To analyze changes in healthcare delivery and results for primary angioplasty at Centro Hospitalario Universitario A Coruña following implementation of the PROGALIAM protocol.
MethodsObservational registry of 1434 patients referred for primary angioplasty between 2003 and 2007. Results under PROGALIAM (May 2005 – December 2007; n=963) were compared with those from the preceding period (January 2003 – April 2005; n=388).
ResultsAfter implementing PROGALIAM, there were increases in the number of primary angioplasty procedures (preceding period, 14.4 cases/month; PROGALIAM, 32.2 cases/month), mean patient age (preceding period, 61.3 (11.9) years; PROGALIAM, 64.2 (11.7) years; P<.001), and the percentage of patients referred from peripheral hospitals and treated after normal working hours. Overall median first medical contact-to-balloon time increased (previous period, 106min; PROGALIAM, 113min; P=.02), but decreased significantly among patients referred from noninterventional centers (previous period, 171min; PROGALIAM, 146min; P<.001). Percentage of cases with an first medical contact-to-balloon time <120min remained unchanged among interventional-center patients (preceding period, 69%; PROGALIAM, 71%; P=.56) and increased among patients at noninterventional centers, although it remained low in this subgroup (preceding period, 17%; PROGALIAM, 30%; P=.04). Thirty-day mortality (preceding period, 5.2%; PROGALIAM, 6.2%; P=.85) and 1-year mortality (preceding period, 9.5%; PROGALIAM, 10.2%; P=.96) remained unchanged.
ConclusionsImplementation of PROGALIAM allowed us to increase the percentage of patients receiving primary angioplasty without jeopardizing the clinical results of this treatment.
Keywords
.
IntroductionPrimary angioplasty (PA) is the treatment of choice in acute ST-elevation myocardial infarction (STEMI)1 as it has been shown to decrease mortality compared to fibrinolysis.2 Recently, a number of health care networks have been set up with a view to providing PA to a larger percentage of patients.3 One such example is the Programa Gallego de Atención al Infarto Agudo de Miocardio or PROGALIAM4 (Galician Program for Acute Myocardial Infarction Care).
The aim of this study is to describe and compare care and results from the PA network in the Northern Galicia Area before and after implementing PROGALIAM.
Methods Study ContextThe Hemodynamics Unit at Complejo Hospitalario Universitario A Coruña (CHUAC, A Coruña University Hospital) provides permanent PA service for Northern Galicia Area, an area with a population of 1 million and 4 noninterventional hospitals (Figure 1). Since May 2005, this activity has taken place within PROGALIAM,4 a publicly funded initiative of the Servicio Gallego de Salud (Galician Health Service) that aims to extend PA coverage to all patients in Galicia. In order to achieve its objectives, the program optimized the efficiency of its existing health resources by organizing an integrated hub and spoke network instead of increasing the resources dedicated to patients with acute myocardial infarction. The PROGALIAM protocol also includes the activity of the other two Galician hospitals offering PA (Central and Southern Areas); those results are not presented in this article.
Figure 1. Regional primary angioplasty network for the Northern Galicia Area. The white frames show the distances and estimated transport times between peripheral hospitals and the interventional hospital. Ambulance-shaped icons show the bases for the four Emergency Medical Service, “dial 061” mobile intensive care units available in the area. CHUAC, Complejo Hospitalario Universitario A Coruña.
Study DescriptionA prospective record was kept of all patients referred to CHUAC for PA between January 2003 and December 2007. An electronic form with demographic, clinical, and care information was completed for each patient. Vital status information was drawn from the SERGAS mortality register. The PROGALIAM results (May 2005 to December 2007) were compared to those gathered during the previous period (January 2003 to April 2005).
Changes in Care Under PROGALIAMLaunching PROGALIAM entailed implementing several changes in the STEMI care protocol used in our area (Table 1).
Table 1. Care Modifications to the Primary Angioplasty Protocol for the Northern Galicia Area Following Implementation of PROGALIAM in May 2005.
| Previous Program (January 2003–April 2005) | PROGALIAM (May 2005–December 2007) | |
| Indication of primary angioplasty | First choice for CHUAC patients; selected cases from other centers | Recommended for all patients meeting eligibility criteria |
| Organisation of interhospital transport | Varied according to available resources | All transport in EMS-061 ambulances |
| Direct transfer from outside a hospital | Not available | Available (in EMS-061 ambulances) |
| Abciximab use | Administered in haemodynamics lab at interventional cardiologist's discretion | Administered during transport at lead doctor's discretion |
| Hospital stay following procedure | All patients hospitalised in CHUAC | Stable patients returned to their designated hospitals |
CHUAC, Complejo Hospitalario Universitario A Coruña; EMS 061, Emergency Medical Service, “dial 061”; PROGALIAM, Programa Gallego de Atención al Infarto Agudo de Miocardio (Galician Program for Acute Myocardial Infarction Care).
Before implementation of the new program, PA was the treatment of choice for all patients in the CHUAC district with STEMI at <12h from onset. It was only considered for patients from other hospitals if fibrinolysis was contraindicated or if the patient was in cardiogenic shock.
Under PROGALIAM, the indication for PA was expanded to include all in-hospital or out-of-hospital patients in the Northern Galicia Area suffering from STEMI at <12h from onset at time of diagnosis, with the following specifications4:
• Fibrinolysis could be performed for patients suffering from STEMI at <2h from onset and if the estimated time to PA was >110min.
• PA is preferable for patients suffering from STEMI at >3h from onset.
• PA may be considered in patients suffering from STEMI at >12h from onset in the presence of electrocardiographic symptoms and signs that point toward persistent ischemia.
The electrocardiographic standard for diagnosing STEMI is ST-segment elevation>1mm in two contiguous leads or suspected new left bundle block.
Interhospital TransferUnder the PROGALIAM protocol, all interhospital transfers are made in life-support ambulances pertaining to EMS-061 (Servicio de Emergencias Extrahospitalarias 061, Emergency Medical Service, “dial 061”). These ambulances transport patients directly from the referring center's emergency department to the CHUAC Hemodynamics Laboratory. Before PROGALIAM, the way transport was organised and the ambulance type varied according to availability.
Direct Transport From Other HospitalsPROGALIAM follows a protocol according to which patients meeting criteria for PA who are picked up at an out-of-hospital location by EMS-061 medical ambulances may be transported directly to the CHUAC Hemodynamics Laboratory, regardless of their designated local hospital. In such cases, the EMS-061 doctor will be responsible for telephoning to activate the intervention team. This protocol also applies to STEMI patients diagnosed at a primary care center when a family doctor requests immediate EMS-061 assistance.
Early Administration of AbciximabThe PROGALIAM protocol in force between 2005 and 2007 recommended early administration of abciximab, whether in the emergency department or in the EMS-061 ambulance, to all patients in the absence of contraindication (0.25mg/kg intravenous bolus+continuous infusion of 0.125mg/kg during 12h). This recommendation was recently modified in light of currently available scientific evidence. The strategy of generalized upstream administration of abciximab is no longer employed. Prior to PROGALIAM, abciximab was administered in selected cases in the hemodynamics laboratory, at the hemodynamics specialist's discretion.
ReturnUnder PROGALIAM, a protocol has been established by which patients from noninterventional hospitals who remain in stable condition and without complications during the first 6h after the PA procedure are sent back to their designated hospitals in EMS-061 medical ambulances for the duration of the hospital stay.
ProtocolSix interventional cardiologists accredited by the Hemodynamics Department of the Sociedad Española de Cardiología (Spanish Society of Cardiology) were responsible for the PA procedures. Except where contraindicated, all patients received an initial oral dose of 250mg to 500mg of acetylsalicylic acid, followed by a daily dose of 100mg to 150mg, indefinitely. Patients treated with coronary stents received an oral dose of 300mg to 600mg of clopidogrel before or during the procedure, followed by a daily dose of 75mg for at least 1 month (6-12 months for patients with drug-eluting stents). Other treatments were left to the judgment of the responsible physician.
VariablesThe “symptom onset time” variable was defined as the date and time when STEMI symptoms began as reported by the patient and/or the patient's companions. The time variable “first contact” was defined as the date and time of the patient's first contact with health professionals—hospital emergency services or EMS-061 medical ambulances—which led to activation of the intervention team. The time variable “activation” was defined as the date and time the on-call hemodynamics specialist was notified. The time variable “balloon” was defined as the date and time of the first attempt at inflating an angioplasty balloon or releasing a coronary stent in the lesion responsible for STEMI. Using these variables, we calculated the symptom-to-contact, contact-to-activation, first medical contact-to-balloon time (FMC-B), activation-to-balloon and symptom-to-balloon times. Angiographic success was defined as a post-angioplasty TIMI 3 flow and residual stenosis <20% in the artery that caused STEMI. The time variable “after normal working hours” was defined as weekdays between 15.00 and 8.00, Saturdays, Sundays and public holidays.
Statistical MethodsCategorical variables are given as percentages and continuous variables as mean (standard deviation). Comparisons between groups were done with chi-square and Student-t tests and ANOVA. Due to their asymmetrical distribution, variables relative to delays are presented as median [interquartile range] and compared using the Mann-Whitney and Kruskal-Wallis tests. The statistical significance level was established at P<.05.
Independent predictors of mortality at 30 days and 1 year were identified using stepwise logistic regression analysis (P-out criterion >0.10) including the following variables: age, sex, symptom-to-balloon time, diabetes mellitus, hypertension, obesity, angiographic success, previous myocardial infarction, referral by noninterventional hospitals, infarction location, Killip class IV, multivessel disease and treatment with abciximab. Final models were used to compare adjusted mortality at 30 days and 1 year for patients treated during the PROGALIAM period and the preceding period, those treated in and after normal working hours, and those whose FMC-B was greater than or less than 120min.
A second stepwise multivariable logistic regression analysis (P-out criterion >0.10) enabled us to identify variables associated with FMC-B>120min. The selected variables were the following: age, sex, left bundle-branch block, symptom-to-first-contact time, Killip class IV, after normal working hours, referral from noninterventional hospitals, direct transport by EMS-061, vascular access procedure, diabetes mellitus, hypertension, infarction location, previous myocardial infarction, previous angioplasty, and previous coronary artery surgery. All analyses were performed using PASW version 18.0.
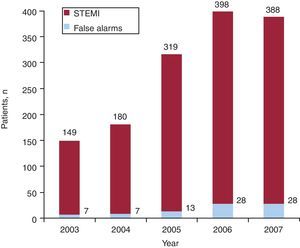
Results ActivityBetween 2003 and 2007, 1434 patients with suspected STEMI were referred to CHUAC to undergo PA, and all underwent at least one diagnostic coronary angiography. Following the implementation of PROGALIAM in May 2005, there was a significant increase in the number of cases (previous protocol, n=402, 14.4 cases/month; PROGALIAM, n=1032, 32.3 cases/month) (Figure 2), accompanied by an increase in the percentage of “false alarms”, that is, patients admitted with a diagnosis other than STEMI (previous protocol, 3.5%; PROGALIAM, 6.7%; P=.02). These “false alarms” (n=83) were excluded from the analysis, and the study population therefore consisted of 1351 patients (previous protocol, n=388; PROGALIAM, n=963).
Figure 2. Changes in the number of patients referred to Complejo Hospitalario Universitario de A Coruña for primary percutaneous transluminal coronary angioplasty during 2003-2007. False alarms, patients admitted with a diagnosis other than ST-elevation myocardial infarction. STEMI, ST-elevation myocardial infarction.
Clinical CharacteristicsAfter implementation of PROGALIAM, both the mean age of the treated population and the percentage of patients referred by secondary hospitals increased (Table 2). Most of the PAs performed under PROGALIAM corresponded to inferior STEMI, while anterior STEMI was more common under the previous program.
Table 2. Clinical Characteristics of 1351 Patients Suffering From an ST-Elevation Myocardial Infarction Referred to Complejo Hospitalario Universitario de A Coruña for Primary Angioplasty Between 2003 and 2007.
| Previous program (n=388) | PROGRALIAM (n=963) | P | |
| Age, years | 61.3±11.9 | 64.2±11.7 | <.001 |
| Patient's hospital of origin | <.001 | ||
| CHUAC district | 314 (81) | 552 (57) | |
| Other medical districts | 74 (19) | 411 (43) | |
| Referring medical service | |||
| Emergency department | 388 | 761 (79) | |
| EMS-061 | 202 (21) | ||
| Women | 60 (15) | 185 (19) | .100 |
| Arterial hypertension | 133 (34) | 358 (37) | .320 |
| Dyslipidaemia | 114 (29) | 303 (31) | .450 |
| Diabetes mellitus | 62 (16) | 165 (17) | .610 |
| Smokers | 177 (46) | 437 (45) | .940 |
| Obesity | 96 (25) | 283 (29) | .090 |
| Prior myocardial infarction | 65 (17) | 95 (10) | <.001 |
| Prior angioplasty | 51 (13) | 91 (9) | .040 |
| Prior coronary surgery | 13 (3) | 22 (2) | .260 |
| Cardiogenic shock | 28 (7) | 58 (6) | .420 |
| Location of infarction | .070 | ||
| Anterior | 183 (47) | 395 (41) | |
| Lower | 176 (45) | 503 (52) | |
| Others | 19 (7) | 65 (7) | |
CHUAC, Complejo Hospitalario Universitario A Coruña; EMS 061, Emergency Medical Service, “dial 061”; PROGALIAM, Programa Gallego de Atención al Infarto Agudo de Miocardio (Galician Program for Acute Myocardial Infarction Care).
Data expressed as no. (%) or as a mean±standard deviation.
Following the implementation of PROGALIAM, the percentage of PAs performed after normal working hours increased. Treatment with abciximab and radial vascular access were used more often in the PROGALIAM period (Table 3). Angiographic success was obtained in 86.8% of patients treated during the previous program, and in 91% of patients treated within the framework of PROGALIAM (P=.02).
Table 3. Characteristics of Interventional Procedure in Study Patients.
| Previous program (n=388) | PROGRALIAM (n=963) | P | |
| Time of procedure | <.001 | ||
| Working hours | 133 (34) | 234 (25) | |
| After normal working hours | 255 (66) | 729 (75) | |
| Vascular access | <.001 | ||
| Femoral artery | 286 (74) | 281 (29) | |
| Radial artery | 102 (26) | 682 (71) | |
| Treatment with abciximab | 144 (37) | 606 (63) | <.001 |
| Coronary disease | |||
| Left main coronary artery | 11 (3) | 41 (4) | .220 |
| Anterior descending | 246 (63) | 623 (65) | .650 |
| Right coronary | 210 (54) | 577 (60) | .050 |
| Circumflex | 145 (37) | 362 (38) | .940 |
| Coronary disease>1 vessel | 180 (46) | 466 (48) | .510 |
| Coronary intervention | |||
| Attempt to perform angioplasty in IRA | 380 (98) | 916 (95) | .020 |
| Stent implanted | 365 (94) | 877 (91) | .110 |
| Conventional stent | 364 (94) | 870 (90) | |
| Drug-eluting stent | 1 (0.3) | 8 (1) | |
| Angiographic success in IRA | 337 (87) | 876 (91) | .020 |
| Multi-vessel angioplasty | 54 (14) | 137 (14) | .930 |
| Complete revascularisation | 228 (59) | 565 (59) | .950 |
| Ventriculography | 299 (77) | 695 (72) | .070 |
| LVEF | 0.57±0.14 | 0.57±0.15 | .810 |
| LVDP (mmHg) | 24.7±9.2 | 26.9±9.4 | .010 |
| ASP (mmHg) | 123±29 | 126.2±28 | .110 |
ASP, aortic systolic pressure; IRA, infarct-related artery; LVDP, left ventricular diastolic pressure; LVEF, left ventricular ejection fraction; PROGALIAM, Programa Gallego de Atención al Infarto Agudo de Miocardio (Galician Program for Acute Myocardial Infarction Care).
Data expressed as no. (%) or as a mean ± standard deviation.
Throughout the Northern Galicia Area, implementation of PROGALIAM led to an increase in the median FMC-B (previous program, 106min; PROGALIAM, 113min; P=.02) (Table 4). However, in the subgroup of patients referred by noninterventional centers, the median decreased significantly (previous program, 171min; PROGALIAM, 146min; P=.01) due to reducing the activation-to-balloon time (medians: previous program, 130min; PROGALIAM, 115min; P<.001). In this subgroup, the percentage of patients with a FMC-B>120min increased significantly (previous program, 17.2%; PROGALIAM, 29.7%; P=.04).
Table 4. Treatment Delay for Patients Receiving Primary Angioplasty During Either of the Periods Under Study.
| CHUAC | Noninterventional hospitals | Total | |||||||
| Previous program (n=315) | PROGRALIAM (n=554) | P | Previous program (n=73) | PROGRALIAM (n=409) | P | Previous program (n=388) | PROGRALIAM (n=963) | P | |
| Symptom-to-first-contact | 99 [117] | 112 [145] | .190 | 110 [195] | 130 [159] | .350 | 100 [123] | 119 [153] | .030 |
| First contact-to-activation | 24 [38] | 23 [38] | .410 | 35 [40] | 26 [41] | .150 | 25 [39] | 24 [39] | .540 |
| Activation-to-balloon | 63 [27] | 63 [29] | .250 | 130 [53] | 115 [42] | <.001 | 68 [44] | 80 [56] | <.001 |
| First medical contact-to-balloon | 94 [56] | 92 [53] | .740 | 171 [88] | 146 [76] | .010 | 106 [72] | 113 [71] | .020 |
| Symptom-to-balloon | 210 [145] | 214 [177] | .360 | 292 [229] | 284 [208] | .500 | 218 [165] | 242 [200] | .010 |
CHUAC, Complejo Hospitalario Universitario A Coruña; PROGALIAM, Programa Gallego de Atención al Infarto Agudo de Miocardio (Galician Program for Acute Myocardial Infarction Care).
Time intervals are presented as a median [interquartile range] in minutes.
For the CHUAC patient subgroup, implementing the new protocol did not significantly affect FMC-B (medians: previous program, 94min; PROGALIAM, 92min; P=.74). In this subgroup, the percentage of patients with a FMC-B>120min was 69.3% during the previous program and 71.3% under PROGALIAM (P=.56).
Table 5 shows the factors associated with FMC-B >120min. The strongest predictive factor for a delay >120min was referral from a noninterventional center (odds ratio [OR]=10.6; 95% confidence interval [95%CI], 7.7-14.6; P=.001).
Table 5. Factors Associated With a Delay >120 min for First Medical Contact-to-Balloon Time: Multivariate Analysis.
| OR (95%CI) | P | |
| After normal working hours | 1.48 (1.09-2.02) | .012 |
| Direct transport from other hospitals | 0.15 (0.01-0.23) | <.001 |
| Transport from noninterventional hospital | 10.6 (7.7-14.6) | <.001 |
| Left bundle-branch block | 2.83 (1.07-7.52) | <.001 |
| Women | 1.50 (1.06-2.14) | .023 |
| Symptom-to-first-contact time (10 min) | 1.008 (1.001-1.016) | .028 |
| Age | 1.017 (1.006-1.028) | .003 |
95%CI, 95% confidence interval; OR, odds ratio.
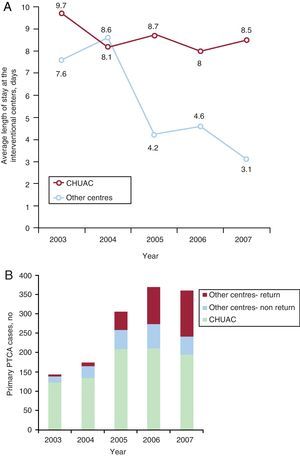
Following implementation of PROGALIAM, we observed a decrease in average length of stay at the interventional center for patients referred from other medical districts. Likewise, the percentage of patients who returned to their designated local center to continue hospitalization after undergoing PA increased. The mean length of stay for patients from the CHUAC medical district remained unchanged (Figure 3).
Figure 3. Changes in average length of stay at the interventional center for patients referred for primary angioplasty between 2003 and 2007. A: according to hospital of origin. B: patient's destination hospital following the procedure. CHUAC, Complejo Hospitalario Universitario de A Coruña; PTCA, percutaneous transluminal coronary angioplasty.
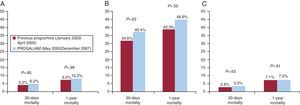
PrognosisWe did not observe significant differences between the two programs in mortality rates at 30 days or at 1 year; the prognosis was particularly poor for patients in cardiogenic shock (Figure 4). Patients from noninterventional hospitals presented lower 30-day mortality rates than CHUAC patients (4.1% vs 6.9%; P=.04), with no differences between the two groups in 1-year mortality (8.5% vs 10.2%; P=.18). We observed a strong correlation between procedure results and 30-day mortality (angiographic success, 3.4%; no success, 20.5%; P<.001) and at 1 year (angiographic success, 7.3%; no success, 30.3%; P<.001).
Figure 4. Mortality at 30 days and 1 year for patients treated with primary angioplasty during the two periods under study. A: sample total. B: patients in cardiogenic shock upon arrival at the hemodynamics laboratory. C: patients without cardiogenic shock. PROGALIAM, Programa Gallego de Atención al Infarto Agudo de Miocardio (Galician Program for Acute Myocardial Infarction Care).
Multivariate analysis showed an independent correlation for age, symptom-to-balloon time, presentation with cardiogenic shock, and angiographic success with 30-day and 1-year mortality rates (Table 6). After adjusting for those variables, we did not observe that the program under which the procedure was performed (PROGALIAM or the previous program) had an independent influence on mortality at 30 days (OR=1.1; 95%CI, 0.6-2.2) or at 1 year (OR=1; 95%CI, 0.5-1.5).
Table 6. Factors Associated With Mortality at 30 Days and 1 Year of the Procedure: Multivariate Logistic Regression Analysis.
| OR (95%CI) | P | |
| 30 days | ||
| Age, years | 1.06 (1.03-1.09) | <.001 |
| Angiographic success | 0.34 (0.17-0.68) | .002 |
| Cardiogenic shock | 14.1 (7.1-28.3) | <.001 |
| Symptom-to-balloon time | 1.08 (1.01-1.16) | .026 |
| 1 year | ||
| Age | 1.06 (1.04-1.08) | <.001 |
| Angiographic success | 0.28 (0.17-0.48) | <.001 |
| Cardiogenic shock | 7.7 (4.1-14.3) | <.001 |
| Diabetes mellitus | 1.57 (0.95-2.60) | .070 |
| Symptom-to-balloon time | 1.05 (0.99-1.11) | .070 |
95%CI, 95% confidence interval; OR, odds ratio.
Patients treated with PA after normal working hours were younger (63 [12.7] vs 64.5 [12.2] years of age; P=.49); more likely to be referred from a noninterventional hospital (37.5% vs 31%; P=.03); more likely to receive abciximab (59.6% vs 45.4%; P<.001); and had a longer median FMC-B (113min vs 99min; P<.001) and symptom-to-balloon time (240min vs 213min; P=.01) than patients treated during working hours. We did not observe differences between the two groups with regard to angiographic success rates (working hours, 91.1%; after normal working hours, 89.4%; P=.37), 30-day mortality (working hours, 6.7%; after normal working hours 5.5%; P=.39) or 1-year mortality (working hours, 11.9%; after normal working hours 9.2%; P=.14). Following adjustment for the variables listed in Table 6, we found no significant influence of the variable “after normal working hours” on 30-day mortality (OR=0.93; 95%CI, 0.49-1.75) or 1-year mortality (OR=0.81; 95%CI, 0.51-1.29).
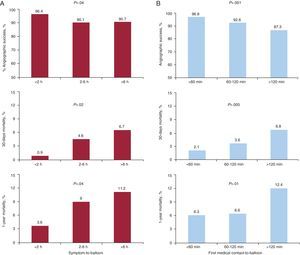
Prognostic Influence of Delay TimeAs shown in Figure 5, univariate analysis shows a significant association between FMC-B and symptom-to-balloon time with angiographic success rates and 30-day and 1-year mortality rates. After adjusting for the variables listed in Table 6, the association between FMC-B>120min, 30-day mortality (OR=1.41; 95%CI, 0.79-2.52; P=.24) and 1-year mortality (OR=1.47; 95%CI, 0.96-2.25; P=.08) lost statistical significance.
Figure 5. Influence of the sympton-to-balloon (A) and first medical contact-to-balloon time (B) on the rates of angiographic success, 30-day mortality, and 1-year mortality in patients treated with primary angioplasty.
DiscussionThe most immediate consequence of a program to generalize PA is the increase in the number of patients receiving treatment, and therefore in the workload. In our center, implementing PROGALIAM doubled the number of procedures performed by increasing activity after normal working hours. In order to deliver the desired results, these programs must rely on highly qualified, dedicated professionals who understand that the foreseeable “decrease in their own quality of life” will provide important benefits to their patients. This is obviously true for members of the interventional cardiology team (doctors and other staff), but the new program will have an impact, be it large or small, on all professionals involved in the process. It is therefore important to reach agreements regarding the terms of the program during the planning stage (goals, compensation, on-call schedules, etc.)5
In our case, the increase in PA activity was due to extending treatment to a less selected, older population with a higher percentage of female patients, longer times from symptom onset, and longer transport distances. As a whole, PROGALIAM successfully maintained 30-day and 1-year mortality rates similar to those from the previous program and from other reference networks.6 These results are based on the high rate of angiographic success, considering the well-known association between that parameter and survival in patients treated with PA.7 Generalized use of abciximab may have contributed to this result, since it has been demonstrated that in the context of PA this drug improves the effectiveness of mechanical reperfusion and reduces morbidity and mortality.8 Other factors that may have had an impact on the results are the combined experience of the intervention team, improved techniques in the field of PA, or extending this treatment to patients at lower risk (for example, inferior STEMI). We should point out that, unlike other groups,9 we did not observe differences in program results correlating to the time of day when the procedure was undertaken or the hospital referring the patient. This reflects uniform and equitable health care services.
One interesting aspect of our study was discovering that, in a real-world care setting, patients treated with PA often have a longer FMC-B than that recommended by clinical practice guidelines.10 This tendency is more marked in the group of patients referred by noninterventional hospitals, as less than one-third of these patients receive treatment within the target FMC-B of <120min recommended by clinical practice guidelines.1 This variable is a strong predictor of mortality in patients treated with PA, regardless of symptom-to-first-contact time and total ischemia time.11 The authors are aware that long distances separate peripheral health centers and the interventional hospital in this geographic area; measures aimed at reducing FMC-B are absolutely necessary and a top priority for the program.
However, we must stress that launching the new program has indeed led to a modest but statistically significant improvement of some 25min in overall FMC-B for patients transported from peripheral centers. We attribute this improvement to implementing interhospital transport and direct transport protocols (EMS-061 mobile units). A previous analysis12 by our group showed that the latter strategy is associated with a significant decrease in FMC-B and early mortality, compared with the conventional practice where only emergency departments may alert the intervention team. We believe that implementing new organizational care measures may contribute to further improvements in the future. One example that might be followed is the D2B Alliance initiative,13 under which simultaneous use of several medical strategies—emergency service doctors or EMS staff alerting the intervention team, commitment by the intervention team to be ready in<30min, ability to activate the entire team by means of a single telephone call, real time information feedback—led to 3 out of 4 patients being treated with a FMC-B<90min. However, we must not lose sight of the fact that these strategies involve transferring the responsibility of activating the intervention team to noncardiologists. For this reason, one possible adverse result may be an increase in “false alarms.” Our experience supports this impression, as presented in detail in a previous study14 published in this journal.
We have identified several factors associated with a significant increase in FMC-B in our cohort. Some of these factors are inherent in the health care system, such as the need to transfer a patient to another hospital15—the strongest predictive factor for a FMC-B<120min in our study—or occurrence after normal working hours,15 when mobilizing the intervention group contributes to the delay because members are not physically present at the hospital. Certain factors inherent in the patient, such as advanced age,16 female sex,16 or left bundle-branch block may also contribute to increase FMC-B due to making diagnosis more difficult. The observed correlation between symptom-to-first-contact time and FMC-B is harder to understand. Hypothetically, prolonged symptom-to-first-contact time may reflect an atypical clinical presentation that does not induce the patient to seek medical care and raises questions in the mind of the primary doctor. This complicates diagnosis of the condition and timely activation of the hemodynamics laboratory. It is also possible that some patients who seek medical attention for STEMI that has been evolving for several hours only show discrete, residual displacement of the ST-segment. This would lead a doctor to question whether or not a PA would be beneficial in such a case, and therefore affects the motivation to reduce delay.
One important aspect of planning a regional PA program is designing measures to prevent excessive occupation of hospital beds in the interventional center. This is the main objective of the PROGALIAM protocol for returning stable patients to their designated medical centers. A preliminary analysis by our group shows that this strategy is feasible and safe, and allows more than 70% of patients referred from secondary centers to return to those centers.17 The progressive decrease in the average length of stay in the interventional center for patients from peripheral areas is a direct consequence of that measure.
The lack of external monitoring is the study's main limitation. In addition, the lack of information relative to patients not receiving PA prevents us from demonstrating PROGALIAM's beneficial effect on the overall survival of STEMI patients in our area of reference. However, we should point out that the main purpose of this study is to describe the changes and medical difficulties that arose following implementation of a generalized PA program, from the point of view of an interventional cardiology unit, so that other groups might learn from our experience when planning similar new initiatives. We should also recall that this study only offers information regarding PROGALIAM results in Northern Galicia Area. Its conclusions might not be extrapolated to other areas of Spain or even to any other Galician interventional hospitals that also participated in the program.
ConclusionsAnalysis of our PA program's activities between 2003 and 2007 shows that designing a regional hub-and-spoke medical network for STEMI makes it possible to significantly increase the number of patients benefiting from this treatment without compromising results or substantially increasing the medical resources provided for this activity. Drawing up a detailed plan that accounts for the expected increase in interventional activity and potential changes in the clinical profile of the treated population is absolutely necessary. The plan must account for the medical resources needed to obtain a high angiographic success rate, keep reperfusion delay within the recommended limits, minimize the proportional increase in “false alarms”, and avoid overloading hospital beds in the interventional center.
Conflicts of interestNone declared.
Acknowledgements
The authors would like to express their gratitude to all of the health care professionals involved in the STEMI integral care network in Northern Galicia Area, and whose efforts and dedication support PROGALIAM day after day.
Received 28 April 2011
Accepted 7 November 2011
Corresponding author: Servicio de Cardiología, Hospital Universitario A Coruña, As Xubias 84, 15006 A Coruña, Spain. blargesbueno@hotmail.com