Keywords
INTRODUCTION
The bundle branch block (BBB) concept was introduced more than a century ago by Eppinger et al.1 Since then it has generated considerable interest in the medical literature, and is now a familiar finding for all physicians involved in clinical practice. Nonetheless, despite the extensive available literature, which agrees on the association of BBB with advanced age, there are considerable discrepancies regarding the prevalence of BBB and its association with other heart diseases and cardiovascular risk factors. The relationship between BBB and hypertension, coronary disease, and heart failure has been the subject of numerous research efforts and the source of conflicting results in major epidemiologic studies.2-7
Although there is agreement on the importance of BBB as an indicator of a poor prognosis in patients with myocardial infarction, whether treated with thrombolysis or not,8-10 and in chronic coronary disease, regardless of the degree of systolic dysfunction or extent of the coronary lesions,11 the role of BBB itself as a predictor of cardiovascular mortality or morbidity is not well established.
More than 30 years ago an association was observed between cardiovascular disease and chronic kidney disease,12 and now this is a fully recognized fact.13 Nevertheless, some specific aspects of cardiovascular disease occurring in dialysis patients have not been fully investigated. Conditions such as atrial fibrillation and peripheral arterial disease, which are quite important in the general population, have received little attention in this group of patients.14-17 To our knowledge, there are no published studies analyzing the relationship between chronic kidney disease under dialysis treatment and intraventricular conduction defects.
The aim of this study is to establish the prevalence of complete BBB in patients starting dialysis and to analyze the factors associated with BBB or that predispose to its appearance. In addition, the associations between BBB and mortality and the development of cardiovascular events are investigated.
METHODS
All patients starting hemodialysis or peritoneal dialysis for the first time at our hospital or affiliated outlying centers between November 1, 2003 and December 31, 2006 were included in the study.
During the first month under treatment, a cardiologist assessed all patients by performing a clinical history, physical examination, electrocardiography, and color Doppler echocardiography. Complete BBB was established when the following criteria were present on electrocardiography:
- Left bundle branch block (LBBB): a) QRS duration ≥120 ms; b) QS or rS complex in lead V1; c) slurred R wave in leads I, aVL, V5, or V6, or rS pattern in V5, or V6; and d) absence of Q wave in leads V5,V6, or I
- Right bundle branch block (RBBB): a) QRS duration ≥120 ms; b) R or rSR' pattern in leads V1 or V2; and c) slurred S wave in leads I, V5, or V6. In RBBB, the QRS axis in the frontal plane was taken into account, such that an axis of less than -30° was considered attributable to a left anterior hemiblock (LAHB) and indicative of bifascicular block
An analysis was performed to determine the relationship between the conduction defect and the following factors: age, sex, diabetes, hypertension, pulse pressure, smoking, body mass index, history of coronary disease, stroke, and atrial fibrillation, analytical values for troponin I, hemoglobin, urea, creatinine, albumin, cholesterol, triglycerides, calcium, phosphorus, and parathyroid hormone, as well as the size of the left atrium and ascending aorta, left ventricular hypertrophy, ejection fraction, E/A ratio for mitral flow, and annular or valvular calcifications. Hematological and biochemical parameters were determined at the start of treatment.
Patients were considered to have hypertension when their blood pressure value at the time of enrollment was >140/90 mm Hg or they were under drug therapy to control blood pressure. Patients were considered to have diabetes when they were taking antidiabetic drug treatment, and were classified as smokers if they were actively smoking at the time of enrollment or had stopped smoking within the 3 months prior to enrollment. A history of coronary disease was established when the patient had experienced a myocardial infarction or showed significant obstructive lesions on coronary angiography. Color Doppler echocardiography studies were performed by the same operator. Left atrial and ascending aorta dimensions were determined using a long-axis parasternal view. Left ventricular ejection fraction was calculated in M mode applying the Teichholz formula, and left ventricular mass was estimated following the Penn convention method.
Patients were followed-up until November 30, 2007 except when there was a change of residence that implied continuing dialysis treatment at another center, death, or transplantation. We analyzed the relationship between BBB and overall mortality and the development of cardiovascular events, defined as coronary disease (acute myocardial infarction or coronary angiography showing >70% lesions in epicardial coronary arteries), stroke, or pacemaker requirement. All patients were in a dialysis program and in permanent contact with the hospital; hence, collection of data related to their evolution did not pose any problems.
Statistical Analysis
Univariate analysis (Student t test for quantitative variables and Fisher's exact test for qualitative variables) was used to examine whether there were differences between patients with and without BBB for candidate variables that would be predisposing factors to this condition. Logistic regression models were developed to measure the association between the predisposing factors and BBB. The models estimated the odds ratio (OR) and 95% confidence interval (CI). A P value of <.05 was considered statistically significant in the hypothesis testing.
RESULTS
The study included 211 patients. The clinical characteristics and echocardiographic parameters of the study population are presented in Tables 1 and 2. Twelve (5.6%) patients had ejection fraction values of <50%. Left ventricular mass was >120 g/m2 in 93.3% (111/119) of men and >100 g/m2 in 94.6% (87/92) of women.
Among the 211 patients, 24 (11.4%) presented complete BBB, including 6 (2.8%) LBBB and 18 (9%) RBBB. Among the latter, 7 patients (38% of all RBBB and 3.3% of the total number of patients) presented RBBB plus LAHB (bifascicular block).
None of the patients with BBB had EF <50%. Left ventricular mass was >120 g/m2 in men with BBB and >100 g/m2 in women with BBB.
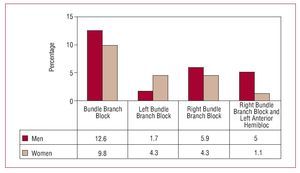
The differences in the presentation of BBB between men and women are shown in Figure 1. BBB was more common in men than in women (15/119 [12.6%] and 9/92 [9.8%], respectively), although the difference did not attain significance. Among men, RBBB were predominant, accounting for 86.6% of the BBB detected (13/15). The percentage was more balanced among women, with LBBB detected in 4 of the 9 patients with BBB (44.4%).
Figure 1. Distribution of bundle branch blocks by site and sex. Values are expressed as percentages of the total population of men and women.
The variables showing the most significant differences between patients presenting conduction defects and those that did not are presented in Table 3. Older age, elevated body mass index, diabetes, increased pulse pressure, and calcifications were significantly related to the presence of BBB. A history of hypertension was documented in 92% of patients with BBB and 89% of those without.
The associations between BBB and all the variables in Table 3 are shown in Table 4. As can be observed, older age and higher body mass index are independently associated with a higher probability of developing BBB.
There was a higher percentage of diabetic subjects among the patients with bifascicular block than among those with RBBB or LBBB alone. Patients with LBBB had a lower ejection fraction and higher frequency of documented coronary disease and atrial fibrillation than those who had RBBB or bifascicular block. Differences according to the location of the conduction defect are shown in Table 5.
Patients were followed up for a mean (SD) of 23.7 (12.9) months. Over the follow-up period, 67 (31.7%) patients died, 15 (7.1%) underwent transplantation, and 5 (2.4%) moved to a residence outside the catchment area of our institution. In addition, 25 (11.8%) had a cardiovascular event during follow-up, which consisted of pacemaker implantation in only 2 cases. Mortality was higher in the group of patients with BBB (54.2% vs 28.9%). Five of the 6 patients with LBBB (83.3%), and 8 of the 18 patients with RBBB (44%) died during follow-up. In addition, cardiovascular events occurred in a higher proportion of patients with BBB than in those with no conduction defect (16.6% vs 11.2%). As was seen for mortality, LBBB was more closely related to development of a cardiovascular event, which occurred in 16.7% of patients with LBBB and 11.1% of those with RBBB. Because of the limited number of patients included, however, the differences were not statistically significant. One of the 2 patients who required pacemaker implantation had a bifascicular block.
DISCUSSION
As this study shows, complete BBB is highly prevalent among patients starting dialysis. Our results cannot be compared with similar studies because there are no published reports analyzing this aspect of cardiovascular disease in the population of dialysis patients. Nonetheless, were able to carry out some estimates regarding the differences with respect to the general population. Our findings concur with epidemiological studies showing that BBB is associated with older age. In the Framingham study,2 the finding of a QRS complex >0.12 s was exceptional in individuals under 50 years, but reached a prevalence of almost 11% in men in the 8th or 9th decade of life. In a study of men in Sweden,3 the prevalence of BBB was 1.2% at age 50, 12.2% at 75, and 17% at 80.In the present study, age was independently related with BBB; only 1 (2.4%) of the 41 patients under 51 had the conduction defect, whereas BBB was documented in 19.4% of patients over 75. The relationship between BBB and age in our study group was similar to the trend seen in the general population. However, same cannot be said for the prevalence. In our analysis, the prevalence of BBB among men 370 years old was 19.2% and among women, 14.3%. These figures are much higher than those of the general population. In the Framingham study,2 the prevalence of BBB in a population of similar age was 11% in men and 5% in women. In the Swedish study, which only included men, the prevalence was 12.2% at age 75 and 17% at age 80.3 The Reikiavik4,5 study reported that 4.1% of men and 1.6% of women aged 75 to 79 years presented BBB. The higher prevalence of conduction defects among men in our study is also similar to the general population,2,4,5 although the differences between sexes occurring in our population were smaller.
The higher prevalence of BBB we found can be attributed to the fact that almost all the patients included had a current or prior history of hypertension. Nonetheless, the relationship between hypertension and intraventricular conduction defects has been, and continues to be, a subject of controversy. In contrast to the Framingham2 study, the one performed in Iceland found no association between hypertension and LBBB,5 but did establish a link between hypertension and RBBB in men and women under 60 with this condition.4 Data from studies by Eriksson et al3 and Ostander6 have also shown a lack of significant relationships between conduction defects and hypertension, whereas other authors have reported an association only in bifascicular block.7 Therefore, we believe that attributing the higher prevalence of BBB found in our study only to hypertension is not supported by a high enough level of evidence. In addition, this higher prevalence is similar to that found in other clinical manifestations of cardiovascular disease in patients with chronic end-stage renal disease.16-18 The higher proportion ofRBBB than LBBB is an almost constant finding in the general population,2-5 although there is no overall agreement on this point either.19
We do not have an explanation for the relationship between BBB and high body mass index seen in our patients, which has not been described previously. Nor have we found descriptions of the association between BBB and pulse pressure documented in our patients. There has been some mention,4,5 although it is not constant,3 of the association we found between conduction defects and diabetes.
The relationship between valvular calcifications and conduction disorders was reported many years ago20,21 and the association between valvular calcifications and chronic kidney disease is well established.22-24 Thus, the association we found between conduction defects and annular or valvular calcifications is not surprising, and, in fact, has been indicated in a previous study.25
As was the case of hypertension, left ventricular hypertrophy was present in a quite significant percentage of our cohort, a fact that makes it difficult to establish differences for this parameter in patients with and without conduction disorders.
When the factors associated with BBB were analyzed in relation to the location of the conduction defect, we found that LBBB was associated with a higher incidence of coronary disease, atrial fibrillation, and valvular calcifications, although the limited patient sample makes it difficult to establish statistical significance.
As is true for the BBB-related factors, the influence of conduction defects on the clinical evolution of the patient remains poorly delimited. The recent Swedish study26 showed that the presence of RBBB in 50-year-old men without myocardial infarction or stroke increased the risk of developing a high-grade atrioventricular block, but did not change the estimated life expectancy or development of cardiovascular events. However, LBBB was associated with both atrioventricular block and a higher risk of death due to ischemic causes. The Framingham27 study concluded that LBBB is more closely associated than RBBB with the development of cardiovascular disease in men, whereas in women, both conduction defect sites showed a similar clinical correlation. In the analysis to determine the significance of isolated BBB, that is, in the absence of heart disease or cardiovascular risk factors, LBBB had a poorer prognosis than RBBB.28,29
The duration of follow-up in our study was shorter than that of the studies performed in the general population mentioned above. This short follow-up and the small number of patients included are the main limitations of the study. It should be kept in mind, however, that the population under study (patients initiating dialysis) is a relatively small group with a much higher mortality rate than that of the age-matched general population. The present study includes all patients starting dialysis in the catchment area of our center (650 000 inhabitants) over a period of 3 years, who had a yearly mortality rate of approximately 15%. Taking into account these limitations, our study showed a poorer prognosis in patients presenting BBB at the start of dialysis, which was more pronounced in those with LBBB.
CONCLUSIONS
In summary, patients starting dialysis present a high prevalence of BBB as compared to similar age groups in the general population. This high prevalence can probably be attributed to several factors, as has been reported for other clinical manifestations of cardiovascular disease.29,30 Among these related factors, we should highlight those that have shown a relationship with interventricular conduction defects in the general population and that are present in a high percentage of these patients, such as hypertension, left ventricular hypertrophy, and calcifications. The presence of BBB in a patient starting dialysis should be considered a factor indicative of a poor prognosis, particularly when the conduction defect is an LBBB.
ABBREVIATIONS
BBB: bundle branch block
LAHB: left anterior hemiblock
LBBB: left bundle branch block
RBBB: right bundle branch block
Correspondence:
Dr. E Vázquez Ruiz de Castroviejo. Navas de Tolosa, 4 y 6, P-1, 6.o D. 23003 Jaén. España.
E-mail: vazquez89@arrakis.es
Received December 31, 2007.
Accepted for publication March 13, 2008.