Keywords
The appendix contains a list of the participating researchers and hospitals in the CORSAIB (COR SA a les Illes Balears) study.
This project was funded by Conselleria de Sanitat i Consum del Govern Balear, grant FIS PI01/1717 from the Spanish Ministry of Health, project ERICE Red Española Epidemiología Cardiovascular G03/065, and network IAP G03/170.
Received April 5, 2005. Accepted for publication August 18, 2005.
INTRODUCTION
Since the 1970s, a reduction in cardiovascular mortality has been observed in the Western World. While France is the only European country with a lower cardiovascular mortality than Spain, cardiovascular disease continues to be the largest cause of death in the Spanish population.1,2
Substantial regional differences exist in mortality and in the reduction of mortality rates. The annual reduction from 1975 to 1992 varied from 3.3% in Navarra to 1.7% in the Autonomous Community of Murcia.2
The Balearic Islands has been considered one of the regions with the highest rates of cardiovascular mortality3,4; it was considered to have one of the highest rates of potential years of life lost and had the second lowest reduction in cardiovascular mortality compared with other autonomous communities in Spain.2 Recently, the IBERICA study showed that the indices are not, in fact, so bad and should be corrected, since the figures included patients who died in the Balearic Islands but whose residence was elsewhere.5 Furthermore, the growth of the population in recent years has been much higher than the national average and the population projections used to calculate regional mortality rates in between-census periods. Similar findings have been reported for another tourist area, the Canary Islands.6
It is particularly important to determine the prevalence of the main cardiovascular risk factors (CRFs) in order to develop prevention plans to reduce cardiovascular morbidity and mortality. Therefore we have addressed the prevalence of the main CRFs and of diagnosed cardiovascular disease in the Balearic Islands population aged between 35 and 74 years.
SUBJECTS AND METHOD
Design
A population-based descriptive cross-sectional study was undertaken in a representative sample of the adult population between 35 and 74 years of age resident in the Balearic Islands in 1998 (340 675 individuals out of a total of 796 438 inhabitants of the islands, according to the Instituto Balear de Estadística, the office of statistics for the Balearic Islands). A sample of 1824 individuals was calculated to be necessary in order to estimate the prevalence of CRFs with a 95% confidence interval (CI) and a relative accuracy of within 20% of the estimated prevalence for any given CRF.
To ensure that the sample was representative, the Balearic Islands were divided into 14 geographic sectors of between 45 000 and 53 000 inhabitants. Each sector corresponded to between 2 and 4 healthcare regions. General practitioners (GPs) were invited to participate and the involvement of 3 to 4 doctors per sector was obtained.
The database used for the sample was the record of individual health cards, which at that time covered 94% of the censored population of the Balearic Islands. For each geographic sector, the population structure was calculated according to decades and sex. A simple random sample was obtained from the population assigned to each doctor and it was confirmed to be proportional to the age and sex of the sector.
Thus, 64 individuals were randomly selected from the patients assigned to each of the 50 recruited doctors, 40 patients to achieve a sample of 2000 and 24 patients as reserves to substitute individuals who did not respond or were not eligible. Each individual was sent a letter on 2 consecutive occasions asking them to attend an appointment with their doctor. If they did not attend, attempts were made to establish contact by telephone. If the selected individual visited the doctor for other reasons, the doctor, having previously identified the medical history of each of the selected patients, arranged a specific appointment and obtained signed consent. Patients who refused to participate or could not be contacted were substituted by one of the 24 reserves from the same age and sex group.
The ethical committee for clinical research in the Balearic Islands (Comité Ético de Investigación Clinica de Baleares) approved the project, including the informed consent documents for participation in the study and the storage and use of biological samples.
The fieldwork was performed in 2000.
Clinical and Analytic Measurements
At the appointment, the doctor administered a questionnaire that included sex, age, education, employment status, history of myocardial infarction, cerebrovascular disease, peripheral artery disease, arterial hypertension (AHT), diabetes, dyslipidemia, medication, smoking, physical exercise in work and free time, and family history of cardiovascular disease. The data were compared with the patient's medical history at the health center.
The physical examination included weight, height, waist size, blood pressure, and heart rate. Blood pressure was assessed in both arms at the beginning of the appointment, after at least 5 minutes rest, and at the end of the appointment, around 20 minutes later (assessing blood pressure in the arm that had showed the highest values). If the second measurement differed from the first by more than 5 mm Hg or the pulse showed arrhythmias, the measurement was repeated and the mean of the 2 latter measurements recorded. Measurements were made using Omron 711 blood pressure monitors, which have been validated previously.7 Calibration was certified by the manufacturer and was checked twice during the study. Patients were considered hypertensive if they were taking antihypertensive medication or if the mean blood pressure from the 2 measurements performed in the same arm was greater than or equal to 140 mm Hg for the systolic arterial pressure (SAP) or greater than or equal to 90 mm Hg for the diastolic arterial pressure (DAP).
The day after the initial appointment, a blood sample was obtained following a 12 hour nocturnal fast to determine the concentrations of glucose (hexokinase method; DAX 72 analyzer, Bayer Diagnostics), total cholesterol (cholesterol esterase enzymatic method; DAX 72 analyzer), high-density lipoprotein cholesterol (HDL-C) (direct method using catalase; DAX 72 analyzer), and triglycerides (Trinder method; DAX 72 analyzer). Measurements were performed in the laboratories of the following hospitals: Hospital de Can Misses (Ibiza), Hospital de la Verge del Toro (Menorca), Hospital de Manacor (Mallorca), and El Carme (Hospital Universitario Son Dureta de Palma), which acted as the coordinating laboratory and was responsible for quality control.
Patients were considered to be diabetic if they received treatment with insulin or oral antidiabetic drugs, or if their fasting glucose level was greater than or equal to 126 mg/dL; they were considered smokers if they reported having smoked in the last 6 months; hypercholesterolemic if their total cholesterol was at least 250 mg/dL; obese if they had a body mass index (BMI) of at least 30; and overweight if their BMI was between 25 and 30. The questionnaire from the 1997 National Health Survey was used to assess whether individuals were sedentary according to whether they themselves declared that to be the case or that they did not undertake regular exercise in their free time.
All participating doctors received an instruction manual and attended training workshops to ensure homogeneity of patient interviews and examinations. To this end, a video prepared by the Mallorca Health Communication Group (Comunicación y Salud de Mallorca) was used. Participating doctors were accredited as field researchers with a signed agreement to follow the protocol.
Statistical Analysis
The mean (SD) was calculated for quantitative variables, since they were considered to fit a normal distribution. Point estimation of the prevalence of the different CRFs was calculated using the 95% confidence interval (CI). Individual coronary risk at 10 years was calculated using the original Framingham formula8 and calibrated for the Spanish population.9 The results presented were obtained following weighted adjustment to the true population. However, the small deviations made very little difference to the results. Statistical analysis was performed using SPSS for Windows version 8 and Epiinfo version 6.
RESULTS
The number of participants was 1685, 92.5% of the sample calculated to be necessary. Of the patients who were included in the study, 77.4% were preselected and the rest were reserves. Patients were contacted by letter or telephone in 72% of cases; the rest were contacted in the health centers. Of the 554 individuals who did not participate, 42% were not eligible (census errors, deaths, absences, changes of address, etc) and 6% refused permission for a blood sample to be taken; the remainder refused to participate without indicating their reasons.
The sample contained 52% women. Table 1 shows the distribution of the groups according to age and sex of the sample and the study population. The sample contained 52% of individuals in active employment, 21% were retired, and 17.2% undertook household responsibilities.
Table 2 shows the results for quantitative variables (biochemical data and physical examination).
Table 3 shows the estimated prevalence of CRFs according to age and sex.
Smoking was more common in men (36.9%) than in women (18.7%). In men, 21.7% were nonsmokers (95% CI, 18.9-24.7) and 41.4% were ex smokers (95% CI, 37.9-44.8), while in women, 68.2% were nonsmokers (95% CI, 64.9-71.2) and 13.1% were ex smokers (95% CI, 10.9-15.5).
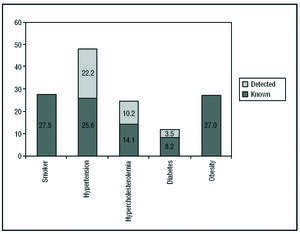
The prevalence of AHT was 47.8%, with large differences according to age in both sexes (Table 3). AHT occurred without the patient's knowledge in 22.7% (Figure 1) and increased with age in men from 8.5% between 35 and 44 years to 16.2% between 65 and 75 years; in women, the increase was from 4.2% in the youngest group to 16.9% in the oldest.
Figure 1. Cardiovascular risk factors: prevalence (%), known or detected for the first time in this study.
The prevalence of hypercholesterolemia in men was 24.4% and in women it was 24.1%; the prevalence of previously unidentified hypercholesterolemia was 10.2% (Figure 1).
The prevalence of diabetes was 11.7%: 8.4% in women and 15.3% in men (Table 3). The prevalence of abnormal baseline glucose levels was 9.5% (95% CI, 8.2-11.1): 11% in men (95% CI, 8.9-13.4) and 8.2% in women (95% CI, 6.4-10.2).
The prevalence of obesity was 27.0%, with marked differences according to age and sex (Table 3). The prevalence of overweight was 40.1% (95% CI, 38.3-43.0): 48.3% in men (95% CI, 44.8-51.8) and 33.4% in women (95% CI, 30.2-36.6).
The prevalence of a sedentary lifestyle was 43.1% in men (95% CI, 39.7-46.5) and 45.6% in women (95% CI, 42.3-49.0). Regular physical activity was undertaken by 22.6% of men (95% CI, 19.8-25.6) and 23.1% of women (95% CI, 20.3-26.0).
In 9.8% of men (95% CI, 7.9-11.8) no risk factors were identified, while in women this figure was 21.8% (95% CI, 19.1-24.7). Two or more risk factors were present in 58.4% of men (95% CI, 55.0-61.8) and 36.8% of women (95% CI, 33.6-40.1).
The prevalence of diagnosed cardiovascular disease was 9.8% (95% CI, 8.3-11.2). That figure included coronary artery disease in 10.5% of men (95% CI, 8.5-12.8) and 3.4% of women (95% CI, 2.3-4.8), cerebrovascular disease in 5% of men (95% CI, 3.6-6.7) and 2.2% of women (95% CI, 1.3-3.4), and peripheral artery disease in 3.6% of men (95% CI, 2.4-5.1) and 1.7% of women (95% CI, 0.9-2.8).
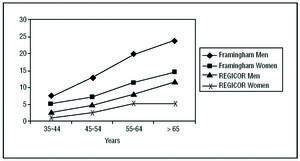
The individual risk of a coronary event in the next 10 years is shown in Figure 2.
Figure 2. Risk of a cardiovascular event at 10 years shown as mean individual percentage for each age and sex group calculated using the Framingham or REGICOR methods.
DISCUSSION
Comparison of the prevalence of CRFs is made difficult by differences in the methods used, the age groups included, standardization of the population, the factors studied, and the limits considered pathological for each factor.
Before discussing the results, it should be pointed out that this study differs from other population-based studies. The study was proposed by scientific societies in the field of primary care. The study population was based on individual health cards, allowing a database to be obtained from within the health-care service itself. Only 1 in 20 patients resident in the Balearic Islands did not have an individual health card, meaning that in terms of CRFs, it can be considered to be a study of the general population. The number of participants obtained was very good, demonstrating the efficiency of patient capture through the primary care system. Most studies increase the number of subjects selected in order to compensate for those who cannot be located, do not respond, or do not agree to participate.10-12
In our study, access to individual health cards meant that we were able to leave substitutes for those who were not eligible or did not respond. Those reserve subjects represented 21.6% of the sample, a percentage that is similar to the 20% classified as not eligible in a study undertaken in Gerona.13
Only 1 in every 4 subjects was contacted when attending a doctor's appointment, suggesting that prevalences have not been overestimated.
More than half of the sample was made up of individuals who were in active employment, a proportion that is similar to that found for these age and sex groups in the Balearic Islands population. There was a slightly lower participation of young people and a slightly higher participation for older men than the reference population (Table 1); however, the estimations of prevalence provided were weighted.
Current trends in smoking habit were confirmed, namely, feminization of the smoking population and increasing numbers of ex smokers.14 Table 4 shows the prevalence of smoking observed in our study, limited to the population aged between 35 and 64 years, along with the prevalence observed in studies of other Spanish populations for the same age groups.10,11,13,15,16 As can be seen in Table 4, our study found a lower prevalence of smokers than the national study, in which there was a lower percentage of ex smokers.10
The temporal trend in prevalence of smoking found in the MONICA study was towards a 5% increase in women and a 5% decrease in men.17 The most similar results in terms of smoking prevalence in men to those found in our study are seen in Castile-La Mancha11 and Alicante,12 and for women, also in Alicante12 (Table 4). Smoking is mainly concentrated in younger subjects. Thus, the prevalence of smoking in the 35 to 45-year age group is 10 times higher than between 65 and 74 years. The proportion of ex smokers was also higher than that found in the national study10 performed 10 years earlier, representing a tendency that is similar to that seen in Southern and Eastern Europe.18
Following Cooper et al,19 an automatic apparatus was used for blood pressure measurements in order to avoid intraobserver and interobserver variation, which can reach 25 mm Hg.20,21
The high prevalence of AHT may be explained by the use of new assessment criteria22,23 and the inclusion of patients receiving antihypertensive treatment. This high prevalence is similar to that of other studies. Thus, in a study of the Spanish population aged between 35 and 64 years, the recalculated prevalence using the new criteria was 45%24; in the Gerona study (population, 25-74 years) it was 39.5%13; in the south of Alicante (population, 20-80 years) it was 50.1%12; and in Castile-La Mancha (population, 25-74 years) it was 41.4%.11 These figures for prevalence differ from those obtained up to the beginning of the 1990s, situated around 20%,10,14,15 if criteria for SAP and DAP are set at above 160 mm Hg and above 95 mm Hg, respectively.
The prevalence increases with age, especially in women, in whom the figure is lower than in men below 65, but becomes higher between 65 and 74 years, as observed in other studies.11,13
Awareness of AHT in our study was similar to that found in Alicante12 but higher than that found nationally.24 Three out of 4 hypertensive patients received treatment, a proportion that is similar to that found in the national study10 but higher than that found in Alicante12 and Gerona.13 Blood pressure was controlled in one third of treated patients, a proportion that is similar to that found in other studies.10,11,13,25
The concentrations of total plasma cholesterol were lower in men than those found in other studies of Spanish populations11,13,26 but similar in women, with the exception of a study performed in Talavera, in which the figures were lower.11 The values for HDL-C were similar to those of the Talavera11 and Gerona13 studies.
The prevalence of cholesterol levels above 250 mg/dL (cutoff point proposed by consensus for analysis of cholesterol levels in Spain27) or treatment with cholesterol-reducing drugs was similar to that found in the Alicante study12 but higher that the national prevalence.10
The estimated prevalence of diabetes is approximate, since the oral glucose tolerance test was not performed. Almost 1 in every 3 cases was previously unidentified or was detected during the study. The results for prevalence of diabetes in other population-based studies that did not use the oral glucose tolerance test are much lower than those obtained in our study.15,10,28 This may be explained by the fact that the cutoff point for glucose concentration used in those studies was 140 mg/dL, whereas our study used the criteria of the American Diabetes Association from 1997 (≥126 mg/dL).29 The prevalence found in our study was closest to that found in the Alicante study,12 in which the same cutoff point was used but which reported a slightly lower degree of previously undiagnosed diabetes. In studies performed in 5 Spanish provinces using the oral glucose tolerance test with pre-1997 criteria29 the prevalence of unrecognized diabetes was 3.5% while the figure for diagnosed diabetes was 4.1%.30
In addition to hyperglycemia as a risk factor, we must also consider abnormal baseline glucose (110-125 mg/dL), which in our study represented 9.5% of the population, since prediabetic stages carry increased risk of cardiovascular events.31,32 Those subjects, along with subjects who have a high HOMA index33 alongside normal glucose levels as an indication of insulin resistance, have a higher cardiovascular risk.
Use of the BMI as an indicator of body fat has been recommended for the adult population between 20 and 69 years.34 Obesity is accepted as corresponding to a BMI ≥30, according to World Health Organization criteria.35 The use of the waist-hip ratio was ruled out, since there is increasing evidence that it is not a good measure of abdominal visceral obesity. Instead, abdominal circumference was used as a good indicator of abdominal fat accumulation, which has also been considered to be a cardiovascular risk factor.36,37
The prevalence of obesity in our study was higher that that seen nationally10 or in the Gerona study,13 and lower than seen in the Alicante study.12 A finding confirmed in all studies is that obesity increases with age.
Those data contrast with data from studies of prevalence performed by the SEEDO group and published in 2000, looking at 8 autonomous communities in Spain, in which a prevalence of 14.5% for the population between 25 and 60 was reported, with a higher prevalence in women (15.7%).34 This marked difference in prevalence may be partly explained by the fact that subjects over 60 years of age were not included, when in our study this corresponded to the age group with the highest prevalence. Our results for the prevalence of overweight were most similar to those from the national10 and SEEDO34 studies.
In our study it is not really possible to talk about sedentary lifestyle since the perception of the subjects was obtained through a questionnaire without confirmation by measurement of calorie expenditure. However, comparison was possible between declaration of exercise undertaken outside of work (which is related to cardiovascular risk38) and the national health survey of 2001,39 since we used the same questionnaire, although not the same age range. In the national health survey, a similar proportion of respondents reported being sedentary in their free time as in our study, representing an additional problem to excess weight (70% of the population) that is added to the fact that only one third of our population reported exercising regularly. This represents a major public health problem that needs to be addressed with combined strategies of promoting healthy eating and healthy lifestyle.40
The prevalence of diagnosed cardiovascular disease, determined by interview and confirmed though the patient's medical history, has not been reported in any other population-based study of Spanish CRFs. Data are available from a primary care study that are similar to those reported here.41 Data from the Gerona study relate to the prevalence of angina and were collected using a specific questionnaire.13
According to our results, 1 in every 10 individuals has known cardiovascular disease. Knowledge of the prevalence of coronary, cerebrovascular, and peripheral vascular diseases allows the volume of patients to be identified for the purposes of secondary prevention.42
Figure 2 shows that individual cardiovascular risk is higher when calculated using the Framingham formula8 than when this formula has been adapted to the Spanish population9; in both cases, the risk increases with age and is higher in men than women.
Finally, in this study we have shown a high prevalence of CRFs in a community with a relatively low incidence of cardiovascular disease and with low mortality rates compared with other industrialized countries,5 a finding that supports the theory of the Southern European paradox.43
ACKNOWLEDGMENTS
We thank Dr. Miquel Fiol, director of the coronary unit of Hospital Son Dureta, Palma de Mallorca, Spain. We are grateful to Dr. Miguel Pocoví, head of the Department of Biochemistry and Molecular Biology at the University of Zaragoza, Spain, and Professor Luis Carlos Silva from the Instituto Superior de Ciencias Médicas, La Habana, Cuba, for revision of the manuscript.
ABBREVIATIONS
CRF: cardiovascular risk factor.
AHT: arterial hypertension.
CI: confidence interval.
BMI: body mass index.
GP: general practitioner.
SAP: systolic arterial pressure.
DAP: diastolic arterial pressure.
HDL-C: high-density lipoprotein cholesterol.
Correspondence: Dr. F. Rigo Carratalá.
Centro de Salud Emili Darder IB-Salut.
Puerto Rico, s/n. 07007 Palma de Mallorca. Baleares. España.
E-mail: frigo@ibsalut.caib.es