Keywords
INTRODUCTION
Since cardiovascular risk factors (CVRF) were first identified, the principal goal regarding prevention and treatment strategies has been to describe the prevalence of these factors.1,2 Several different CVRF usually appear together in the same person. At the end of the 1980s, Reaven3 described the metabolic syndrome (MS) as the combination of different clinical features with a common pathophysiological nexus: insulin resistance. Later studies have shown the basic role of CVRF and insulin resistance in the course of atherosclerotic diseases. For instance, ischemic heart disease is known to be the main cause of death and disease in persons who have MS.4
The prevalence of CVRF has been widely studied, especially since the publication of the findings from the Framingham study. However, the prevalence of MS and its impact on cardiovascular diseases, although simple to diagnose,5 has not yet been clearly described. The results of the third National Health and Nutrition Examination Survey (NHANES III) showed an alarming prevalence of the MS of 24%, which rose to 42% among women older than 60 years of age.6 Other cohorts from America7,8 and Europe9,10 have confirmed these findings.
MS has been consistently associated with CVRF and it has received increasing interest since the description of its close correlation with new markers of atherosclerotic disease and endothelial dysfunction, such as C-reactive protein,8 microalbuminuria,11 or vascular thickness and stiffness12; furthermore, the number of components of the MS is associated with the extension of coronary disease and its complications,13 and MS has been proposed as the best integration of the analytical variables in patients who have had an acute myocardial infarction.14 This increasing evidence has led prestigious expert committees from cardiology societies to formulate specific recommendations for the clinical management of patients with MS.15
Although much information exists in Spain about CVRF,16-21 less is available on MS. The high prevalence of insulin resistance and its important predictive value for the development of MS have been demonstrated.22 The prevalence of MS in a community survey was 24%,23 whereas another study reported the prevalence to be 8% among persons without ischemic heart disease and 41% among those who had ischemic heart disease.24 These data, related to both the prevalence of MS and insulin resistance, were corroborated by a recent study.25 Moreover, a new study now shows that the presence of MS increases cardiovascular risk in diabetics.26
These data, however, are probably not fully representative of the population of Spain. The MESYAS (MEtabolic SYndrome in Active Subjects) Registry developed the idea of clarifying the prevalence of MS in a large population sample from Spain. It was decided to include employed persons due to their accessibility via company benefit organizations; and it included an age range with a higher incidence of cardiovascular diseases. Furthermore, it is within this group that the number of potential years of life lost, days off work, or illness have more social and economic relevance. Later stages of the MESYAS Registry, which have already been designed, aim to undertake a prospective evaluation of the incidence of the MS and its specific impact on cardiovascular disease. This report presents the prevalence data for the first workers studied, together with their association with MS and their different jobs performed.
SUBJECTS AND METHOD
Selection and Inclusion and Exclusion Criteria
The description of the prevalence of MS in the MESYAS Registry was planned as a cross-sectional, epidemiological study. The workers were selected from annual medical checkups given during 2003 by the benefit organizations of the 2 separate institutions: el Corte Inglés in Valencia (mostly shop and office workers) and the Ford factory in Almussafes, Valencia (with manual labor workers, supervisors, and managers). The prevalence of the CVRF in the second of these cohorts has already been published.16
Data concerning the annual medical checkups were available for 8169 workers. We excluded 913 workers whose data lacked some of the laboratory measurements required for the diagnosis of MS. The final analysis therefore included 7256 persons (88.8%).
Data Collection and Diagnosis of the Metabolic Syndrome
We designed a uniform database for the collection of data from both benefit organizations. All persons included, as well as the chief representatives of the companies, signed an informed consent document in which they approved the use of their data, with the guarantee of anonymity, and with no chance of being identified by name, worker number or any other such information. The protocol was passed by the ad hoc ethics committee of the Section of Preventive Cardiology of the Spanish Society of Cardiology.
A person was considered to have MS if 3 of the following 5 diagnostic criteria were present (modified ATP-III)5: body mass index (BMI) >28.8; blood pressure (BP) ≥ 130/85 mm Hg; high-density lipoprotein (HDL) cholesterol <40 mg/dL in men or <50 mg/dL in women; triglycerides ≥ 150 mg/dL; baseline fasting blood glucose ≥ 110 mg/dL, or receiving antidiabetic treatment, or the presence of previously diagnosed diabetes mellitus. Abdominal obesity was measured using a BMI≥28.8 instead of the abdominal circumference, a modification that has already been validated in large cohorts.8,9 An oral glucose tolerance test was given to all persons with an altered glucose level (from 110-125 mg/dL) in order to make a correct diagnosis of diabetes.
Blood samples were drawn after a 12 hour fast and processed in the same laboratory. The concentration of low density lipoprotein (LDL) cholesterol was obtained from the Friedewald equation and the non-HDL cholesterol, by calculating the total cholesterol minus the HDL cholesterol. The pulse pressure was obtained by calculating the difference between the systolic BP and the diastolic BP; the mean BP was calculated as one third of the sum of the systolic BP plus double the diastolic BP. Smoking was classified as follows: active smokers, ex smokers (those who had quit smoking more than one year prior to entering the registry), and non-smokers. According to their position, the participants were classified as manual laborers, office or customer service workers, and managers, in accordance with the level of physical exercise and preparation required to perform the job.16
Statistical Study
The data were analyzed using Access 2000 and SPSS 11.0 programs. The quantitative variables are presented as the mean ± standard deviation (SD); all variables were considered normal. Adjustment for prevalence and means was made in a simple population, with an age distribution by decade. The Student t and the χ² tests were used to evaluate the statistical differences between the characteristics of the participants, with the variance analysis of 1 factor to account for the differences among the job categories. The odds ratio (OR) was calculated by a multivariate, logistic regression analysis with the presence of the MS as the dependent variable and age and sex, together with the study variables (job category, obesity, hypertension), as covariables. The specific analyses state which variables were included. Values were considered to be statistically significant if the P was ≤05.
RESULTS
Prevalence of the Metabolic Syndrome
Of the 7256 persons included in the study, 82.4% were men and the mean age was 45.4±8.9 years. Table 1 shows the general characteristics of the participants, as well as the means of the CVRF and the different components of the MS. The men were significantly older than the women.
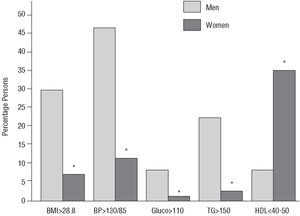
The overall prevalence of MS was 10.2% (743 of the 7256 workers; 95% confidence interval [CI], 9.6%-10.8%); after adjusting for age and sex, the prevalence was 5.8% (95% CI, 4.1%-7.6%), and it was significantly higher in men (8.7%; 95% CI, 7.3%-10.0%) than in women (3.0%; 95% CI, 0.8%-5.1%). The prevalence of the diagnostic criteria was: BP≥130/85 mm Hg in 40% of the workers; BMI≥28.8 in 28.5%; hypertriglyceridemia in 18.3%; low HDL cholesterol in 12.6%; and abnormal blood glucose levels in 7.5%. The workers with the MS were significantly older and more often male; they had higher levels of blood glucose, BMI, systolic BP, diastolic BP, pulse pressure, mean BP, total cholesterol, triglycerides, and non-HDL cholesterol, and lower levels of HDL cholesterol (P<.001 for all the differences). All the components of the MS were significantly more prevalent in the men from our sample, except the criteria for low HDL cholesterol, which was more common in the women (Figure 1). The numbers and percentages of persons who had some of the components of the MS were as follows: 2501 (34.5%) with no component, 2489 (34.3%) with 1 component, 1523 (21%) with 2 components, 589 (8.1%) with 3 components, 140 (1.9%) with 4 components, and just 14 persons (0.2%) with all 5 criteria.
Figure 1. Percentage of persons with at least one of the 5 components of the metabolic syndrome, according to the modified ATP-III criteria.5 *P<.01 men versus women. BMI indicates body mass index; BP, blood pressure (mm Hg); Gluco, baseline glucose (mg/dL); HDL, high-density lipoprotein (mg/dL); TG, triglycerides (mg/dL).
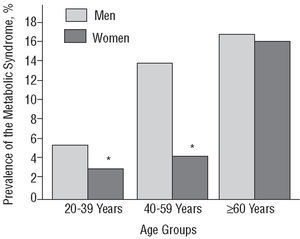
As shown in Figure 2, the prevalence of MS increased in parallel with age. Among persons younger than 60 years of age, MS was more common in the men, with no marked difference in those above this age.
Figure 2. Prevalence of the metabolic syndrome according to age and sex. *P<.01 men versus women.
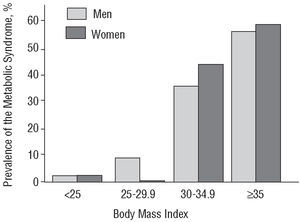
After stratifying for BMI (Figure 3), the prevalence of MS increased markedly in persons with a BMI>30 (35% in men and 42.8% in women) or a BMI≥35 (43% in men and 57.2% in women). The women with a BMI≥35 had the greatest prevalence of the whole cohort (57.2%). Most persons in the study were normoglycemic, with only 3.5% having altered blood glucose levels and 4.2% diabetes mellitus. The greatest prevalence of MS was seen in the workers with diabetes (58.4%), followed by those with abnormal blood glucose levels (50.4%). The workers with normal blood glucose levels had a low prevalence of the MS (6.5%).
Figure 3. Prevalence of the metabolic syndrome according to the body mass index. P>.05 for all comparisons.
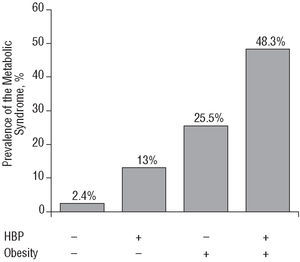
In order to study the effect of high blood pressure, obesity, and diabetes on the presence of MS we undertook a multivariate, logistic regression analysis, adjusted for age and sex. The men had a higher tendency to have the MS (OR=3.2; 95% CI, 2.2-4.7) on the base model (age and sex). The independent incorporation to the base model of the different factors showed that, after adjusting for age and sex, the presence of high blood pressure (BP>140/90 mm Hg) conferred a high risk for the MS (OR=4.4; 95% CI, 3.85.2), although lower than the risk conferred by obesity (BMI>30) (OR=9.9; 95% CI, 8.4-11.8), with both these factors being lower than the risk conferred by diabetes (baseline blood glucose >126 mg/dL) (OR=11.1; 95% CI, 8.6-14.5). Figure 4 shows the increase in the prevalence of MS depending on the presence of obesity and high blood pressure. Table 2 gives the independent OR for each factor after considering the independent influence of each of these factors in a joint model adjusted for age as a continuous variable.
Figure 4. Prevalence of the metabolic syndrome according to the presence of high blood pressure and obesity. HBP indicates high blood pressure; +, presence; , absence.
Job Category and the Metabolic Syndrome
Table 3 shows the overall characteristics of all the participants, classified according to the three job categories. The manual laborers, who represented two thirds of the total, were mainly men, were older, had a higher BMI, systolic BP, diastolic BP, and triglyceride concentrations, and were more often smokers. The office workers were the youngest, with both sexes equally represented, and had the highest HDL cholesterol, and lowest total cholesterol and non-HDL cholesterol levels of all the participants. The managers, who were also older and mainly men, were the group with the highest blood glucose, total cholesterol, and LDL cholesterol levels, whereas they were the group that smoked least.
The crude prevalence of MS was 12.5% in the manual laborers, 7% in the managers, and 5.7% in the office workers. However, the age differences and sex proportion warranted adjustment of the prevalences and means. According to job category, the adjusted results were only calculated for the men ages 30-60 years, due to the low number of women and persons with ages above or below these limits in some categories. The prevalence of MS in men in the 30-60 year age range was 11.3 (95% CI, 9.8-12.7). The adjusted prevalences in each job category were as follows: manual laborers, 11.8 (95% CI, 10.2-13.4); office workers, 9.3 (95% CI, 6.1-12.5), and managers, 7.7 (95% CI, 2.6-12.8). Despite the variation in the prevalence, the differences were not statistically significant because the 95% CI overlapped. The multivariate, logistic regression analysis of the influence of job category on the presence of MS, adjusted for age and sex, and considering an incremental influence (managers, office workers, and manual laborers), only showed significant differences in the last increment, probably owing to the low number of managers in the sample. We therefore calculated the influence considering the managers and office workers jointly, which showed that the fact of belonging to the category of manual laborer increased the likelihood of having MS (OR=1.3; 95% CI, 1.1-1.6) as compared with the other 2 job categories. Individual inclusion of the BMI, BP, or HDL cholesterol in the model failed to make the significance disappear, which did occur when the triglycerides were included, thus suggesting that the greater prevalence in the manual laborers depended on the differences in these concentrations.
Other Risk Factors and the Metabolic Syndrome
Over 50% of the sample was composed of active smokers. The prevalence of smoking was similar in the persons with and without MS. However, the workers with MS were more commonly ex smokers (30% vs 20%; P<.001). Although a similar percentage of men and women smoked, more men were ex smokers (24% vs 5%; P<.001).
Most of the participants were normoglycemic, with only 3.5% having an altered blood glucose level and 4.2% diabetes mellitus. Concerning this classification, the greatest prevalence of MS was found in workers with diabetes (58.4%), followed by those with abnormal blood glucose level (50.4%). The workers with normal blood glucose levels had a low prevalence of MS (6.5%). The multivariate analysis, adjusted for age, sex, and BP, showed that the risk for MS conferred by the presence of abnormal blood glucose levels was very high (OR=8.4; 95% CI, 6.6-11.0), although lower than that conferred by diabetes mellitus (OR=10.2; 95% CI, 7.8-13.4).
DISCUSSION
Prevalence of the Metabolic Syndrome
The MESYAS Registry describes the prevalence of MS in a large group of Spanish people. The results show that 1 in 10 active workers had the MS. Moreover, the prevalence of MS increased to 45% in certain subgroups of workers, despite the fact that the overall sample had low cardiovascular risk (with almost 70% of the subjects having none or only one component of the MS) as active workers who were supposedly healthy.
The most prevalent components of the MS in our study population were high blood pressure (44.4%) and a BMI>28.8 (25.5%), followed by hypertriglyceridemia (18.3%), low HDL cholesterol (13.6%) and altered blood glucose level (7.5%). Among the workers with MS, the most prevalent component was a BP>130/85 mm Hg (94.5%), although only 61.6% were truly hypertensive (BP>140/90 mm Hg) . These results coincide with the findings of the WOSCOPS study, in which 95% of the participants who had MS fulfilled the criterion for high BP.9 The finding of a small, but significant, difference in pulse pressure coincides with recent findings showing that the MS is accompanied by increased intima-media thickness and vascular stiffness.12
The prevalence of MS increased in parallel with increasing age and BMI, which agrees with all the large studies published to date.6-9 The men had a significantly higher prevalence of MS in the age groups <60 years of age, though the difference disappeared above this age. This fact has not been previously reported and it agrees with the clinical experience that men have cardiovascular complications at earlier ages than women, who have these complications some 10 years later, or after menopause.
The increase in the number of overweight and obese persons in western countries and their association with cardiovascular diseases has led to the determination that these disorders are an important public health care problem of epidemic proportion27; the situation in Spain may well be similar if we consider the prevalence of overweight and obese persons in some series that were not specifically evaluating this fact.16-18 The results of Ascaso et al22 show the important predictive factor of abdominal obesity in the appearance of insulin resistance and MS. In our study we evaluated obesity from the BMI and saw that its presence considerably increased the prevalence of MS. Increased physical exercise, a balanced diet, and weight loss are the basic measures for the management of most CVRF, especially for MS.28,29 The WOSCOPS study demonstrated the important predictive power of the MS in the onset of new cases of diabetes.9 Adequate description and diagnosis of the MS thus assume more importance from a predictive viewpoint. Furthermore, the place of origin of our sample should also be considered. According to some of the most recent results from the IBERICA Study,30 the autonomous community of Valencia is one of the areas with the highest rates of death and disease associated with acute myocardial infarction. These data are not at all promising and heighten interest in describing new risk factors and alternative preventive measures.
Assessment of the more atherogenic lipoproteins by calculating the non-HDL cholesterol has been shown to be highly predictive for cardiovascular death, even superior to valuation of the concentration of LDL cholesterol.31 The workers with MS had far higher levels of non-HDL cholesterol, with the difference being much greater than that of other lipoproteins, such as LDL cholesterol or HDL cholesterol. Concentrations of apolipoprotein B have recently been shown to be associated with markers of insulin resistance and presence of MS.32 The purpose of the MESYAS Registry is to describe the prevalence of MS and study the distribution of its components in a large sample of Spanish subjects, in an attempt to provide simple tools to identify this disorder. We believe that the calculation of non-HDL cholesterol is simple and will prove a useful enhancement to the daily systematic measurements for the evaluation of cardiovascular risk.
Other Risk Factors and the Metabolic Syndrome
The findings relating to the association between smoking and the prevalence of the MS are highly relevant. Furthermore, this is the first registry in Spain to study this association. The workers with MS were more often ex smokers. This may be because the higher number of associated classic CVRF may have stimulated more energetic measures to quit smoking. In the Whitehall II Study,33 the likelihood of having MS was slightly increased in ex smokers. Alternatively, as MS was significantly associated with being a smoker or an ex smoker, never having smoked may be considered protective against the MS, if the other risk factors are discounted.
Although the prevalence of altered fasting glucose or an alteration in carbohydrate metabolism was less than in other studies,8-11,17 our data nevertheless clearly show that having baseline glucose >110 mg/dL was associated with a series of clinical conditions that increased the prevalence of MS to 50%. In those workers who were diabetic, the mean BP was 137.1/85.6 mm Hg and the mean triglyceride concentration was 165 mg/dL.
Another very interesting finding was the difference in the levels of pulse pressure and mean BP. The capacity of MS to enhance the harmful effects of age on the vessel wall has recently been demonstrated, and this might partly explain the greater pressure differential seen in our sample.12 The prognostic value of the pulse pressure and the onset and course of cardiovascular diseases has been clearly shown34 and this could be one more of the multiple causes of ischemic heart disease associated with MS. Additionally, the great difference found in the mean BP values in persons with MS as compared to those without MS is also of relevance, given the strong, independent association between mean BP and stroke.35 These findings are in agreement with a recent subanalysis of the NHANES III, which showed the high prevalence of stroke in association with MS.36
Job Category and the Metabolic Syndrome
As far as we are aware, this is the first study to include an analysis of the various characteristics of the MS in different job categories. A study of Japanese factory workers found a higher overall prevalence of the MS than in our study (17.3% vs 10.2%).37 The geographic, social, and cultural differences between the 2 studies are obvious. The fact that our study was undertaken in 2 companies with very different kinds of employees added heterogeneity to our sample. Furthermore, unlike the Japanese study, our study included workers with very different jobs, including assembly line workers, office workers, and supervisors or managers. Contrary to common belief, the manual laborers had a greater BMI, probably due to the stationary tasks, such as those of an assembly line, as a result of the incorporation of machinery to replace previous tasks involving intense physical activity. The office workers, on the other hand, had a lower cardiovascular risk profile (lower values of BMI, BP, LDL cholesterol, non-HDL cholesterol, and triglycerides). The fact that they were more often women and that they were younger resulted in the standardized prevalence of MS being greater than in the managers, despite the fact that they had a less favorable crude lipid profile.
Finally, it is interesting to note that the managers had the highest mean levels of baseline glucose, total cholesterol, and LDL cholesterol, in spite of having a mean BMI of 25.7. The age-adjusted prevalence of MS in men showed an inverse social gradient, although these differences were not statistically significant. Nevertheless, the logistic regression analysis showed that the influence was significant. Given the small number of managers in the sample, it cannot be confirmed whether or not there are differences between them and the office workers, however the manual laborers clearly had a greater prevalence of MS. We believe that these findings reflect lifestyle and dietary habits, especially if we consider that the triglyceride concentrations were the component of the MS that best explained these differences in prevalence. Indeed, the results of the Whitehall II Study33 suggested that the MS might reflect social differences according to the level of education. In the Whitehall II Study, the figures for total cholesterol and LDL cholesterol were not associated with the level of education, though this was associated with HDL cholesterol and triglycerides, as was in our study. We noted that the association between social level and MS seemed to depend on the differences between the groups in the levels of triglycerides especially, and to a lesser extent, HDL cholesterol. The close association between overweight, BP, and glucose levels was also seen in our study.
Limitations
The main limitation of our registry is that it is a cross-sectional study with active workers, and thus it can describe associations but not causes. Furthermore, the results should be considered representative of a particular group of workers. The MESYAS Registry does not describe the profile of patients selected from health care centers or hospitals, but rather that of persons free from limiting disease. Further studies including persons of different ages, a greater proportion of women, and other working conditions could provide different results. For obvious reasons, the number of persons in the sample who were older than 60 years of age was limited. The use of BMI rather than abdominal circumference is a widely accepted modification,6,8,9 although this modification is known to have a tendency to underestimate the prevalence of MS. Furthermore, this criterion was elaborated in study cohorts including persons from Northe for Spanish people. It should be kept in mind that our results are limited to the risk conferred by obesity, as evaluated from the BMI, of having MS and not the risk conferred by abdominal obesity, as evaluated by the abdominal circumference. Moreover, the use of a single sample to measure the baseline glucose level may reduce the diagnostic rigor, though the large sample size would tend to attenuate this. No record was made of menopause, although 92.1% of the women were ≤50 years old. To date, collection of specific data concerning dietary habits has not been possible.
CONCLUSIONS
One in 10 active workers had MS. Although this prevalence may seem low in comparison to other series, it rose to 40% in certain groups of workers. The prevalence of MS increased with age, BMI, BP, and baseline fasting glucose. All the components of the MS were more common in the men, except for a low HDL cholesterol, which was more frequent in the women. High blood pressure (OR=3.4), obesity (OR=9.6), and diabetes (OR=15.4) were independently associated with a greater prevalence of MS. Being a manual laborer conferred a higher risk for MS, independently of age or sex (OR=1.3). This effect seems to depend on less favorable triglyceride concentrations.
ACKNOWLEDGEMENTS
The authors are grateful to the following for their collaboration: the medical service of the Corte Inglés, Valencia: Luis Francisco Camisa Jiménez, Eva María Costa Morant, Eugenia del Mar García-Vilanova Comas, and Joaquín Antoni Martínez.
The medical service of Ford, Spain: Francisco Orts Suárez, Francisco Iñiguez Albort, José Cruz Gisbert, Manuel Puchades Buendía, Concepción Benaches Cárcel, Agustín Baldovi Vercher, Jorge Grau Carmen, and Jorge Sanchís Botella.
MEMBERS OF THE MESYAS RESEARCH TEAM
Eduardo Alegría, Ignacio Ferreira, José Antonio Casasnovas, Alfonso del Río, Alberto Cordero, Martín Laclaustra, Alberto Grima, Emilio Luengo, Montserrat León, Mónica Nájar, Beatriz Ordóñez, and Clara Bergua.
The MESYAS Registry has a grant from the Spanish Society of Cardiology (Seville, 2003) and the Section of Preventive Cardiology and Rehabilitation.
Correspondence: Dr. E. Alegría Ezquerra.
Departamento de Cardiología. Clínica Universitaria de Navarra.
Avda. Pío XII, 36. 31008 Pamplona. Navarra. España.
E-mail: ealegria@unav.es