Atrial fibrillation is associated with substantial morbidity and mortality and both its incidence and prevalence are high. Nevertheless, comprehensive data on this condition in Spain are lacking. The aim of this study was to estimate the prevalence of atrial fibrillation in Spain.
MethodsA cross-sectional study was conducted in the general Spanish population older than 40 years. Two-stage random sampling was used, in which first-stage units were primary care physicians randomly selected in every Spanish province and second-stage units were 20 randomly selected persons drawn from each participating physician's assigned population. The reported prevalence was standardized for the age and sex distribution of the Spanish population. The electrocardiogram recordings were read centrally.
ResultsOverall, 8343 individuals were evaluated. The mean age was 59.2 years (95% confidence interval, 58.6-59.8 years), and 52.4% of the participants were female. The overall age-adjusted prevalence of atrial fibrillation was 4.4% (95% confidence interval, 3.8-5.1). Prevalence was similar in both sexes, men 4.4% (3.6-5.2) and women 4.5% (3.6-5.3), rising with increasing age older than 60 years. In patients older than 80 years, the prevalence was 17.7% (14.1-21.3). In 10% of patients an unknown atrial fibrillation was diagnosed.
ConclusionsThe prevalence of atrial fibrillation in the general Spanish population older than 40 years is high, at 4.4%. The prevalence is similar in both sexes and rises steeply above 60 years of age. It is estimated that there are over 1 million patients with atrial fibrillation in the Spanish population, of whom over 90 000 are undiagnosed.
Keywords
Atrial fibrillation (AF) is the most common arrhythmia in Western countries and is associated with high mortality and morbidity.1,2 It is the leading cause of embolic events and is also associated with episodes of heart failure, cognitive impairment, and decreased quality of life.3–6 The most common embolic event is stroke, which is associated with severe disability and dependence, involving significant increases in costs and in the use of health care systems.7 Identifying these patients is important because anticoagulation therapy is effective in preventing embolic events in patients at high risk. Study of the population prevalence of AF, using homogeneous criteria, provides valuable information for planning appropriate strategies for the prevention and treatment of this disease. In Spain, there is a lack of epidemiological data that would allow the prevalence rates of AF to be determined in the general population. In general, previous studies were conducted in groups of patients or in selected populations that were not representative of the Spanish general population, such as patients from specific areas not representative of the whole country, patients attending health centers or cardiology clinics, which introduced bias, or patients within narrow age ranges.8–11
The aim of this population-based study was to estimate the prevalence of AF in the Spanish population older than 40 years by age (decades) and sex groups.
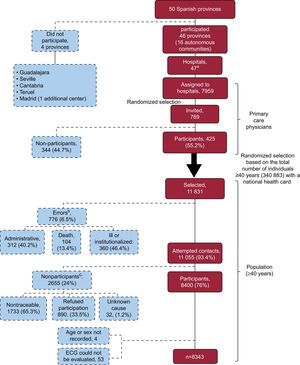
METHODSDesign and DefinitionsA cross-sectional study was conducted in primary care (PC) among the general Spanish population older than 40 years assigned to a PC physician. One hospital from each Spanish province (2 in the case of Barcelona and Madrid) was invited to participate in the study, as well as a referral cardiologist from each hospital. In total, 46 provinces and 47 hospitals and cardiologists participated. Four provinces and the second hospital in Madrid were excluded or did not participate due to a variety of logistic problems. Based on this, a 2-stage random sampling procedure was used.
In each hospital, the number of PC physicians and their assigned population was determined and the participating physicians were selected using simple random sampling. Ten PC physicians were selected from each hospital. Each cardiologist was responsible for coordinating the work of these 10 physicians in his or her center. At this time, the participating hospitals had almost 8000 PC physicians assigned to them. A further 769 physicians were invited to participate, of whom 425 (55.2%) participated (Fig. 1).
Flowchart of participation in the OFRECE study. ECG, electrocardiogram.
aBarcelona: 2 hospitals participated. bErrors. Administrative: no longer a patient of the physician (does not belong to the center or the quota assigned), language difficulty; ill or institutionalized: institutionalized, acute or chronic disease preventing visits to the center, hospitalization, terminal process, bedridden, dementia, Alzheimer disease, mental disability, mental retardation or cognitive impairment. cReasons for not participating. Unreachable: after repeated attempts to contact by mail and/or telephone; participant refusal: refusal to participate or initial acceptance but failure to attend the center, various personal or business reasons preventing attendance at the center; unknown: unspecified cause.
For each participating PC physician, simple random sampling based on the national health card of the assigned population older than 40 years was performed, so that 20 patients were selected per physician. Selected individuals were invited to participate by the PC physician. At this stage, a 76% (n=8400) participation rate was achieved. All participants gave their informed consent to participate in the study. The study began in March 2010 and ended in October 2012.
Overall, 57 people were excluded due to the lack of key information (n=4) or because the electrocardiogram (ECG) could not be evaluated (n=53), and thus the final sample consisted of 8343 participants (Fig. 1).
All patients were examined by their PC physician, an ECG was performed on the day of the visit, and the patients were referred to the coordinating cardiologist for fast tracking according to the protocol (newly diagnosed or uncertain diagnosis). All ECGs were read centrally by at least 2 cardiologists (Fuenlabrada University Hospital) as described below. All the ECGs were initially evaluated by 1 cardiologist and subsequently by another cardiologist. If there was a discrepancy between the 2 diagnoses, a third cardiologist was consulted and a final diagnosis was reached by consensus between the second and third cardiologists. Of the total number of ECGs analyzed, a consensus was reached in 99.9% of the patients, of which 98.1% were classified as having AF (262 of 267) by 1 observer; thus, in 1.9% of the patients, there was disagreement between the 2 cardiologists who specifically analyzed the ECGs for the presence of AF. In total, the 15 patients who were not diagnosed during their examination by the PC physician were diagnosed when their ECGs were read centrally. These diagnoses were reported to the PC physicians in order for them to take any appropriate action.
Information on demographic variables, personal details, and general variables were collected, as well as clinical variables using a specific questionnaire for AF. The various clinical variables were defined according to the guidelines of the American College of Cardiology/American Heart Association for AF12 as follows: obesity, body mass index greater than or equal to 30; overweight, body mass index greater than or equal to 25; central obesity, waist circumference greater than or equal to 102 cm for men and greater than or equal to 88cm for women; hypercholesterolemia, previous diagnosis and treatment with lipid-lowering drugs; diabetes mellitus, previous diagnosis and treatment with oral diabetic agents or insulin; and previous diagnosis of documented ischemic heart disease, such as previous myocardial infarction, unstable angina or revascularization. Hypertension was defined as the presence of any of the following criteria: a) previous diagnosis of hypertension and treatment with medication, diet or exercise, and b) systolic blood pressure greater than or equal to 140 mmHg or diastolic blood pressure greater than or equal to 90 mmHg on at least 2 occasions on the day of examination.
A diagnosis of AF was based on 2 criteria: a) the presence of AF on ECG performed on the day of examination, and/or b) a documented clinical history of nonpermanent AF (paroxysmal or persistent).
Statistical AnalysisGiven the nature of the sampling process, in which individuals in the population had different probabilities of being selected, each participant in the final sample was assigned a weight representing the number of people in the Spanish population (with the exception of Ceuta, Melilla, and Cantabria, which did not provide participants), for the same age, sex, and geographical area as those represented by the patient.13 Thus, the sum of all the weights of the sample was equal to the size of the Spanish population older than 40 years.
Weighting was done in 2 stages. In the first stage of the 2-stage sampling design, the weights were calculated as the inverse of the probability of selecting each individual in each stage of the sampling process. In the first stage (physician selection), the probability of selection in each province was calculated by using the number of PC physicians in the province as the denominator. In the second stage (participant selection), the number of people older than 40 years assigned to each physician was used as the denominator. In the second stage, a reweighting procedure was performed to adjust the sample distribution to the population distribution for variables related to the outcome of the analysis and not considered in the sampling procedure (age and sex). A third variable (geographical area) was included in case it was decided to present the data disaggregated by area. The data by autonomous community was not presented because the sample size calculated would provide inaccurate estimates. The reweighting procedure was performed using the method proposed by Deville and Särndal14 using the calibrate instruction in the Stata v10.1 statistical software package. The municipal population census of 2011 was used to adjust or calibrate for sex, age, and geographic area. We considered 5 geographic areas defined by autonomous community grouping: north (Aragón, Principality of Asturias, Galicia, Chartered Community of Navarre, Basque Country, La Rioja); central (Castile and León, Castile-La Mancha, Community of Madrid); east (Catalonia, Valencian Community, Region of Murcia, Balearic Islands); south/south-West (Andalusia, Extremadura); and the Canary Islands.
All the analyses took into account the sampling design of the study. In the case of AF, specific prevalences were calculated by age and sex, as well as total prevalence and their 95% confidence intervals (95%CI).
Age- and sex-adjusted odds ratios were estimated using logistic regression models in order to identify cardiovascular risk factors and antecedents associated with the presence of AF. Subsequently, a multivariate model was adjusted for the variables with P<.01 in the bivariate analysis
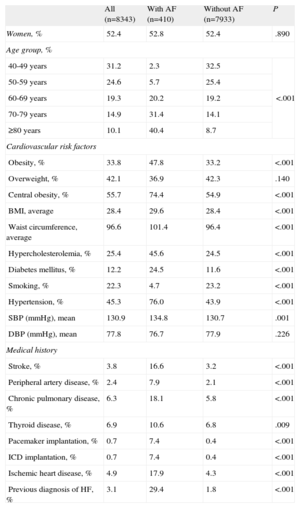
RESULTSThe study included 8343 participants (mean age, 59.2 [95%CI, 58.6-59.8] years; 52.4% women). Table 1 shows the general characteristics of the study population and, for purposes of comparison, the same population disaggregated into those with a diagnosis of AF and those without AF. In the study population, AF was diagnosed in 410 patients (204 men and 206 women). Of these, 267 had a diagnosis of AF on ECG on the day of examination. The remaining 143 patients had a documented history of AF but did not have AF on the day of examination (nonpermanent AF, 34.9% of all patients with AF).
Characteristics of the Population With and Without Atrial Fibrillation
| All (n=8343) | With AF (n=410) | Without AF (n=7933) | P | |
| Women, % | 52.4 | 52.8 | 52.4 | .890 |
| Age group, % | ||||
| 40-49 years | 31.2 | 2.3 | 32.5 | <.001 |
| 50-59 years | 24.6 | 5.7 | 25.4 | |
| 60-69 years | 19.3 | 20.2 | 19.2 | |
| 70-79 years | 14.9 | 31.4 | 14.1 | |
| ≥80 years | 10.1 | 40.4 | 8.7 | |
| Cardiovascular risk factors | ||||
| Obesity, % | 33.8 | 47.8 | 33.2 | <.001 |
| Overweight, % | 42.1 | 36.9 | 42.3 | .140 |
| Central obesity, % | 55.7 | 74.4 | 54.9 | <.001 |
| BMI, average | 28.4 | 29.6 | 28.4 | <.001 |
| Waist circumference, average | 96.6 | 101.4 | 96.4 | <.001 |
| Hypercholesterolemia, % | 25.4 | 45.6 | 24.5 | <.001 |
| Diabetes mellitus, % | 12.2 | 24.5 | 11.6 | <.001 |
| Smoking, % | 22.3 | 4.7 | 23.2 | <.001 |
| Hypertension, % | 45.3 | 76.0 | 43.9 | <.001 |
| SBP (mmHg), mean | 130.9 | 134.8 | 130.7 | .001 |
| DBP (mmHg), mean | 77.8 | 76.7 | 77.9 | .226 |
| Medical history | ||||
| Stroke, % | 3.8 | 16.6 | 3.2 | <.001 |
| Peripheral artery disease, % | 2.4 | 7.9 | 2.1 | <.001 |
| Chronic pulmonary disease, % | 6.3 | 18.1 | 5.8 | <.001 |
| Thyroid disease, % | 6.9 | 10.6 | 6.8 | .009 |
| Pacemaker implantation, % | 0.7 | 7.4 | 0.4 | <.001 |
| ICD implantation, % | 0.7 | 7.4 | 0.4 | <.001 |
| Ischemic heart disease, % | 4.9 | 17.9 | 4.3 | <.001 |
| Previous diagnosis of HF, % | 3.1 | 29.4 | 1.8 | <.001 |
AF, atrial fibrillation; BMI, body mass index; DBP, diastolic blood pressure; HF, heart failure; ICD, implantable cardioverter-defibrillator; SBP, blood pressure.
The overall prevalence of AF was 4.4% (95%CI, 3.8-5.1). The prevalence was similar in men (4.4% [3.6-5.2]) and women (4.5% [3.6-5.3]), rising with increasing age older than 60 years. The prevalence of AF by age and sex is presented in Table 2 and Figure 2.
Prevalence of Atrial Fibrillation by Sex and Age Group and Estimated Number of Patients in the Spanish Population
| Men (n=3829) | Women (n=4514) | Total (n=8343) | ||||
| Age | % | 95%CI | % | 95%CI | % | 95%CI |
| 40-49 years | 0.5 | 0.0-1.2 | 0.2 | 0.0-0.4 | 0.3 | 0.0-0.7 |
| 50-59 years | 0.9 | 0.3-1.6 | 1.1 | 0.1-2.1 | 1.0 | 0.4-1.7 |
| 60-69 years | 5.3 | 3.1-7.5 | 4.0 | 2.3-5.7 | 4.6 | 3.4-5.9 |
| 70-79 years | 11.9 | 8.9-14.9 | 7.2 | 5.1-9.3 | 9.3 | 7.4-11.2 |
| ≥80 years | 17.0 | 11.9-22.1 | 18.1 | 13.3-22.9 | 17.7 | 14.1-21.3 |
| Total | 4.4 | 3.6-5.2 | 4.5 | 3.6-5.3 | 4.4 | 3.8-5.1 |
| Age | Total (in thousands) | 95%CI | Total (in thousands) | 95%CI | Total (in thousands) | 95%CI |
| 40-49 years | 17.3 | 0.0-43.6 | 6.30 | 0.0-14.0 | 23.6 | 0.0-50.9 |
| 50-59 years | 26.7 | 9.26-44.2 | 31.6 | 0.49-62.6 | 58.3 | 21.4-95.2 |
| 60-69 years | 114.6 | 64.6-164.7 | 92.7 | 52.1-133.3 | 207.4 | 145.3-269.4 |
| 70-79 years | 183.0 | 131.8-234.1 | 138.9 | 97.5-180.3 | 321.8 | 252.9-390.9 |
| ≥80 years | 142.3 | 99.9-184.7 | 272.4 | 193.8-351.1 | 414.7 | 326.2-503.3 |
| Total | 483.9 | 394.9-572.9 | 541.9 | 437.4-646.5 | 1025.8 | 879.1-1172.6 |
95%CI, 95% confidence interval.
Regarding cardiovascular risk factors, patients with AF had a higher percentage of obesity (47.8% vs 33.2%; P<.001), hypercholesterolemia (45.6% vs 24.5%; P<.001), diabetes mellitus (24.5% vs 11.6%; P<.01), and hypertension (76% vs 43.9%; P<.01), and a lower percentage of smoking (4.7% vs 23.2%; P<.001) than patients without AF. Patients with AF more often had a history of cerebrovascular disease (16.6% vs 3.2%; P<.001), peripheral arterial disease (7.9% vs 2.1%; P<.001), pulmonary disease (18.1% vs 5.8%; P<.001), ischemic heart disease (17.9% vs 4.3%; P<.001) and a history of heart failure (29.4% vs 1.8%; P<.001) (Table 1).
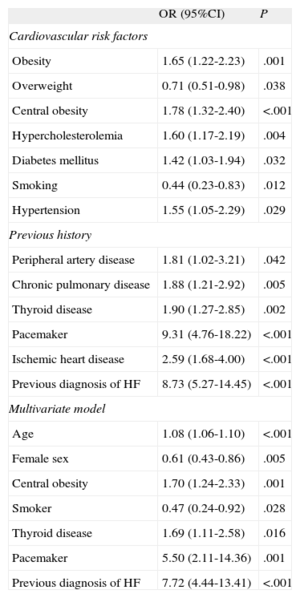
Multivariate analysis showed that age, male sex, central obesity, not smoking, a history of heart failure, thyroid disease, and having a pacemaker were independently associated with the presence of AF (Table 3). Although no differences were found in the prevalence of AF by sex, differences were found by decade, with a higher prevalence in men less than 80 years of age and in women more than 80 years of age. These data are in line with those of other studies, except for the finding of a higher prevalence in women in their eighties. Of the 410 patients with AF, 41 (10%) were diagnosed on the day of the examination (unknown AF).
Age- and Sex-adjusted Odds Ratios of Having Atrial Fibrillation for Each Cardiovascular Risk Factor, Previous History, and Final Multivariate Model
| OR (95%CI) | P | |
| Cardiovascular risk factors | ||
| Obesity | 1.65 (1.22-2.23) | .001 |
| Overweight | 0.71 (0.51-0.98) | .038 |
| Central obesity | 1.78 (1.32-2.40) | <.001 |
| Hypercholesterolemia | 1.60 (1.17-2.19) | .004 |
| Diabetes mellitus | 1.42 (1.03-1.94) | .032 |
| Smoking | 0.44 (0.23-0.83) | .012 |
| Hypertension | 1.55 (1.05-2.29) | .029 |
| Previous history | ||
| Peripheral artery disease | 1.81 (1.02-3.21) | .042 |
| Chronic pulmonary disease | 1.88 (1.21-2.92) | .005 |
| Thyroid disease | 1.90 (1.27-2.85) | .002 |
| Pacemaker | 9.31 (4.76-18.22) | <.001 |
| Ischemic heart disease | 2.59 (1.68-4.00) | <.001 |
| Previous diagnosis of HF | 8.73 (5.27-14.45) | <.001 |
| Multivariate model | ||
| Age | 1.08 (1.06-1.10) | <.001 |
| Female sex | 0.61 (0.43-0.86) | .005 |
| Central obesity | 1.70 (1.24-2.33) | .001 |
| Smoker | 0.47 (0.24-0.92) | .028 |
| Thyroid disease | 1.69 (1.11-2.58) | .016 |
| Pacemaker | 5.50 (2.11-14.36) | .001 |
| Previous diagnosis of HF | 7.72 (4.44-13.41) | <.001 |
95%CI, 95% confidence interval; HF, heart failure; OR, odds ratio.
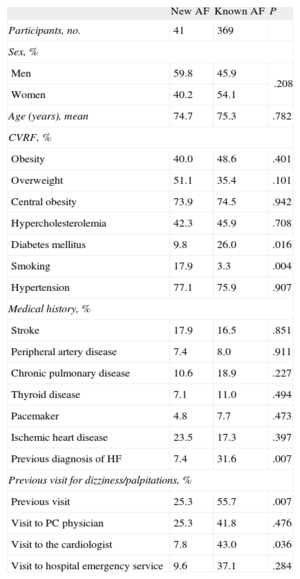
Among patients with undiagnosed AF, there were higher percentages of patients without diabetes, smokers, and patients without a history of heart failure. Furthermore, this group had fewer symptoms as indicated by the fact that dizziness or palpitations were less often cited as the reason for their visit (Table 4).
Characteristics of the Population With New Atrial Fibrillation and Previously Diagnosed Atrial Fibrillation
| New AF | Known AF | P | |
| Participants, no. | 41 | 369 | |
| Sex, % | |||
| Men | 59.8 | 45.9 | .208 |
| Women | 40.2 | 54.1 | |
| Age (years), mean | 74.7 | 75.3 | .782 |
| CVRF, % | |||
| Obesity | 40.0 | 48.6 | .401 |
| Overweight | 51.1 | 35.4 | .101 |
| Central obesity | 73.9 | 74.5 | .942 |
| Hypercholesterolemia | 42.3 | 45.9 | .708 |
| Diabetes mellitus | 9.8 | 26.0 | .016 |
| Smoking | 17.9 | 3.3 | .004 |
| Hypertension | 77.1 | 75.9 | .907 |
| Medical history, % | |||
| Stroke | 17.9 | 16.5 | .851 |
| Peripheral artery disease | 7.4 | 8.0 | .911 |
| Chronic pulmonary disease | 10.6 | 18.9 | .227 |
| Thyroid disease | 7.1 | 11.0 | .494 |
| Pacemaker | 4.8 | 7.7 | .473 |
| Ischemic heart disease | 23.5 | 17.3 | .397 |
| Previous diagnosis of HF | 7.4 | 31.6 | .007 |
| Previous visit for dizziness/palpitations, % | |||
| Previous visit | 25.3 | 55.7 | .007 |
| Visit to PC physician | 25.3 | 41.8 | .476 |
| Visit to the cardiologist | 7.8 | 43.0 | .036 |
| Visit to hospital emergency service | 9.6 | 37.1 | .284 |
AF, atrial fibrillation; CVRF, cardiovascular risk factors; HF, heart failure; PC, primary care.
The Spanish 2011 census estimated the population to be 46 815 916 inhabitants; of these, 51.1% (23 922 933 people) were older than 40 years of age. By applying the specific prevalences for age and sex observed in the OFRECE study to the Spanish population, and taking into account the design, the number of patients with AF in the population older than 40 years in Spain (with the exception of Cantabria, Ceuta, and Melilla) was estimated to be 1 025 846 (95%CI, 879 077-1 172 614), of whom 94 546 (95%CI, 57 944-131 148) would be undiagnosed.
DISCUSSIONThis study is the first to provide estimates of the prevalence of AF in the Spanish population older than 40 years of age and shows that the prevalence of AF in this population increases with age. The strength of this study lies in the fact that it was conducted using the general population and that a highly representative sample was obtained by the random selection of PC physicians and the population assigned to each physician, thereby strengthening the validity of the results. Previous studies have been based on the records of patients with other cardiovascular diseases (eg, hypertension) or on specific geographical areas, which has led to widely varying estimates, with prevalences between 0.7% and 8.5%.8–11 The REGICOR study,9 the only study conducted in the general population rather than in patients from different areas, found a prevalence of 0.7%. However, that study was strongly limited by its exclusion of the population older than 74 years of age, precisely the age group with the highest prevalence of AF. In the PREV-ICTUS study,10 a population-based cross-sectional study that analyzed participants older than 60 years, the prevalence of AF was 8.5% (95%CI, 7.9%-9.2%), was higher in men (9.3% vs 7.9% in women), and increased from 4.2% in those aged between 60 and 64 years to 16.5% in those older than 85 years. The CARDIOTENS study,8 which was conducted in hypertensive patients, found a prevalence of AF of 4.8%, which increased with each decade of life (1.0% in those younger than 50 years and 11.1% in those older than 80 years). However, CARDIOTENS cannot be considered a population-based study because it included consecutive patients attending PC centers or cardiology services, which could have led to a selection bias that overestimated prevalence.
European studies have also reported wide variability in prevalences in the general population, with estimates ranging from 0.2% to 1.2% and, for people older than 50 years of age, from 1.5% to 5.5%.2,15–19 Most of the studies that have investigated the prevalence of AF are not strictly comparable for 2 reasons: a) the characteristics of the study population and their distribution by age and sex, and b) the method used to diagnose AF. Studies that based the diagnosis of AF on ECG alone, and not on a history of AF, found lower prevalences than those that based the diagnosis on ECG and a clinical history of AF.15 Another aspect that may influence the prevalence of AF in different series, as confirmed in this study, is the risk profile of the populations analyzed (prevalence of hypertension, diabetes mellitus, obesity, etc). In the case of the Spanish population, recent studies have demonstrated a high prevalence of variables associated with AF, which are not always well adjusted.20,21 In this study, all ECGs were read centrally by 2 cardiologists, which increased the quality of the information by enhancing diagnostic certainty and reducing variability and misclassification problems.
Interestingly, 10% of patients with AF at the time of examination were unaware of having AF. This figure is slightly different from that described by Labrador et al.11 or Wheeldon et al.,16 who found that 8.6% and 7.7% or more of patients had undiagnosed AF, respectively. However, both these studies only analyzed the general population aged 65 years and older, and therefore the data are not directly comparable.11,16 It should be noted that there were higher percentages of men, patients without diabetes, smokers, and patients without a history of heart failure in the population of patients with previously undiagnosed AF (an arrhythmia that may cause few symptoms). This finding is very important because patients with AF have a 5-fold higher risk of a stroke22 and because effective treatment is available using classical or novel anticoagulants to prevent these embolic events.23,24
LimitationsThe hospitals studied within each province were not randomly selected. This probably had very little impact on the study as it is unlikely that the prevalence of AF varies significantly between adjacent areas. Of more importance, the randomized selection of the physicians and particularly of the patients assigned to each physician was considered to add strength to the results of this study. The high number of sampling points improved the representativeness of the sample, which is sometimes difficult to evaluate. A limitation inherent to this type of general population study is that the participants may differ from nonparticipants. Although it is impossible to completely rule out potential bias due to selective participation and to determine its direction, it should be emphasized that any such bias cannot be very large, since there was a very good participation rate for this type of study (76% of those invited to participate in the study) and, of the nonparticipants, only one-third did not participate due to refusal. Another limitation is that the patients without a known history of paroxysmal AF and with a normal ECG at the time of examination by the family physician were not diagnosed with AF; however, this limitation is common to all published studies on the prevalence of AF and is difficult to avoid. Furthermore, when AF was diagnosed on the basis of clinical history alone, a centralized reading of the previous ECG was obviously not possible; nevertheless, a diagnosis of AF was only included in the study if such a reading was recorded in a medical record or the clinical history in PC.
CONCLUSIONSThe prevalence of AF in the general Spanish population older than 40 years is high (4.4%). The overall prevalence is similar in men and women, but differs according to the decade of age analyzed and increases steeply above 60 years of age. There are over 1 million patients with AF in the Spanish population, of whom more than 90 000 are undiagnosed. This has important implications for public health due to the frequency and severity of complications caused by this arrhythmia in the absence of treatment.
FUNDINGThe OFRECE study was supported by the Research Agency of the Spanish Society of Cardiology (Agencia de Investigación de la Sociedad Española de Cardiología). This study was made possible by financial support from SANOFI, which was not involved in the study design, data analysis, or preparation of the final manuscript, and partly (pilot study) by the Observatorio de Salud de la Mujer, the Observatorio del Sistema Nacional de Salud, the Agencia de Calidad del Sistema Nacional de Salud, and the Ministerio de Salud y Consumo.
CONFLICTS OF INTERESTNone declared.
The authors acknowledge the assistance of the Steering Committee, coordinators, researchers and collaborators listed in the Appendix, and the following institutions which contributed to the development of the study: Consejería de Salud de la Junta de Andalucía; Servicio Aragonés de Salud, Gobierno de Aragón; Consejería de Sanidad del Principado de Asturias; Servicio de Salud de Castilla-La Mancha; Consejería de Sanidad de la Junta de Castilla y León; Conselleria de Salut de la Generalitat de Catalunya; Conselleria de Sanitat de la Generalitat Valenciana; Consejería de Sanidad, Gobierno de Extremadura; Consellería de Sanidade de la Xunta de Galicia; Conselleria de Salut i Consum, Gobern de les Illes Balears; Consejería de Sanidad, Gobierno de Canarias; Consejería de Sanidad, Gobierno de la Rioja; Consejería de Sanidad de la Comunidad de Madrid; Consejería de Sanidad y Política Social, Región de Murcia; Consejería de Sanidad, Gobierno de Navarra, and Consejería de Sanidad del Gobierno Vasco. We also thank ODDS S.L. as the coordinating center and for data analysis. We also extend special thanks to Soly Santiago Perez, for data analysis, Teresa Rosalía Perez Castro, for managing the database, training the participating physicians, and coordinating work field, and M. Luisa López Domínguez, for her administrative work and call-center coordination.
| Steering Committee | |
| Executive Committee | Juan José Gómez-Doblas, Servicio de Cardiología, Hospital Clínico Universitario Virgen de la Victoria, Málaga; Javier Muñiz, Instituto de Ciencias de la Salud, Universidad de A Coruña, A Coruña; Joaquín J. Alonso Martín, Servicio de Cardiología, Hospital Universitario de Fuenlabrada, Fuenlabrada, Madrid; Eulalia Roig, Servicio de Cardiología, Hospital de Sant Pau, Barcelona |
| Scientific Committee | Gustavo Rodríguez-Roca, Centro de Salud La Puebla de Montalbán, Toledo; José Maria Lobos, Centro de Salud Villablanca, Madrid; Gaietá Permanyer, Servicio de Cardiología, Hospital Universitari Vall d’Hebron, Barcelona; Manuel Anguita, Servicio de Cardiología, Hospital Reina Sofía, Córdoba |
| Coordinators, researchers and collaborators | |
| Autonomous community | Province | Coordinator | Primary care researchers and collaborators |
| Andalusia | Almería | Jacinto Benítez Gil | Francisco Garzón Montero; Virginia Bueno del Campo; Carmen Montabes Pereira; Santiago López Fábrega; Francisco Javier Almecija Flores; Eduardo C. Mecández García. Collaborators: Jesús Enrique Montoro Robles, Manuela González López |
| Cádiz | Manuel Ruiz Ruiz | Juan Carlos Molina Deudero; Inmaculada País Mateos; Javier Rodríguez Conejo; Dolores Montero Fuentes-Guerra; Myrian Olivares Morales; Raquel de Lara Muñoz; Milagros Pérez López; Francisco Umbría Campoo; José María Tenorio Sánchez | |
| Córdoba | Manuel Anguita Sánchez | Emilio García Criado; Jorge Martínez de la Iglesia; Juana Redondo Sánchez; Enrique Martín Rioboo; Juana María González Barranco; Francisco Javier Ruiz Moruno; María Auxiliadora Cabanás Espejo; Trinidad Lechuga Varona; Cristina Aguado Taberne; Juan José García Gallego. Collaborators: Antonia Calero Espino | |
| Granada | Pablo Toledo Frías | Nieves Hitos Henares; Rosario López Bueno; Adoración Caba Martín; Concepción Molina Serrano; Concepción Macía Canon; Pedro Tejeda Paredes; Antonieta Maldonado Larroque. Collaborators: Amparo Arrabal Martín, Agustina Matilla Marcos | |
| Huelva | Carlos Sánchez González | Antonio Ortega Carpio; M. Eloisa Arias Fortes; Javier Ferraro García; Migliane Lima Costa; Isabel Ruiz Cumplido; Pilar Freire Pérez | |
| Jaén | Eduardo Vázquez Ruiz de Castroviejo | Ramiro Aguilera Tejero; Fermina Bruque Sánchez; Pablo Tallón Povedano; Lorenzo Escabias Andreu; Víctor Figueroa Cardona; Alejandro Pérez Milena; José Moraleda Martínez; M. Dolores Rodríguez Serrano | |
| Málaga | Juan Robledo Carmona | Amparo Aragón Ramírez; Carlos Gutiérrez Maturana Camañes; Concepción Cañero Criado; Cristina Delgado Utrera; Dolores Muñoz Galán; Ignacio Boto Gutiérrez; Juan Luis Villamor Bueno; Vicente Villatoro Jiménez; Victoria Alcaraz Martínez. Collaborators: Belén Pajariño Gallego, Jacinta Meléndez Ortigosa, Vicente Raimundo Arrabal Pérez, Alberto Márquez López, María del Pilar Aguilar Trujillo | |
| Seville | Antonio Casco Gallardo | ||
| Aragón | Huesca | Javier Escota Villanueva; Mariano Rodríguez Torrente | Eva Aguaron Joven; José María Borrel Martínez; Juan Manuel Culebras Marco; Dolores Idañez Rodríguez; Teófilo Lorente Aznar; Ana Rivera Fuertes; Carmen Quintana Velasco; Carlos Aisa Arenaz; José María Barrio Navascues; José María Castillo Olivera. Collaborators: Inmaculada Lera Omiste, Gemma Ciria |
| Zaragoza | Ricardo Gayán | Ana Avelino Terrón; M. Luisa Aznar Arribas; Pedro J. Marín Velázquez; Adolfo Benito Jiménez; Rafael Vargas Arévalo; José Fernando Pina; Jesús Fco. Romeo Ladrero; M. Asunción Alfaro Lozano; José Javier Calvo García; Jesús María Lasso Moreno | |
| Principality of Asturias | Asturias | Inés Möller Bustinza | M. Teresa Saldaña Hernández; Manuel Berrocal Varela; Amador Jenaro Carbajal Cocina; Francisco Javier Claros González; Natalia Juesas Fernández; Joaquín Prieto Gutiérrez; Agustín Sánchez Hernández; Purificación Seijo González; Ana Picasso Martínez de Ubago |
| Castile-La Mancha | Albacete | Moisés Barambio Ruiz | Antonio Cifuentes Verdú; Concepción Escolano Vizcaíno; Francisco Javier Ayllón Ayllón; Francisco Lorenzo Salido; Cándido Martínez García; María Concepción Casado Moragón; Antonio Martínez Lozano; Lucinio Carrión Valero; José Miguel Ocaña López; Mirian Martínez Carretero |
| Ciudad Real | Luis Ruiz-Valdepeñas Herrero | Raquel Bañón García; M. Teresa Alcaide Cornejo; Cristina Herráiz Serrano; Antonio Guindas Ruiz; Andrés Herrera Canales; Antonio-Lorenzo Ruiz Serrano; Francisco de Asís Asenjo Hernández; Angel Fermín Pérez Sánchez; Alfonso Ruiz-Póveda García-Rojo; M. Isabel Ariza Sánchez | |
| Cuenca | Antonio Melero Pita | Isidro Sanz Polo; Rafael Morilla Ramilo; Joaquín Román López Villar; Fernando Madero López; Alfredo Cabrejas Sánchez; Rosa M. Cejudo Serrano; Jesús Buendía Bermejo; Sagrario Saiz Santos; Adoración Romero Saiz; Julia Martín Lezana | |
| Toledo | Luis Rodríguez Padial | Raquel Parejo Míguez; José Ignacio Jaén Díaz; Angel Alonso Alía; Alberto Sepúlveda Martín; María Vega Martínez Escudero; Miguel Laborda Peralta; José María Jiménez Rodríguez; M. Angeles Adán Valero; Francisco Javier Alonso Moreno; Carmen Ramos López. Primary care collaborators: Irene Martínez Giner, Jesús Adrián Sifuentes Hernández, María Dolores Martínez Malabia, Victoria Madiedo Acosta | |
| Castile and León | Ávila | Igor Molina Puente | Miguel Angel Fernández Gutiérrez; Carlos de Cabo González; Lidia Sastre Jiménez; F. Javier Ríos Almarza; Blanca Noreña Delgado; Cesarina Rivas Hernández; Carlos Javier García Gómez; Juan Luis Martín Clavo; Alfonso Carlos Caro Picón; Benigno Sánchez Martín |
| Burgos | Germán Pérez Ojeda | Angel María Olea Movilla; Pedro Luis Estables Recansens; Lucinio Anaya Bernabe; Carmen Caballero Abad; Jesús García Cuadrillero; M. Felisa Lara Caballero; Benito Sanz Mozo; Felipe Eulalio Martín Rosón; M. Cruz González González | |
| Leon | Norberto Alonso Orcajo; Raúl Carbonell de Blas; Cristina Pascual Vicente; Agustín Romero Blanco | Leonor Martín Santín; M. Isabel Fernández Marassa; Mercedes García de Celis; Elena Fernández Mielgo; Faustino Sánchez Sanmartino; Margarita Gallego de la Varga; Angel Novoa Mato; Ana Isabel Barragán Marín; Jesús Marino Villamar Berceruelo | |
| Palencia | Chema Asín Guillén | Juan Antonio Losmozos Sánchez; José Luis Durand Eguiluz; María Carmen Monge González; Enrique de Inés Martín; José Manuel Zumel Elices; Juan Manuel Durantez Cacharro; Tomás Manzano Benito; Isaac Alcalde García; M. Eugenia Barón Laguna | |
| Salamanca | Javier Jiménez Candil | Javier García Izquierdo; Julio Guerrero del Olmo; Luis García Ortiz; Carlos Hernán-Pérez Leal; José Calama Becerro; Carmen de Antonio Jiménez; Manuel Becerro Cereceda | |
| Segovia | Carlos Junquera Planas | Emilio García Ortega; Rosa María Fernández Santa Teresa; M. Concepción Manrique de la Fuente; Juan Francisco Gil García; Martín Merino Segovia; Fernando Mondejar Quirós; Javier González Perlado; Ana Isabel Herrero Cecilia; José de Pablo Álamo | |
| Soria | Valentin del Villar Sordo | M. Jesús de Pablo Ramos; Ana M. Cabrerizo Puente; M. Antonia Hernández Caballero; Antonio Alberto Gil Gómez; Francisco Javier Martínez Sanz; Luis Gutiérrez Moreno; Elena de Pablo Ramos; Ramón García Martínez; Angel Lafuente Esteban; Gema Borque Molinos | |
| Valladolid | María Jesús Rollán Gómez | Rocio Velasco Pastor; M. Jesús Aller de la Fuente; Mercedes Redondo Valdeolmillos; Jesús María Aguilar García; Verónica Casado Vicente; Elpidio García Ramón; Luis Angel Herrán Oteruelo; Jesús Francisco García Rodríguez; Enrique Sanz Monedero; Ruperto Sanz Cantalapie Collaborator: Miguel Angel Morales Torres | |
| Zamora | José Antonio Ortiz de Murua López | Angela Nistal Ramos; Francisco Javier Delgado Rodríguez; Luis Garrote Gutiérrez; Antonia Refoyo Enríquez; M. Dolores Rodríguez Martín; Pedro Martín Martín; Clodoaldo Pérez Ramos; Mercedes Prieto Mantellán; Gabriel González Panero; Alberto Jiménez Meléndez | |
| Catalonia | Barcelona | Amparo Álvarez Auñón; Vicens Brossa Loidi | Sandra Sabarich Flores; Judit Novo Salvador; Montserrat Llordés Llordés; María Eugenia Pérez Domínguez; Telma Cristina Vicentín; Francisco Javier Martínez Quílez; Francisco Javier Avilés Fernández; Laura Diaz Gete; Alicia Mostazo Muntané; Amelia Espinosa Santana; Antonia Llauger Roselló; M. Dolors Moriano García; Jordi Nadal Echevarria; M. Angels Salvador Millán; Herminio Moliner Lizondo. Collaborator: Monserrat Roca Vilalta |
| Girona | Joan Sala Montero | Josep Gil Yubero; Ferrán Cordón Granados; Montse Lloveras Clos; Emili Marco Segarra; Ramón Creus Bosch; Carmen López Sanmartín; Dídac Parramón i Font; Begoña Santana de Carlos; Cristina Servent Batlle. Collaborators: Judith Pinsach Garanger, Laura Vegas Fernández | |
| Lleida | Fernando Worner Diz | Jorge Soler González; Marta Ortega Bravo; Antonio Rodríguez Rosich; Plácido Santafe Soler; Eduard Peñascal Pujol; José Masamunt Jove; José Luis Morera Serra; Olga Pérez Queiruga; Antoni V. Plana Blanco | |
| Tarragona | Jordi Mercé Klein | Merce Peri Viñes; Elisabeth Salsench Serrano; Eva María Oya Girona; Francisco Martín Luján; Rosa María Lara Ibáñez; Rafael Albiol Lluis; Ferrán Grifoll Ruiz; Irene Pascual Palacios; Dolores Gazol Soler | |
| Valencian Community | Alicante | Alberto Cordero Fort | Manuel Carlos Salas Tomás; Rosario García Santafe; Nieves Gómez Moreno; Salvador Pertusa Martínez; Soledad García Bevia; Luis Richard Rodríguez; Alberto Asencio Aznar. Collaborator: María Adsuar Adán |
| Castellón | Lorenzo Fácila Rubio | José Vicente Herrero Ballestar; Beatriz Sánchez-Peral Sánchez; Amparo Antón Aguilera; M. José Manrique Costa; Manuel Batalla Sales; María Isabel Martí Giner; María Teresa Aguilar Arnau; M. Angeles Goterris Pinto; M. Dolores Aicart Fort; M. José Monedero | |
| Valencia | Francisco Ridocci Soriano | Fernando Quiles Añón; Juan Carlos Beguer Miquel; Asunción Girbes Revert; M. Angels Pages Juanola; María Teresa Villalba Calatayud; Amparo Castro Lorente | |
| Extremadura | Badajoz | Antonio Merchán Herrera | Macarena Candela Maestú; Juan José Dorado Martín; Antonio García Concellón; María S. Gil Llinás; Calixta Mantilla Calderón; Manuel Martínez de la Concha; Beatriz Pardo Díaz de Entresotos; Rosario T. Trinidad Ramos; José A. Morales Ruiz |
| Cáceres | José Javier Gómez Barrado | Fernando Pérez Escanilla; Carlos Arjona Mateos; Dimas Igual Fraile; Amparo Gómez Espárrago; M. Socorro Gacto Fernández; José Polo García; Sebastián Traba Hernández; Sabina Rodríguez Borreguero; Alfonso Barquilla García | |
| Galicia | A Coruña | José Angel Rodríguez Fernández | David Bouza Álvarez; Luis Buendía Fernández; Francisco Javier Maestro Saavedra; Manuel Barral Castro; Juan Manuel Peteiro Martínez; José Luis Díaz Santiago; Concepción Blanco Sánchez; Cristina Iglesias Díaz |
| Lugo | Ana Testa Fernández | Germán Fernández López; José Enrique Cajiao Bonome; José Manuel Menéndez Tamargo; Cristina Arijón Barazal; Vicente Quirós Madariaga; Domingo D. García Rivas; Domingo Fernández Méndez; M. Teresa García Novo; Bernardino Pardo Teijeiro | |
| Ourense | Manuel García García | Rosario Calle Custodio; Alberto J. del Alamo Alonso; Pedro Blanco Iglesias; Antonio Pedreira Penedo; M. Dolores Antolín Novoa; Ana Veiga Vázquez; Agapito Diéguez Estévez; Jorge Lloveres Insua; Aida Robles Castiñeiras | |
| Pontevedra | Francisco Calvo Iglesias | Evangelina Filloy Miguez; José Carlos Sendín Sánchez; Xesús Fernández Núñez; Juan José Crespo Sabaris; José Rubio Panadeiros; M. Luisa Blázquez Ballesteros; Manuel Domínguez Sardiña; M. Begoña Porritt Lueiro; Manuel M. Lorenzo San Martín; Francisco López Sobrino | |
| Balearic Islands | Mallorca | David Crémer Luengos | Natalia Feuerbach Achtel; Montserrat de la Torre Vidal; Alejandro Pizá Colom; Adriano Juan Mayrata Vicens; Cristina Gadea Ruiz; Catalina Picornell Yanes; Montserrat Sauleda Pares; Carmen López Moreno; Francisca Bestard Reus; Silvia Martín Delgado |
| Canary Islands | Las Palmas | M. Antonia Viña Liste | Pedro J. Díaz Alayón; Luis Antonio Escalada Muñoz; Juan Pedro Jiménez Sarmiento; Beatriz Pérez López; Domingo Guerra Vega; Emilio Sánchez Carrión; Javier Santana Quilez; Gloria Calero González; Tomás González Rodríguez; Carmen Berrio Santana |
| Sta. Cruz de Tenerife | Horacio Pérez Hernández | Nicolás Maffiotte Carrillo; Juan Francisco Tejera Cabrera; Alfredo Bartolomé Andrés; Emma Navarro Brito; Francisco José Castro Álvarez | |
| La Rioja | La Rioja | Adrián Beloscar Llorca; Alfonso Jiménez Galán | José Tomás Gómez Saenz; Juan Manuel Marrodan Adan; Julio Peña Angos; Alejandro Paradiñeiro Somoza; Jesús M. Gutiérrez de Bobadilla; José María Martínez Martínez; Ignacio Fernández Hurtado; Mikel Ugalde Olano; Juan José García Díaz; Oscar León Fernández |
| Community of Madrid | Madrid | José María Serrano Antolín | Antonio Sánchez Serrano; Belén Muñoz Gómez; M. José García Sacristán; Rocío Balas Urea; M. José Rojas Giraldo; Mar Noguerol Álvarez; Carlos Díaz Gómez-Calcerrada; Ignacio Arjona Anchoriz; Rocío Vello Cuadrado |
| Region of Murcia | Murcia | Manuel Villegas García | María Xania de Casas Fernández; Rafael Luquín Martínez; Antonio Javier Llorens Minguell; M. del Carmen Paniagua Merchán; Concepción Carvajal Lucerga; Montserrat Martínez Sánchez; M. Isabel Caceres López; M. José Miras Martínez; Manuel Haenelt Maguel; Ana Celia Melgar García |
| Chartered Community of Navarre | Navarre | Marisol Alcasena Juango | Vicente Estremera Urabayen; Juan Manuel Pérez Gómez; Ramón Villanueva Moreno; M. Teresa Salinas Videndo; M. del Mar Hernández Espinosa; Carlos Figuero Echeverria; José Manuel Calleja Pascual; Arturo Erlanz Abad; Jesús Javier Jurio Burgui |
| Basque Country | Álava | Maruja Bello Mora | Jon Azkarate Zubiaur; M. Asunción Aldecoa Eguillor; Juan Francisco Pérez de San Román Setien; Laura Ortiz de Lazcano Herrera; Lucia Pereda López; María Angeles Calvo Gainzarain; Olga Ruiz de Arbulo Ruiz de Alegría; Juan Carlos Martín Fernández Landa; Luis Laborda González; Francisco Javier Blanco Cuadra |
| Guipúzcoa | Esther Recalde | José Ramón Chopitea Gabiola; Aintzane Abasolo García; Miguel Mier Cascallana | |
| Vizcaya | Nekane Murga Eizagaetxebarría | Ana Isabel Izaguirre Berasategui; Juan Bautista Loizaga Horno; Cristina Lekube Angulo; José Angel Del Pozo Yruegas; Alazne Ramoneda Errazquin; Igone Asua Angulo; Epifanio Álvarez Grande; María Natividad de Soto Gorroño; Rosario Angulo Rivero | |
| Electrocardiogram reading center | |||
| Center | Coordinator | Other members of the group |
| Hospital Universitario de Fuenlabrada (Madrid) | Paula Awamleh García | Alejandro Curcio Ruigómez; Carmen Cristobal Valera; Adolfo Fontenla Cerezuela; Catherine Graupner Abad; Rosa María Jiménez Hernández; María Luaces Méndez; José María Serrano Antolín; Pedro Talavera Sánchez; Rodrigo Teijeiro Mestre |