When the bicuspid aortic valve is associated with dilatation of the aorta, surgical repair requires correction of all the components of the aortic root. Here, we review our experience in this type of surgery.
MethodsA descriptive and retrospective observational study was carried out to analyze morbidity and mortality in valve-sparing techniques and evaluate the medium-term durability of the aortic valve. We included all patients with a bicuspid aortic valve and dilatation of the aorta who underwent surgery with a valve-sparing technique in our center between 1999 and 2011.
ResultsA total of 151 patients underwent surgery. A valve-sparing technique was used in 51 patients. The mean (standard deviation) age of the patients was 51 (12) years and 92% were men. In 69% of the patients, aortic insufficiency was less than grade II and the aortic cusps showed little structural degeneration. Valve reimplantation was performed in 32 patients. There was no hospital mortality. With a median follow-up of 36 months (interquartile range, 18-45 months), none of the patients died or required reoperation, and all patients were free of aortic insufficiency greater than grade II.
ConclusionsValve-preserving surgery in bicuspid aortic valves associated with dilatation of the aorta shows excellent short- and medium-term results in selected valves. The stabilization of all of the components of the aortic root improves the durability of the valve, and the techniques proposed are reproducible and stable in the medium-term.
Keywords
Bicuspid aortic valve (BAV), found in 1% to 2% of the population, is the most common congenital cardiac malformation.1 Although a recent study demonstrated that the incidence of acute aortic syndrome in persons with BAV is low and that their survival is similar to that of the general population, most studies describe a greater predisposition to aortic valve (AoV) disease and aneurysms of the ascending aorta (AA).2–4 These types of disorders usually present early in life (eg, in the Olmsted County series,3 BAV surgical intervention was required at a mean age of 40 (20) years compared with 67 (16) years in patients with tricuspid AoV), which means that patients with BAV have a high probability of requiring surgery of the AoV or of the thoracic aorta during the natural history of the disease.5
In recent years, AoV-sparing surgical techniques have been developed to avoid complications with prostheses and chronic anticoagulation.6,7 Although these techniques were initially reserved for patients with tricuspid AoV, various groups have since used them for BAVs. For example, both Aicher et al.8 and El Khoury et al.9 analyzed the medium-term results of 205 and 68 patients, respectively, that underwent reconstructive surgery of the BAV, and found no significant differences in the stability of the repair compared with that of tricuspid AoV patients.
However, other authors doubt the durability of these types of procedures in a valve with a high susceptibility to calcification, and the procedure of choice remains controversial.5,10
In our study, we analyzed the results of reconstructive surgery and the durability of valve-sparing techniques in patients with BAV and aortic aneurysms.
METHODSA descriptive and retrospective observational study was performed to analyze the in-hospital morbidity and mortality of AoV-sparing techniques for BAV associated with aneurysm of the aortic root and/or the AA. In addition, the medium-term durability of the repaired AoV was analyzed. The aim of this study was not to compare these patients with those with dilatation of the Valsalva sinus (VS) or of the AA, nor with the series of patients not undergoing BAV-sparing surgery. Therefore, we only present data that could be valuable in understanding patient selection.
In agreement with the recommendations current during the study period,11 patients with a dilatation of the aorta greater than 50mm were considered candidates for surgery.
During this period, another 225 patients with BAV who required valve replacement underwent surgery; 125 had isolated valve disease, while 100 also showed dilatation of the aortic root or AA. The decision to preserve the AoV was taken by the surgeon after careful inspection of the aortic root (ie, ring, VS, sinotubular junction, commissures, and cusps). Patients with valves with calcification in both cusps or with retraction, tissue loss, or perforations were not considered candidates for surgical repair. However, preservation was not conditional on cusp prolapse, ring diameter, or the preoperative aortic insufficiency (AI) grade.
In all patients, intraoperative transesophageal echocardiography was performed to evaluate the anatomy and function of the AoV after repair.
This study was approved by the Ethics Committee of the Hospital Universitario 12 de Octubre, Madrid, and all patients provided informed consent for review of their clinical data.
Surgical TechniqueIn patients in group A (n=32; with aneurysm of the VS), valve reimplantation was carried out according to the method of David, as reported previously.12 To reconstruct the VS, a Hemashield Platinum Dacron graft (Boston Scientific Ibérica; Barcelona, Spain) was used. In patients in group B (n=19; with aneurysm of the AA), resection of the AA aneurysm and remodeling of the sinotubular junction was performed via a supracoronary tubular Hemashield Dacron prosthesis (Boston Scientific Ibérica).
Follow-upA total of 98% of the patients were successfully followed up. One patient from outside Madrid with serious social problems was lost to follow-up. The clinical follow-up was by consultation at 2 months after surgery and annually thereafter. A transthoracic echocardiogram was carried out before discharge, and again at 2 months and 1 year (in all patients the last follow-up visit took place between January and September 2012). The AI was graded semiquantitatively as mild, moderate, or severe. Follow-up was via telephone for those patients located outside Madrid, who forwarded the corresponding echocardiography reports.
Statistical AnalysisTo test the normality of the population, the Kolmogorov-Smirnov test was used. Continuous variables are presented as mean (standard error) of the mean. Categorical variables, such as absolute and relative frequencies, are reported as percentages. Total survival and survival free of AI greater than grade II was analyzed with the Kaplan-Meier method. The statistical software package SPSS 15.0 (SPSS Inc.; Chicago, Illinois, United States) was used for all statistical analyses.
RESULTSBetween March 1999 and September 2012, 51 patients with BAV and dilatation of the aortic root or AA underwent an AoV-sparing technique; 32 patients had an aneurysm of the VS (group A) and 19 had an aneurysm of the AA (group B).
In 39 patients, the surgical indication was aneurysmal dilatation of the VS and/or AA. In 9 patients, the indication was for AI grade III-IV associated with dilatation of the left ventricle, and 3 patients underwent emergency surgery upon diagnosis of Stanford type A acute aortic dissection.
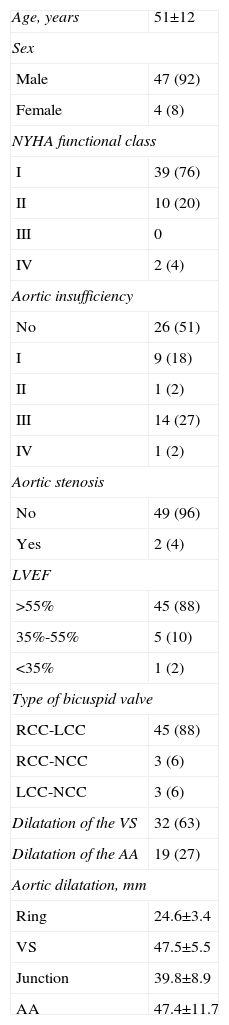
Patient CharacteristicsThe demographic and preoperative characteristics of the 51 patients with BAV who underwent AoV-sparing surgery are shown in Table 1. The majority (92%) were male, with a normally functioning AoV or preoperative AI less than grade III (71%) and with a predominance of type I BAV (fusion of the right and left coronary cusps). Fusion of the raphe and mild calcification of 1 of the cusps or the raphe was seen in 40 patients (78%) and 9 patients (18%), respectively. In all patients, a segment of the aorta was dilated at the time of the intervention. Aneurysms of the VS (group A) and the AA (group B) were also found in 32 and 19 patients, respectively. The logistic EuroSCORE was 3.92% (1.23%) for the entire series.
Preoperative Characteristics of Patients With Bicuspid Aortic Valve
| Age, years | 51±12 |
| Sex | |
| Male | 47 (92) |
| Female | 4 (8) |
| NYHA functional class | |
| I | 39 (76) |
| II | 10 (20) |
| III | 0 |
| IV | 2 (4) |
| Aortic insufficiency | |
| No | 26 (51) |
| I | 9 (18) |
| II | 1 (2) |
| III | 14 (27) |
| IV | 1 (2) |
| Aortic stenosis | |
| No | 49 (96) |
| Yes | 2 (4) |
| LVEF | |
| >55% | 45 (88) |
| 35%-55% | 5 (10) |
| <35% | 1 (2) |
| Type of bicuspid valve | |
| RCC-LCC | 45 (88) |
| RCC-NCC | 3 (6) |
| LCC-NCC | 3 (6) |
| Dilatation of the VS | 32 (63) |
| Dilatation of the AA | 19 (27) |
| Aortic dilatation, mm | |
| Ring | 24.6±3.4 |
| VS | 47.5±5.5 |
| Junction | 39.8±8.9 |
| AA | 47.4±11.7 |
AA, ascending aorta; LCC, left coronary cusp; LVEF, left ventricular ejection fraction; NCC, noncoronary cusp; NYHA, New York Heart Association; RCC, right coronary cusp; VS, Valsalva sinus.
Data are expressed as no. (%) or mean±standard deviation.
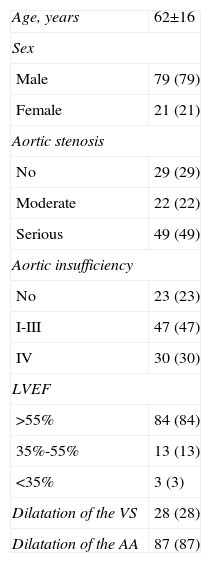
The demographic data of the 100 patients with BAV and aneurysm of the aorta who underwent valve replacement are shown in Table 2. In the majority of patients (71%), the AoV was stenotic. Of the 29 patients with a normal AoV or AI, 17 underwent surgery before 2005, when the surgical repair of the AoV had still not been established in our department, and the BAV was replaced. Of the 12 patients who underwent surgery after 2005, 8 had calcifications in both cusps and 4 had cusps that appeared retracted and with highly calcified commissures. The logistic EuroSCORE was 4.12% (1.33%).
Demographic Characteristics of Patients With Bicuspid Aortic Valve Not Undergoing Valve-sparing Surgery
| Age, years | 62±16 |
| Sex | |
| Male | 79 (79) |
| Female | 21 (21) |
| Aortic stenosis | |
| No | 29 (29) |
| Moderate | 22 (22) |
| Serious | 49 (49) |
| Aortic insufficiency | |
| No | 23 (23) |
| I-III | 47 (47) |
| IV | 30 (30) |
| LVEF | |
| >55% | 84 (84) |
| 35%-55% | 13 (13) |
| <35% | 3 (3) |
| Dilatation of the VS | 28 (28) |
| Dilatation of the AA | 87 (87) |
AA, ascending aorta; LVEF, left ventricular ejection fraction; VS, Valsalva sinus.
Data are expressed as no. (%) or mean±standard deviation.
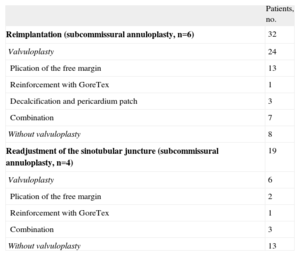
The surgical techniques used are shown in Table 3. For reconstruction of the VS, 34-mm and 32-mm Hemashield Platinum Dacron grafts were used in 17 and 15 patients, respectively. In 24 patients (75%), a procedure on the aortic cusps was required (due to cusp prolapse in 17 patients and calcification in 7); in all of these patients, this intervention was performed after completing reimplantation of the AoV. The most common technique used (n=13) was a plication of the free margin of the cusp at the level of the nodules of Arantius via a 6-0 Prolene suture (Ethicon; San Lorenzo, Puerto Rico). In 3 patients with a calcified raphe, decalcification of the raphe was required for its subsequent reconstruction via an autologous pericardium patch. In 1 patient with prolapse of the anterior cusp, the free margin was strengthened with a 7-0 GoreTex suture (W.L. Gore and Associates; Flagstaff, Arizona, United States). A combination of these techniques was performed in 7 patients. A Cabrol subcommissural annuloplasty was performed in 7 patients with an aortic ring of greater than 24mm after valve reimplantation.13
Surgical Techniques Used
| Patients, no. | |
| Reimplantation (subcommissural annuloplasty, n=6) | 32 |
| Valvuloplasty | 24 |
| Plication of the free margin | 13 |
| Reinforcement with GoreTex | 1 |
| Decalcification and pericardium patch | 3 |
| Combination | 7 |
| Without valvuloplasty | 8 |
| Readjustment of the sinotubular juncture (subcommissural annuloplasty, n=4) | 19 |
| Valvuloplasty | 6 |
| Plication of the free margin | 2 |
| Reinforcement with GoreTex | 1 |
| Combination | 3 |
| Without valvuloplasty | 13 |
Patients in group B (n=19) underwent resection of the aneurysm of the AA and remodeling of the sinotubular junction via a supracoronary tubular Hemashield Dacron prosthesis (mean diameter, 28 [3] mm). Six patients (32%) required surgery of the aortic cusps. Four patients with a dilated aortic ring underwent a subcommissural annuloplasty.13
Other associated procedures were surgery of the aortic arch in 5 patients, repair of the mitral valve in 3, resection of the subaortic membrane in 1, and myocardial revascularization in 1.
In-hospital OutcomeThe mean durations of extracorporeal circulation and aortic clamping were 127 (18) min and 109 (18) min in group A, respectively, and 74 (22) min and 57 (24) min in group B, respectively. Intraoperative transesophageal echocardiography was performed after the bypass, which showed a normally functioning AoV (AI grade, 0-1) in all patients except 2 patients in group A with AI greater than grade II due to cusp prolapse. In both patients, the prolapse was corrected through a central plication. The results of a subsequent echocardiographic evaluation were normal. There was no hospital mortality. One patient in group A required reintervention due to excessive bleeding during the first few hours after surgery. One patient in group B with a history of ischemic stroke had a new cerebrovascular event, which resulted in permanent dysarthria. There were no other major complications.
Follow-upDuring a median follow-up of 36 months (interquartile range, 18-45 months), no patient died or required reintervention on the AoV. One patient in group B showed signs of degeneration of the aortic cusps, with a mean transvalvular gradient of 40mmHg. All patients were free of AI greater than grade II (AI grade II, 7 patients; AI grade I, 14 patients; and AI grade 0, 30 patients), and 84% were free of anticoagulant therapy.
DISCUSSIONAlthough valve replacement is the surgical procedure most often used to treat AoV disease, the implantation of an aortic prosthesis leads to considerable medium- and long-term morbidity. Hammermeister et al.14 note that 15 years after the implantation of an aortic prosthesis (biological or mechanical), approximately 60% of the patients had serious prosthesis-related complications. According to other authors,15–17 the annual incidence of thrombotic and/or hemorrhagic complications due to chronic anticoagulation is between 2% and 7%. Other series, however, report better results in the long-term follow-up of aortic prostheses, with a lower incidence of thromboembolism or hemorrhage secondary to anticoagulant therapy.18,19 However, in young patients, the chronic need for medication significantly impairs their quality of life, which, in women, is compounded by the potential difficulties of any pregnancy. Therefore, repair and preservation of the AoV avoids these complications and improves patients’ quality of life, particularly that of young patients.
The surgical repair of the BAV has undergone considerable development in recent years, largely due to a better understanding of the aortic root as a functional unit and the standardization of surgical techniques that act on all its components (ie, aortic ring, valve cusps, VS, and sinotubular junction). Nonetheless, controversy exists about whether the AoV should be repaired because, according to some authors,2,3,20 it has a greater predisposition to calcification and stenosis. Inevitably, valve repair depends on the underlying valvular health, and the type of valves that can be expected to show appropriate durability are those without stenosis or those that have AI without marked calcification. In these valves, the progression of degeneration may be different. In fact, in the series with the longest known follow-up, Michelena et al.2 observed that, although 47% of patients had some degree of underlying AI, only 3% required surgical intervention on the AoV.
The objective of our study was to analyze the early results and evaluate the medium-term durability of repair in 51 patients who underwent reconstructive surgery of the BAV. This study is the most significant Spanish series published and has one of the largest number of participants. There was no hospital mortality, and perioperative morbidity was low, with one case of stroke in a patient with a history of embolic strokes. With a median follow-up of 36 months, there were no deaths and all patients were free of AI greater than grade II and reintervention on the AoV. The results obtained indicate that, when an appropriate and accurate surgical technique is used, most patients can benefit from repair, even when the AoV is bicuspid. In addition to stabilizing the components of the aortic root, surgery of the aortic cusps with prolapses or isolated calcifications is required to achieve correct valve function. In 75% of the patients in group A, some type of procedure had to be performed on the cusps, the most frequent being central plication.
El Khoury et al.9 reported their results in 68 patients with BAV and associated AI. With a mean follow-up of 34 months, 58 patients (85%) had AI less than grade II, although 6 (8.8%) required reintervention due to AoV dysfunction. Aicher et al.8 published the series with the largest number of patients (205 patients surgically treated for BAV), in which, after a 10-year follow-up, 19% of the patients required reintervention due to AoV dysfunction. The difference between the results of these series and the present series could be due to diverse factors: a shorter follow-up, a smaller number of patients with AI grades III-IV (29% in our series), and the fact that AoV without substantial cusp degeneration were repaired in the present study (although the raphe was fused in 25 patients, only 7 had calcification of the cusps or the raphe). We believe that the factors with the greatest impact on the durability of repair are calcification and/or fibrosis of the valve cusps. Thus, in the series of El Khoury et al.,9 triangular resection of the cusps was necessary in 26 of the 38 patients (68%) with BAV and associated dilatation of the VS or AA. The high incidence of resections indicates the presence of considerable fibrous tissue in the cusps, which probably affected the durability of the repair. This thickening of the cusps excludes the use of a central plication, which, in our opinion and that of other authors,8 is the easiest and most reproducible technique. Furthermore, because central plication is performed in the region of the cusp submitted to the least stress, the durability of the repair is enhanced.
The association of dilatation of the VS or AA with BAV is frequent and well documented.2,3 In our study, dilatation of a segment of the aorta was seen in all patients. We performed an AoV reimplantation in 32 patients that showed dilatation of the VS, and all achieved a normally functioning AoV. De Kerchove et al.21 reported similar results. These authors analyzed 161 patients with BAV repair, and compared the valve reimplantation group (n=74) with the group without BAV repair (n=87). After a 6-year follow-up, they found that the absence of reoperation and an AI greater than grade II were significantly greater in the valve reimplantation group (100% vs 90% [P=.03], and 100% vs 77% [P=.002], respectively). Other authors8 have also published good results with remodeling of the aortic root, although when this technique is used, the aortic ring must be stabilized separately. Lansac et al.22 suggest performing an annuloplasty with a rigid external ring. Kazui et al.23 propose a subvalvular circular annuloplasty through a polytetrafluoroethylene ring, and Svensson et al.24 advocate a subannular polytetrafluoroethylene suture. In our experience, reimplantation is a simple and reproducible technique. Moreover, its advantage is that it simultaneously stabilizes all of the components of the aortic root and also acts on the ring.
A subcommissural annuloplasty was performed in 11 patients (7 in group A for an aortic ring greater than 24mm after reimplantation and 4 in group B for an associated annular dilatation). We believe that this technique reduces the diameter of the aortic ring and improves the coaptation surface of the aortic cusps. Although some authors8 associate this technique with a decrease in the durability of the repair, we found no such association in our series and, at the time of writing, the 11 patients remain free of AI greater than grade II.
LimitationsThis study reports a nonconsecutive series of patients chosen according to the surgeon's criteria. Although the initial and medium-term results are good, longer patient follow-up is required to evaluate the long-term behavior of the preserved BAV. Due to the considerable number of remotely located patients, postoperative follow-up echocardiography was decentralized and performed by multiple observers.
CONCLUSIONSValve-sparing surgery in BAV associated with dilatation of the VS and/or AA shows excellent short- and medium-term results in selected valves. The stabilization of all of the components of the aortic root improves the durability of the valve, and the techniques proposed are reproducible and stable in the medium-term.
CONFLICTS OF INTERESTNone declared.