of CDC patients.
Fifty deaths (48%) were due to progressive heart failure, 44 (42%) were sudden, 6 (6%) were due to stroke, and 4 (4%) were due to noncardiovascular causes. Nine patients received a pacemaker and 5 patients received a cardioverter-defibrillator. Three patients underwent cardiac resynchronization therapy. Patients who received a cardioverterdefibrillator or cardiac resynchronization therapy were censored at the time of implantation.
Predictors of Outcome
The overall mortality rate in our study population was 11.96% per year. A number of baseline characteristics were univariate predictors of outcome in the study cohort (Table 3). Neither age nor sex influenced the probability of survival.
When evaluated in a univariate model, CDC was associated with a worse outcome. Similar analysis was also performed after stratifying patients on the basis of their LVEF, and the survival rate remained dependent on the etiology of dilated cardiomyopathy. When compared with ICD patients, survival was significantly worse in patients with dilated cardiomyopathy due to Chagas disease (hazard ratio=3.53; 95% confidence interval, 1.77 to 7.025; P<.001).
Although the number of cardiac events at the end of the study was similar between chagasic (n=91, 41%) and non-chagasic (n=22, 35%), there was significant difference in the time to death. The 1-year mortality was 25% and 11% for patients with CDC and IDC, respectively (P=.024). To adjust for differences between groups, we performed multiple Cox proportional-hazards analyses. In a multivariate analysis in which all univariate (P<.05) predictors of outcome were considered, Chagas disease as the primary cause of dilated cardiomyopathy remained a strong predictor of prognosis (hazard ratio=2.48; 95% confidence interval, 1.28-4.78; P=.007), independent of clinical data and standard Doppler echocardiographic predictors of outcome.
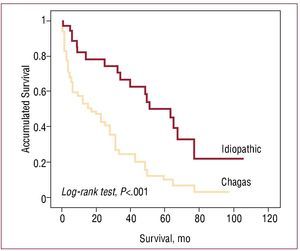
In a subgroup with severe LV systolic dysfunction (LVEF≤30%), the survival rate in patients with cardiomyopathy due to Chagas disease was 55% and 26% at 1 and 3 years, compared with 82% and 67% at 1 and 3 years in those with IDC (hazard ratio=3.01; 95% confidence interval, 1.35-6.73; P=.007 and hazard ratio=3.47; 95% confidence interval, 1.76 - 6.82; P<.001, respectively) (Figure 1).
Figure 1. Survival of patients with dilated cardiomyopathy and severe left ventricular systolic dysfunction (ejection fraction ≤30%) stratified according to etiology of the cardiomyopathy.
The other independent predictors of outcome were NYHA functional class, LVEF, RV Tei index and LA volume indexed to body surface area (Table 4). Although beta-blocker use was not a significant univariate predictor of outcome, we included it in the multivariable model due to its clinical importance, but it was not a predictor of prognosis.
DISCUSSION
The present study evaluated the long-term prognostic value of Chagas disease as the primary etiology of cardiomyopathy. CDC was found to be a significant predictor of poor survival when compared with IDC, after adjusting for well-established parameters predictors of outcome. To the best of our knowledge, this is the first study which included several echocardiographic parameters in prognostic models in patients with dilated cardiomyopathy.
Chagas Compared With Idiopathic Dilated Cardiomyopathy
Our finding of worse survival CDC is consistent with previous studies.6-8,10 However, these studies compared the prognosis of CDC with the prognosis of HF secondary to several etiologies (including ischemic) and at distinct stages of disease progression, showing different survival rates. In addition, some studies were performed before modern therapy for HF was available.6,23-25 In our study, Chagas was compared to a homogenous population in terms of the etiology of the dilated cardiomyopathy (only idiopathic dilated cardiomyopathy was included). Additionally, our study included important new echocardiographic prognostic variables, such as left ventricular filling pressures and RV function parameters, which have not been included in previous studies.26 The addition of Chagas disease as the underlying cause of the dilated cardiomyopathy significantly improved the prognostic utility of a model containing clinical variable and conventional echocardiographic indexes of LV systolic and diastolic function, as well as RV systolic function. While Chagas patients are often excluded from randomized trials analyzing therapy for HF, our study confirmed in Chagas disease, the value of several new prognostic parameters described as predictors of all cause-mortality in dilated cardiomyopathy.13-14,23-25,27-30
The main differential diagnosis of CDC is idiopathic cardiomyopathy.4 The worse prognosis of CDC may be related to a more extensive amount of myocardial destruction in this disease than in IDC, although this is somewhat controversial.11 Perhaps the persistence of the activity of myocarditis, whether due to the direct participation of the parasite or due to immunological mechanisms, in addition to the diffused distribution of histological lesions may somehow contribute to the more adverse outcome of CDC.11,31 Indeed, myocardial fibrosis has been shown to correlate inversely with LVEF and clinical status.32 The prognostic value of Chagas etiology may also be attributed to the severity of ventricular arrhythmias,33 to the autonomic nervous system burden present and to myocardial perfusion abnormalities.31,34,35 Besides, neurohormonal activation per se can lead to a vicious cycle of progressive remodeling in chronic Chagas heart disease.36
Prognostic Value of Echocardiographic Parameters in Dilated Cardiomyopathy
Echocardiography is the single most useful diagnostic test in patients with HF, providing measurements of ventricular function and evaluating prognosis4,17 LVEF, the conventionally used prognostic variable, is related to a variable clinical course and other parameters, such as LV filling pressures, left atrial volume, and RV function, improve the accuracy of prognostic stratification.37-39
However, studies assessing the long-term prognostic value of these echocardiographic parameters in patients with Chagas disease are scarce. In our study the degree of diastolic dysfunction predicted survival in patients with both CDC and IDC, similar to what has been described in other etiologies of HF.14,37,40-42 Although E/E' has proven to be superior to BNP levels in diagnosing volume overload,41 these parameters did not remain in the final model. Left atrial volume is associated with BNP levels in Chagas disease,43 and had strong impact on adverse cardiac events.
RV function has been clearly shown to relate to prognosis in patients with HF of both ischemic and nonischemic etiology.13,44,45 The present study confirms the prognostic value of RV dysfunction in patients with CDC and IDC. RV involvement is considered a typical feature of Chagas cardiomyopathy,46-48 and previous studies have suggested that the worse prognosis of Chagas heart disease could be related to RV dysfunction in this disease.6-7,10 The current study does not completely support this explanation, because echocardiographic parameters used to assess RV function were similar between the two groups. However, CDC patients had lower pulmonary artery systolic pressure than patients with IDC. Our patients with RV dysfunction presented with more extensive biventricular involvement, and this may be due to the primary pathologic process.
Study Limitations
The applicability of our results to the general population of patients with HF is limited by the referral nature of this cohort. Overall, treatment of patients with HF in South America is not uniform.3
Patients who received a cardioverter-defibrillator or cardiac resynchronization therapy were censored at the time of implantation. As a consequence, it could have introduced a systematic bias confounding the prognosis of patients. However, these important confounders were partly addressed by including all patients in the analysis regardless of devices use. Even thus, there was no difference in mortality.
Although the Cox proportional hazards model showed a strong association between Chagas cardiomyopathy and mortality, no definitive cause-effect relationship between these variables can be established, since in cohort studies confounding cannot be ruled out for all (residual confounding, unmeasured or unknown important variables).
Clinical Implications
Chagas disease is an important health problem in some areas of the world. The fact that Chagas disease is usually thought of as an exotic disease restricted to South America, decreases clinicians' awareness of the disease and likely that many Chagas patients are actually being misdiagnosed as having idiopathic dilated cardiomyopathy.49
The identification of the underlying cause of the dilated cardiomyopathy is critical, because HF secondary to Chagas cardiomyopathy has worse survival than IDC. Therefore, due to the limited number of hearts available for transplantation, it may be that Chagas patients in the high-risk group should be considered as having priority to receive cardiac transplantation.
CONCLUSIONS
The present study demonstrates that Chagas etiology was associated with worse survival when compare with idiopathic dilated cardiomyopathy, independent of other markers of poor prognosis in HF, such as NYHA functional class, LVEF, RV function and left atrial volume. The identification of the underlying cause of the dilated cardiomyopathy has prognostic importance, primarily for patients with Chagas cardiomyopathy. Furthermore, echocardiographic assessment provides important prognostic information in patients with dilated cardiomyopathy and should be used in clinical practice.
ABBREVIATIONS
CDC: Chagas dilated cardiomyopathy
HF: heart failure
IDC: idiopathic dilated cardiomyopathy
LV: left ventricle/ventricular
LVEF: left ventricular ejection fraction
RV: right ventricle/ventricular
Correspondence: Dra. M.C.P. Nunes.
Departamento de Clínica Médica. UFMG.
Av. Professor Alfredo Balena, 190. Santa Efigênia. 30130 100 - Belo Horizonte, MG. Brazil.
E-mail: mcarmo@waymail.com.br
Received July 29, 2009.
Accepted for publication January 25, 2010.