Di@bet.es is a national study designed to estimate the prevalence of diabetes mellitus and other cardiovascular risk factors in the Spanish adult population. The prevalence of hypertension and the degree to which it is recognized, treated, and controlled are described.
MethodsThe study included a sample of the Spanish population with 5048 adults aged ≥ 18 years. Patients were questioned and examined, with 3 blood pressure readings while seated and at rest to calculate the mean of the 3 readings. Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg and/or prescription for antihypertensive drug therapy.
ResultsHypertension was found in 42.6% of the Spanish adult population aged ≥ 18 years and was more common among men (49.9%) than women (37.1%). The prevalence was higher among prediabetics (67.9%) and diabetics (79.4%). Undiagnosed hypertension was identified in 37.4% of patients and was more common in men (43.3%) than in women (31.5%). Among patients with known hypertension, 88.3% were receiving drug therapy. Well-controlled blood pressure was found in only 30% and was more common among women (24.9%) than men (16%).
ConclusionsThe prevalence of hypertension in Spain is high, and a considerable percentage of hypertensive patients have still not been diagnosed. Hypertension is associated with diabetes and prediabetes, and although drug therapy is increasingly common, the degree of control has not improved and remains low. Population campaigns should be developed and promoted for hypertension prevention, detection, and treatment.
Keywords
Hypertension (HT) is associated with an increased risk of cardiovascular morbidity and mortality,1,2 and the mortality rate and the risk of cardiovascular events are significantly reduced if blood pressure (BP) is lowered in these patients.3 Consequently, one of the main objectives of health care systems is to identify people with HT and achieve good BP control to prevent complications.
In Spain, the prevalence of HT is high, and it has been reported that the degree of awareness of HT and its control are lower than those observed in other countries in our setting or in the United States,4–6 with medical and financial consequences. Additionally, the degree of BP control has not improved in the last decade.4
In this context, further analysis of the prevalence of HT in Spain and its degree of control is essential to track the changes resulting from better prevention and treatment in recent years.
The Di@bet.es study is a population-based study that covers the entire adult population of Spain, conducted by only 7 well-trained professional teams to determine the current prevalence of cardiovascular risk factors. This study reports on the results regarding prevalence, diagnosis, and degree of HT treatment and control in Spain.
METHODSThe Di@bet.es study is a national cross-sectional, population-based survey carried out between 2009 and 2010.7 A conglomerate-based randomized design was used to select participants and obtain a representative sample of the Spanish population on the basis of data from the registry of the taxpayer-funded Spanish National Health System, which covers more than 99% of the Spanish population. During the first stage, 100 health care centers were selected from throughout Spain, based on a proportional distribution relative to the population of each autonomous community. A total of 100 individuals aged ≥ 18 years were then selected at random from each health care center.
The sample was composed of more than 10 000 adults, of whom 55.8% attended the examination; 9.9% of them were excluded by protocol (institutionalization, serious illness, pregnancy, or recent delivery), leaving a final sample of 5048 individuals aged 18 to 93 years (41.6% men and 58.4% women).
The study was approved by the ethics and clinical research committees in all autonomous communities, and all participants gave informed consent.
Participants were invited to attend a single visit at their health care center, and any participants unable to attend were replaced by the person immediately below on the list. A trained interviewer collected the information directly by a structured questionnaire, and a physical examination was performed. After the interview, a fasting blood sample was taken and an oral glucose tolerance test was performed with 75 g of glucose. Blood samples were centrifuged immediately, and the serum was frozen until the time of analysis. Serum glucose, triglycerides, and cholesterol were measured by enzymatic methods, and high-density lipoprotein cholesterol was determined using a direct method. Low-density lipoprotein cholesterol was calculated by the Friedewald equation.
Information was collected on age, sex, educational level, marital status, job status, and smoking. Educational level was estimated by the highest level completed and divided into 4 groups: no education, primary education, secondary education, and university education. Marital status was classified into 4 categories: married or cohabitating, single, widowed, and divorced. Socioeconomic level was classified as retired, unemployed, student, homemaker, manual worker, or other professionals.
Weight, height, waist, and hip measurements were obtained using standard methods, and the body mass index (BMI) was calculated.
Blood pressure was measured with a validated BP monitor (Hem 703-C, Omron; Barcelona, Spain)8 after several minutes in a seated position. For the analysis, the mean of 3 readings taken 2 min to 3 min apart was used. Participants were considered to have HT if they were taking antihypertensive medication and/or had systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg or to have well-controlled BP if the figures were ≤ 140/90 mmHg (general population) or < 130/80 mmHg (patients with diabetes, nephropathy, or known cardiovascular disease). Patients were considered to be receiving drug therapy if they were on antihypertensive agents, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, renin antagonists, calcium antagonists, alpha-blockers, beta-blockers, or diuretics. Hypertension was assumed to have been previously diagnosed if the patient responded affirmatively to the question: “Have you ever been told by your physician that you have high BP?”
To evaluate regional differences in HT prevalence, the country was divided into 5 areas with equivalent populations: north, central, south, northeast, and eastern coast.
Statistical AnalysisQualitative variables are expressed as a frequency distribution, and quantitative variables are expressed as the mean ± standard deviation. The overall prevalence was standardized by age using the direct standardization method and the 2010 data from the Spanish National Statistics Institute.9
Qualitative variables were compared by the chi-square test, whereas the linear trend in HT prevalence was tested in the case of ordinal qualitative variables by the linear trend test. Both groups were compared by the t test for quantitative variables having a normal distribution.
Logistic regression models were constructed to identify factors independently related to HT and to HT awareness and degree of control. The variables included in the model were: age, BMI, presence of diabetes, educational level, socioeconomic level, marital status, and geographical area. The null hypothesis was rejected in each statistical test at a P value < .05. All data were processed and analyzed by SPSS version 19.0 (IBM Corp.; United States).
RESULTSThe characteristics of the study participants are shown in Table 1, with BMI, waist circumference, systolic BP, and diastolic BP significantly higher in men than in women.
Characteristics of the Study Population, Stratified by Sex
| Men (n=2164) | Women (n=2884) | P | |
|---|---|---|---|
| Age, y | 50.50±17.25 | 50.37±16.79 | NS |
| Age brackets, no. | NS | ||
| 18-30 y | 305 | 368 | |
| 31-45 y | 597 | 849 | |
| 46-60 y | 575 | 813 | |
| 61-75 y | 494 | 605 | |
| > 75 y | 193 | 249 | |
| BMI | 28.52±4.46 | 27.74±5.68 | < .001 |
| Waist circumference, cm | 98.67±11.97 | 90.59±14.71 | < .001 |
| SBP, mmHg | 137.53±18.39 | 127.36±20.52 | < .001 |
| DBP, mmHg | 79.34±10.53 | 75.22±10.20 | < .001 |
| Obesity (BMI ≥ 30), % | 31.7 | 29.8 | NS |
| Diabetes mellitus, % | < .001 | ||
| Known | 11.4 | 9.5 | |
| Unknown | 6.5 | 4.8 | |
| Cardiovascular disease, % | 9.3 | 4.9 | < .001 |
| Stroke, % | 2.8 | 1.6 | < .001 |
| PAD, % | 1.1 | 0.3 | < .05 |
| Known HT, % | 31.3 | 28.6 | |
| Educational level, % | .002 | ||
| No education | 11.8 | 14.0 | |
| Primary education | 35.0 | 37.5 | |
| Secondary education | 37.7 | 33 | |
| University education | 15.6 | 15.5 | |
| Socioeconomic status, % | < .001 | ||
| Student | 3.2 | 2.4 | |
| Retired | 29.7 | 14.9 | |
| Unemployed | 10.8 | 8.3 | |
| Homemaker | 0.2 | 30.7 | |
| Manual worker | 24.2 | 19.4 | |
| Other professionals | 49.4 | 50.6 |
BMI, body mass index; DBP, diastolic blood pressure; HT, hypertension; NS, nonsignificant; PAD, peripheral artery disease; SBP, systolic blood pressure.
Unless otherwise indicated, data are expressed as mean ± standard deviation.
The age-adjusted prevalence of HT was 42.6% (95% confidence interval (CI), 41.2%-44.0%) of the total population, 49.9% (95%CI, 47.8%-52.0%) of men and 37.1% (95%CI, 35.3%-38.9%) of women.
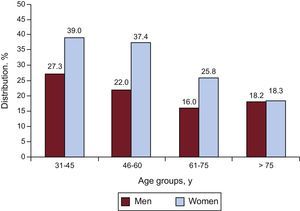
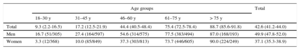
Table 2 lists the prevalence of elevated BP, stratified by sex and age groups. Hypertension increased with age (P < .001 for the tendency) and was more prevalent in men aged up to 75 years, but became just as common among women aged 75 years or older. Also noteworthy was the high prevalence in groups of younger men: more than 15% of men younger than 30 years and 27.3% of men aged 30 to 45 years.
Standardized Prevalence of Hypertension, Stratified by Sex and Age
| Age groups | Total | |||||
|---|---|---|---|---|---|---|
| 18–30 y | 31–45 y | 46–60 y | 61–75 y | > 75 y | ||
| Total | 9.3 (2.2-16.5) | 17.2 (12.5-21.9) | 44.4 (40.5-48.4) | 75.4 (72.5-78.4) | 88.7 (85.6-91.8) | 42.6 (41.2-44.0) |
| Men | 16.7 (51/305) | 27.4 (164/597) | 54.6 (314/575) | 77.5 (383/494) | 87.0 (168/193) | 49.9 (47.8-52.0) |
| Women | 3.3 (12/368) | 10.0 (85/849) | 37.3 (303/813) | 73.7 (446/605) | 90.0 (224/249) | 37.1 (35.3-38.9) |
Data are expressed as percentage (95% confidence interval) or percentage (no./No.).
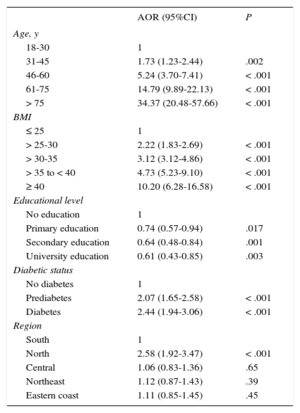
Regarding the influence of other factors (Table 3), HT was more common in patients with higher BMI, lower education level, or impaired glucose tolerance or baseline blood sugar (odds ratio = 2.07; 95%CI, 1.65-2.58) and in diabetics (odds ratio = 2.44; 95%CI, 1.94-3.06).
Probability of Hypertension Adjusted by Age, Body Mass Index, Educational Level, Known Diabetes, Smoking Habit, Occupation, Marital Status, Geographical Area, and History of Cardiovascular Disease
| AOR (95%CI) | P | |
|---|---|---|
| Age, y | ||
| 18-30 | 1 | |
| 31-45 | 1.73 (1.23-2.44) | .002 |
| 46-60 | 5.24 (3.70-7.41) | < .001 |
| 61-75 | 14.79 (9.89-22.13) | < .001 |
| > 75 | 34.37 (20.48-57.66) | < .001 |
| BMI | ||
| ≤ 25 | 1 | |
| > 25-30 | 2.22 (1.83-2.69) | < .001 |
| > 30-35 | 3.12 (3.12-4.86) | < .001 |
| > 35 to < 40 | 4.73 (5.23-9.10) | < .001 |
| ≥ 40 | 10.20 (6.28-16.58) | < .001 |
| Educational level | ||
| No education | 1 | |
| Primary education | 0.74 (0.57-0.94) | .017 |
| Secondary education | 0.64 (0.48-0.84) | .001 |
| University education | 0.61 (0.43-0.85) | .003 |
| Diabetic status | ||
| No diabetes | 1 | |
| Prediabetes | 2.07 (1.65-2.58) | < .001 |
| Diabetes | 2.44 (1.94-3.06) | < .001 |
| Region | ||
| South | 1 | |
| North | 2.58 (1.92-3.47) | < .001 |
| Central | 1.06 (0.83-1.36) | .65 |
| Northeast | 1.12 (0.87-1.43) | .39 |
| Eastern coast | 1.11 (0.85-1.45) | .45 |
95%CI, 95% confidence interval; AOR, adjusted odds ratio; BMI, body mass index.
Hypertension was very significantly associated with glucose tolerance (P < .001). In persons with prediabetes, the prevalence of HT was twice that of the level seen in people with normal glucose tolerance (67.9% compared with 31.6%) and even higher in diabetics (79.4%). In addition, there was an interaction between sex, diabetes, and HT. Whereas HTA was usually less frequent among women, as indicated, these differences in prevalence disappear in prediabetic women (69.0% compared with 70.4% of men; P = .787), and in diabetic women, the prevalence was higher (P < .01) than among men (84.6% compared with 79.8%).
Occupation and marital status had no effect on the prevalence of HT, which was significantly higher in the north than in other areas in Spain.
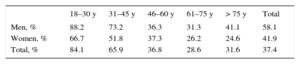
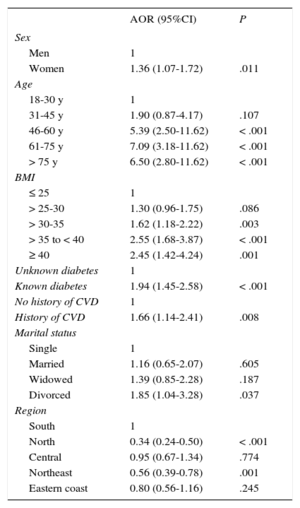
A total of 37.4% of hypertensive patients were unaware of their condition (men, 43.3%; women, 31.5%). When prevalence was analyzed by age group (Table 4), undiagnosed HT was more common in younger individuals, particularly men aged 18 to 30 years (P < .001). Logistic regression analysis showed that women and patients who were elderly, obese, diagnosed with diabetes, or diagnosed with cardiovascular disease were more likely to be aware of their HT (Table 5). Patient awareness of HT also differed between the areas of the country and was significantly lower in the north and northeast than in other areas of the country (P < .001).
Probability of Known Hypertension, Adjusted by Age, Body Mass Index, Educational Level, Known Diabetes, Smoking Habit, Occupation, Marital Status, Geographical Area, and History of Cardiovascular Disease
| AOR (95%CI) | P | |
|---|---|---|
| Sex | ||
| Men | 1 | |
| Women | 1.36 (1.07-1.72) | .011 |
| Age | ||
| 18-30 y | 1 | |
| 31-45 y | 1.90 (0.87-4.17) | .107 |
| 46-60 y | 5.39 (2.50-11.62) | < .001 |
| 61-75 y | 7.09 (3.18-11.62) | < .001 |
| > 75 y | 6.50 (2.80-11.62) | < .001 |
| BMI | ||
| ≤ 25 | 1 | |
| > 25-30 | 1.30 (0.96-1.75) | .086 |
| > 30-35 | 1.62 (1.18-2.22) | .003 |
| > 35 to < 40 | 2.55 (1.68-3.87) | < .001 |
| ≥ 40 | 2.45 (1.42-4.24) | .001 |
| Unknown diabetes | 1 | |
| Known diabetes | 1.94 (1.45-2.58) | < .001 |
| No history of CVD | 1 | |
| History of CVD | 1.66 (1.14-2.41) | .008 |
| Marital status | ||
| Single | 1 | |
| Married | 1.16 (0.65-2.07) | .605 |
| Widowed | 1.39 (0.85-2.28) | .187 |
| Divorced | 1.85 (1.04-3.28) | .037 |
| Region | ||
| South | 1 | |
| North | 0.34 (0.24-0.50) | < .001 |
| Central | 0.95 (0.67-1.34) | .774 |
| Northeast | 0.56 (0.39-0.78) | .001 |
| Eastern coast | 0.80 (0.56-1.16) | .245 |
95%CI, 95% confidence interval; AOR, adjusted odds ratio; BMI, body mass index; CVD, cardiovascular disease.
Most people with previously undetected HT had high isolated systolic HT (66.6%); 22.3% had grade I HT; 7.9% had grade 2 HT, and 2.8% had grade 3.
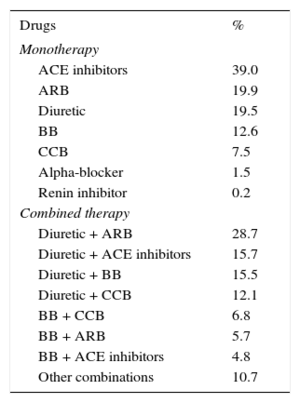
A total of 88.3% of patients with known HT were receiving drug therapy: 55.9% in monotherapy and 44.1% in multiple treatments. The most common drug among patients receiving monotherapy was an ACE inhibitor, followed by angiotensin receptor blockers and diuretics (Table 6). The combinations most commonly used were angiotensin receptor blockers + diuretic (28.7%), ACE inhibitor + diuretic (15.7%), and beta-blocker + diuretic (15.5%). When the entire population (monotherapy and polytherapy) was analyzed, the most frequently used drugs were diuretics (45.4%), followed by angiotensin receptor blockers (36.5%) and ACE inhibitors (34.9%).
Type of Antihypertensive Drug Therapy
| Drugs | % |
|---|---|
| Monotherapy | |
| ACE inhibitors | 39.0 |
| ARB | 19.9 |
| Diuretic | 19.5 |
| BB | 12.6 |
| CCB | 7.5 |
| Alpha-blocker | 1.5 |
| Renin inhibitor | 0.2 |
| Combined therapy | |
| Diuretic + ARB | 28.7 |
| Diuretic + ACE inhibitors | 15.7 |
| Diuretic + BB | 15.5 |
| Diuretic + CCB | 12.1 |
| BB + CCB | 6.8 |
| BB + ARB | 5.7 |
| BB + ACE inhibitors | 4.8 |
| Other combinations | 10.7 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; BB, beta-blockers; CCB, calcium channel blocker.
Hypertension was controlled in 23.9% of all participants and in 26.6% of those receiving medication, with no differences observed between patients receiving 1 drug (28.6%) or more than 1 drug (24.2%). The degree of control was better among women (28.0%) than men (19.0%) in all age groups except patients older than 75 years (Figure).
Only 10.7% of hypertensive diabetics had good BP control, a significantly lower percentage (P < .001) than the rest of the sample (28.7%), even though multitherapy was more common in this patient group (27.5% compared with 22.5%).
However, if the criterion of good control used for diabetics is BP < 140/90 mmHg—as currently recommended—, 27.2% of diabetics would be well controlled, without significant differences compared with control in the rest of the population.
Logistic regression analysis showed that BP control was worse among participants with excess weight or grade 1 obesity, in addition to diabetics. There were also fewer patients with controlled BP in the north of the country than in the other regions (Table 7).
Probability of Controlled Hypertension, Adjusted by Age, Body Mass Index, Educational Level, Known Diabetes, Smoking, Occupation, Marital Status, Geographical Area, and History of Cardiovascular Disease
| AOR (95% CI) | P | |
|---|---|---|
| Sex | ||
| Men | 1 | |
| Women | 1.78 (1.28-2.48) | .001 |
| Age | ||
| 18-30 y | 1 | |
| 31-45 y | 2.25 (0.41-12.38) | NS |
| 46-60 y | 2.65 (0.50-14.01) | NS |
| 61-75 y | 1.90 (0.34-10.36) | NS |
| > 75 y | 1.49 (0.26-8.47) | NS |
| BMI | ||
| ≤ 25 | 1 | |
| > 25-30 | 0.54 (0.34-0.83) | .006 |
| > 30-35 | 0.51 (0.32-0.80) | .004 |
| > 35 to < 40 | 0.67 (0.39-1.14) | NS |
| ≥ 40 | 0.52 (0.26-1.02) | NS |
| Unknown diabetes | 1 | |
| Known diabetes | 0.31 (0.21-0.46) | < .001 |
| No history of CVD | 1 | |
| History of CVD | 0.66 (0.44-1.02) | NS |
| Region | ||
| South | 1 | |
| North | 0.33 (0.17-0.61) | < .001 |
| Central | 1.05 (0.69-1.59) | NS |
| Northeast | 0.71 (0.46-1.11) | NS |
| Eastern coast | 0.77 (0.48-1.23) | NS |
95%CI, 95% confidence interval; AOR, adjusted odds ratio; BMI, body mass index; CVD, cardiovascular disease.
The results of this study provide up-to-date information on HT and on the treatment and control of the condition in the Spanish adult population. Its main strengths are that the sample was representative of all of Spain, that diabetes was diagnosed by an oral glucose tolerance test, and that all data were collected using a small number of well-trained teams according to a rigorous protocol, which ensured their quality. Nevertheless, the study has several limitations: participation was relatively low (56%), and there was greater participation by women and older persons and, therefore, all prevalence data and analysis were corrected for age and sex. Three BP readings were taken at rest at the same visit, although they were not validated with the BP home readings (24-hour ambulatory BP monitoring), which is a possible limitation of the study.
The prevalence of HT in our study was 42.6% (16.5 million people). This figure was significantly higher among men than among women (49.9% compared with 37.1%; P < .001). When participants were stratified by age, the results showed that, as in other population-based studies, the prevalence of HT increased with age and that the lower prevalence observed among women gradually reached the levels seen in men, until becoming equal or higher as of age 70 years.10–13 The prevalence of HT in Spain was similar to that in Portugal,14 but was higher than that among the Spanish adults in the ENRICA (Estudio de Nutrición y Riesgo Cardiovascular en España), study, which provides data on biological cardiovascular risk factors (eg, HT [33%]),10 and that in the United States13 and England.15 These discrepancies are common in the scientific literature, and it is known that the diversity of methodologies and populations among studies may help explain these differences. In our study, the higher prevalence of HT could be explained by an older population, with high rates of obesity and diabetes, as well as by an overestimation of the prevalence by 3 BP readings at health centers compared with the results of the ENRICA study, which took 6 home readings. On the other hand, the use of only 7 pairs of observers for the entire sample may have prevented biases and may have fit reality more closely.
Other factors that affected HT in our study were high BMI, low educational level, and geographical location. The prevalence was higher and the degree of HT awareness was lower in the northern area of the country, but there is no explanation for this and further analyses are required.
The incidence of diabetes in the hypertensive patients in our study was 21%, similar to that in the ENRICA study, whereas obesity and excess weight levels were of great concern in both studies, possibly related to a clearly sedentary lifestyle.
There was a very significant association between HT and changes in glucose metabolism of any grade. The prevalence of HT was not only higher among diabetics, as has been observed worldwide,16 but also among prediabetics, in whom it may be 2-fold the levels seen in persons without impaired glucose metabolism. In addition, it was also observed that, whereas the prevalence of HT was lower among women in the general population, there were no sex-related differences among people with impaired glucose tolerance. In other words, women lose their sex-related advantage when they have abnormal glucose tolerance, whether in prediabetes or diabetes. This finding could be a factor in the increased cardiovascular risk seen in women with impaired carbohydrate metabolism.
This study found that 63.7% of participants were aware that they had HT, a percentage higher than that observed in the ENRICA study (59%)10 or in Portugal (45.7%),17 but lower than that seen in the United States (74%).13 However, more than 6 million people in Spain have undiagnosed HT. We found that 43.3% of men and 31.5% of women with HT were undiagnosed, and undiagnosed HT was particularly noticeable among individuals younger than 45 years. These results are consistent with those reported by other studies10–12,14 and may indicate a lower demand for health care by this segment of the population. In addition, we observed that the percentage of patients already diagnosed with HT was higher among obese and diabetic patients, probably due to more stringent medical follow-up of their condition. Patients were less likely to know about their HT in northern Spain.
More than half the hypertensive patients treated were in monotherapy, a higher percentage than that observed in the studies mentioned, which could also explain the difference in the degree of control. The drug class used most often in monotherapy was ACE inhibitors, differing from that reported by the PRESCAP study,18 which reflects differences in sample selection. The combination most often used was, however, the same as in the PRESCAP study: diuretic + angiotensin receptor blockers (28.7%), followed by diuretic + ACE inhibitor (15.7%).
The degree of control of treated hypertensive patients was 26.6%, noticeably lower than that of ENRICA and slightly lower than the level observed in Portugal (28.6%),14 which is partially explained by the older age of our study population. This degree of control is clearly lower than the level recently observed in Spain by the PRESCAP study,18 but the lack of sample randomization in that study should be taken into consideration. As expected, the degree of control worsened with age and was clearly superior in women than in men.
Among all hypertensive patients, good control was found in only 20.4%, noticeably lower than that reported for other countries, such as the United States.13
Women had better HT control than men, which could be explained by their better response to hypertensive treatment.19 The multivariate analysis also showed that people of normal weight had better control than those with excess weight or obesity, which may be due to the increased sympathetic activity caused by higher BMI.20
In our study, as also reported by PRESCAP, HT control was worse in diabetic patients than in nondiabetics, such that only 10.7% were well controlled according to the existing criteria at the time of the study (BP < 130/80 mmHg). However, if the current criteria were applied (140/90 mmHg), this difference would disappear, which may be due to more intensive therapy in these patients, as it reflects the fact that a higher percentage are receiving multiple drugs.
A meta-analysis on the degree of HT control in Spain,4 which included 76 epidemiologic studies with 341 632 participants observed that 33% of hypertensive patients have well-controlled BP compared with only 12% in the high-risk group. Moreover, the rate of good control in the past decade has barely improved, even though the number of hypertensive patients in monotherapy has dropped significantly and the use of validated automatic units to measure BP is increasingly widespread, which prevents rounding biases in the readings. Our results confirm this lack of improvement apparently seen in previous studies21,22 and reported by PRESCAP. The possible explanations are, first of all, population ageing, as increased age leads to a higher prevalence of systolic HT, with known difficulties with treatment, as well as therapeutic inertia and current socioeconomic difficulties that cause greater difficulty with BP control.23 It is evident from our study that HT is treated to some extent, but is controlled in fewer patients than in the United States or England; nonetheless, our degree of HT control is consistent with the levels reported by other studies conducted in Spain and with the levels generally observed in industrialized nations.5,24
Although a number of meta-analyses and large studies have shown the net cardiovascular benefit of HT control, it is evident that we fall well short of the desired targets, even in settings with clear health standards.25,26
CONCLUSIONSAccording to this population-based study, which is representative of the entire population attended in Spain, a country with a publicly-funded health system covering more than 99% of the population, the prevalence of HT has not decreased and there is a still a high percentage of patients with undiagnosed HT. A strong association was observed between HT and diabetes and between HT and prediabetes, an association that was stronger in women than men, which means that the prevalence of HT among women with diabetes is equal to that of men with diabetes. In addition, although drug therapy is increasingly more common and complex, it does not improve the degree of BP control, which continues to be very low.
It is essential to develop and promote population campaigns for the prevention, detection, and treatment of HT and other cardiovascular risk factors, with particular emphasis on lifestyle habits and targeting the youth population.
FUNDINGCentro de Investigación Biomédica en Red de Diabetes y Enfermedades Metabólicas Asociadas (Instituto de Salud Carlos III-Ministerio de Ciencia e Innovación), Ministerio de Sanidad y Consumo, and Sociedad Española de Diabetes.
CONFLICTS OF INTERESTNone declared.
We would like to thank the following for their assistance: Spanish Society of diabetes, the Federation of Spanish Diabetics, and the Quality Agency of the Health Ministry of Spain. We are deeply appreciative of all family physicians and other health care staff at the participating health facilities, as well as Drs. L. Forga and F. Casanueva for their invaluable assistance in the northern region, all the field workers, nurses, and dieticians (I. Alonso, A. Arocas, R. Badia, C.M. Bixquert, N. Brito, D. Chaves, A. Cobo, L. Esquius, I. Guillén, E. Mañas, A.M. Megido, N. Ojeda, R.M. Suárez, and M.D. Zomeño), without whom this study could not have been done, and to all those who that voluntarily participated in the study.