Keywords
INTRODUCTION
B-type natriuretic peptide (BNP) is mostly synthesized in the left ventricle, is released in response to pressure and volume overload, and has a beneficial effect in patients with heart failure.1,2 In recent years the measurement of BNP has become an aid in the diagnosis3-5 of heart failure and in determining the prognosis of patients with this syndrome.4-6 However, while a number of papers have reported increased BNP levels to be associated with a poorer prognosis, beta-blocker (BB) treatment was suboptimal in the majority of populations studied.6-10 Treatment with these agents improves patient prognosis11,12; however, it also affects BNP values in a variable fashion.13-16 The prognostic value of BNP in patients receiving optimized therapy including BB remains unclear.
Risk stratification is routine clinical practice when treating patients with heart failure (this is particularly true in heart transplantation units). An exercise test, involving measurement of respiratory gases or cardiopulmonary monitoring, particularly the measurement of maximum oxygen consumption (VO2max), is a classic tool used in prognostic stratification and decision-making.17,18 However, it was developed using populations that were not receiving optimized treatment including BB.18 Further, the VO2max loses its prognostic potential in patients with intermediate functional deterioration who are receiving optimized treatment including BB.18 Patients who receive BB have a better prognosis for an equivalent VO2max,19,20 such that the recommended cut-off indicating the need for heart transplantation is reduced from 14 mL/kg/min to £12 mL/kg/min.17,21
The aim of the present study was to determine the usefulness of BNP and the cardiopulmonary exercise test on the long-term risk stratification of patients with systolic heart failure and intermediate functional deterioration receiving optimized treatment including BB.
METHODS
Study Design and Patients
The potential study subjects were consecutive outpatients who attended a clinic for advanced heart failure associated with a heart transplant program during 2003-2004. Medical treatment was optimized according to the guidelines in force at the time.22 The final study population (n=80) was composed of patients receiving optimized treatment that included BB plus an angiotensin converting enzyme inhibitor (ACEi) or an angiotensin II receptor antagonist (ARA-II) (both at the maximum tolerated dose). These patients were all clinically stable; none had been subject to any changes in therapy, or hospitalized within the previous 3 months. All patients underwent cardiopulmonary exercise testing; none showed a need for heart transplantation in the short term. Coronary angiography was performed in 58 patients (70%) in whom coronary artery disease had not been ruled out. Following a treatment optimization period, all patients underwent experimental testing on the same morning. All echocardiographic and exercise tests were performed by the same operator. Echocardiography was performed using a Sonos 5500 apparatus (Philips, Andover, Massachusetts) before the exercise test, after taking a sample of blood. The left ventricular ejection fraction (LVEF) was calculated using the Simpson method and employing a second harmonic image. Standardized projections were performed and standard measurements taken for the study of heart anatomy and function.23
BNP and Other Blood Variables
After an overnight fast, and following a rest period of 20 min, blood was obtained by venipuncture of the antecubital vein using a vacuum system. Samples for the determination of BNP were collected in polystyrene tubes containing ethylenediaminetetraacetic acid (500 kIU/mL) and immediately placed on ice. All were centrifuged within 60 min. The plasma fraction was stored at -80oC until analysis. Plasma BNP was determined in duplicate using a sandwich-type solid phase radioimmunoanalytical technique employing the ShionoRia BNP kit (CIS Bio International, Gif sur Yvette, France). The lower detection limit was 2 pg/mL. Cross reactivity with atrial natriuretic peptide is specified by the manufacturer as <0.001%. The coefficient of variability was 6%. The normal concentration of BNP defined by the manufacturer was <18.4 pg/mL. The physicians responsible for the management of the patients were kept blind to the BNP results; they were not, therefore, available to them for therapeutic decision-making.
Hemoglobin and hematocrit were determined using an XE-2100 model automated blood analyzer (Symex, Kobe, Japan). Other biochemical variables were determined using a Roche/Hitachi Modular Analyzer (Roche Diagnosis, Mannheim, Germany). The glomerular filtration rate (GFR) was calculated using the simplified modification of diet in renal disease (MDRD) formula (mL/min/1.73 m2: 186.3´[plasma creatinine]-1.154´[age]-0.203) (´0.742 to correct for female sex).
Cardiopulmonary Exercise Test
Using (Marquette, Milwaukee, USA) a modified Bruce protocol, all subjects underwent a cardiopulmonary exercise test. Values for gas exchange and ventilation variables were obtained using a pneumatograph and analyzer (CPX System, Medical Graphics Corp., St. Paul, Minnesota, USA); values for oxygen consumption (VO2), carbon dioxide production (VCO2), and minute ventilation (VE) were recorded every 10 s. The patients were encouraged to exercise until exhaustion. All reached the anaerobic threshold and showed a respiratory quotient of >1.05. Continuous electrocardiographic monitoring (12-lead) was performed throughout the test. Blood pressure was measured every minute using a cuff sphygmomanometer. All patients stopped exercising due to dyspnea or fatigue; none stopped because of chest pain or ischemic alterations to the ST segment. The VO2max was established as the value in the final phase of exercise, and was expressed as mL/kg/min. The slope for the relationship between minute ventilation and the production of carbon dioxide (VE/VCO2) provided the coefficient of the ventilatory response to exercise or ventilatory inefficiency.24 The operator who performed the exercise test was blind to the BNP values recorded for the patients.
Clinical Follow-up and Events
Patients were followed up for a period of 2.7 (0.8) years; no patient was lost to follow-up. The adverse events recorded were death due to cardiovascular cause, heart transplantation, and hospitalization due to heart failure. The need for urgent heart transplantation was considered equivalent to death. The main end points recorded were death, and its combination with heart transplantation, and/or hospitalization due to heart failure.
Statistical Analysis
The Kolmogorov-Smirnov test was used to check the normal distribution of quantitative variables. BNP values showed a deviation from normality, and were therefore log-transformed for analysis; values are expressed as medians and interquartile range. Normally distributed quantitative variables were expressed as means (standard deviation [SD]); qualitative variables were expressed as number (and percentage). Comparisons between groups were undertaken using the Student t test for independent samples. Univariate Cox regression was used to study the possible predictors of events. The best prognostic cut-off was taken as that which maximized specificity and sensitivity in the analysis of the receiver operating characteristic (ROC) curve. The cut-off thus obtained was used in Kaplan-Meier survival analysis (log rank). Variables that were significant in the univariate Cox regression were used in multivariate Cox analysis (conditional forward stepwise method), adjusting for possible confounding factors. A P value less than .05 was considered significant. All calculations were performed using SPSS software for the social sciences (SPSS v. 14.0 for Windows, SPSS Inc., Chicago, Illinois, USA).
RESULTS
Population and Events
The study population was composed of 80 patients (78% were men; mean age 50 [11] years). Table 1 records the patients' clinical characteristics. As a whole the subjects showed severe systolic ventricular dysfunction (LVEF 25% [9%]) and intermediate functional deterioration (NYHA class I/II/III, 4/42/34 [2.4 (0.6)]). The etiology of heart failure in the majority (74%) was non-ischemic.
Table 2 shows the pharmacological treatment received. All 80 patients received optimized treatment including a BB and either an ACEi or an ARA-II drug.
Seven patients (8.8%) died during follow-up (4 suddenly, 3 from refractory cardiogenic shock). Another 6 (7.5%) required a heart transplant, and a further 6 (7.5%) were hospitalized at least once for decompensated heart failure. In total 19 (24%) patients experienced some adverse event during follow-up.
BNP Concentration and Prognosis
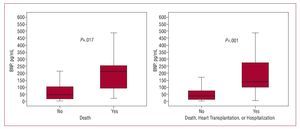
The median BNP concentration was 64 (17-130) pg/mL. It was significantly higher in patients who died than in those who did not (n=7, 211 [51-266] pg/mL vs 46 [16-105] pg/mL; P=.017), in those who required a heart transplant compared to those who did not (n=6, 226 [88-527] pg/mL vs 47 [17-108] pg/mL; P=.006), and in patients associated with the combined event death/heart transplantation/hospitalization compared to the remaining patients (n=19, 139 [88-286]) vs 40 [13-81] pg/mL; P<.001) (Figure 1).
Figure 1. Box diagram comparing BNP values (pg/mL) and the appearance of events during follow-up.
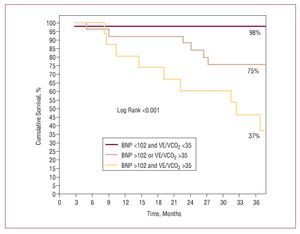
The area under the ROC curve for the prediction of death was 0.773 (95% CI, 0.670-0.859); for any adverse event it was 0.814 (95% CI, 0.711-0.892). In both cases the best cut-off was 102 pg/mL (sensitivity and specificity 72% and 74%, and 79% and 80% respectively). The negative predictive value were was 96% and 93%, respectively. Kaplan-Meier survival analysis showed event-free survival to be shorter in patients with a BNP of >102 pg/mL (log rank <0.001) (Figure 2).
Figure 2. Kaplan-Meier cumulative event-free survival curves according to BNP values below or above the optimum reference value.
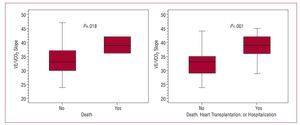
Exercise Test Results and Prognosis
Patients performed exercise for 6 (2.5) min; the mean VO2max was 19 (5) mL/kg/min and the mean VE/VCO2 slope value 34 (6). The VE/VCO2 slope was steeper in patients who died (n=7; 39 [3] compared to 33.8 [5.5] in those who did not; P=.018) and in those included in the combined adverse event outcome (n=19; 38.7 [4.3] compared to 32.9 [5.2]; P<.001) (Figure 3). No significant differences were seen in VO2max between those who died and those who did not (17.2 [2.9] compared to 19.2 [5.3]; P=.332), although differences were seen when a similar comparison was made for the combined adverse event (16.8 [3.9] compared to 19.7 [5.4]; P=016).
Figure. 3. Box diagram comparing the value of the VE/VCO2 slope against the appearance of adverse events during follow-up.
The VE/VCO2 slope showed an area under the ROC curve for the prediction of death of 0.805 (95% CI, 0.702-0.885); the optimum cut-off was 35 (sensitivity 100%, specificity 69%, negative predictive value 100%). For the combined end point, the area under the curve was 0.814 (95% CI, 0.712-0.893); the best cut-off point was also 35 (sensitivity 84%, specificity 71%, negative predictive value 94%). Kaplan-Meier analysis showed event-free survival to be shorter in patients with a VE/VCO2 slope value of 335 (log rank <0.001) (Figure 4).
Figure 4. Kaplan-Meier cumulative event-free survival curves, according to BNP VE/VCO2 slope values below or above the optimum reference value.
Multivariate Analysis
Following adjustment for the different variables in Cox multivariate regression analysis, a BNP of >102 pg/mL and a VE/VCO2 slope of >35 were identified as independent predictors of adverse events (Table 3).
Kaplan-Meier analysis showed the presence of neither, one and both predictors to be associated with a cumulative incidence of 2%, 25%, and 63% (log rank <0.001).
DISCUSSION
The results show the plasma BNP concentration and the VE/VCO2 slope (under cardiopulmonary exercise) to be the main markers of long-term risk of developing an adverse event.
Risk stratification forms part of clinical practice associated with the management of patients with heart failure (especially in heart transplantation units); VO2max has been the traditional risk measurement tool.18 However, in patients with intermediate functional deterioration, such as those in the present study, risk stratification is more difficult—albeit of great importance with respect to the medium-long term prognosis. In recent years, BNP has become recognized for its long-term prognostic value, although its dependence on the population studied has limited its use as a prognostic tool in individual patients. The use of BB seems to affect BNP concentration; some authors report it to become reduced13,14 while others report it to undergo a significant increase.15,16 This might be explained in that beta adrenergic modulation interacts with the synthesis, secretion, and clearance of BNP2; an initial increase in BNP concentration would therefore be expected, followed by a progressive reduction in parallel with the clinical and echocardiographic improvement made.26 The present patients all had stable heart failure and had received BB for at least three months before the start of the study; the mentioned interaction may therefore have been minimized.
Figure 5.Kaplan-Meier cumulative event-free survival curves depending on whether the BNP concentration was >102 pg/mL or not, and/or the VE/VCO2 slope value was >35 or not.
BNP levels were found to be a significant prognostic marker of adverse events taken into account. Other studies involving similar outpatient populations with different percentages receiving BB report similar findings, eg, that of Koglin et al8 (n=78; 75% of patients in NYHA class II/III) in which 79% of patients received BB, and that of Stanek et al27 (n=91; 98% of patients in NYHA class II/III) in which 55% received BB. In the present study, in which all patients received BB, BNP levels were of great prognostic significance, and the results confirm its independence of BB treatment. The same is indicated by the VAL-HEFT registry, in which the prognostic value of BNP appears independent of treatment with BB or ACEi.7 Since BNP values are influenced by the characteristics of the population studied, and given their linear association with the increase in risk, earlier studies described many different prognostic reference values, hindering the practical use of this marker.4-10,28,29 In the present outpatients, all of whom received optimized treatment (all received BB and ACEi, or ARA II), a BNP of <102 pg/mL was associated with a good prognosis (7% adverse events), while the persistence of high values was associated with a significantly increased risk (55%) of an adverse event in the long term (36 months). This agrees with the findings of the VAL-HEFT study (which has the largest number of patients in such a study to date), in which appropriately treated outpatients showed BNP values below the cut-off for the diagnosis of heart failure (100 pg/mL); this was therefore associated with a better prognosis.28,29 These findings therefore indicate that, in similar outpatient populations (it should be emphasized that this is only the case for populations similar to those described in the latter and present studies), and when administering treatment with BB and ACEi or ARA-II, BNP values below 100 pg/mL are associated with a significantly better prognosis.
The prognostic value of VO2max was affected by treatment with BB; these drugs reduce the capacity to perform exercise but at the same time improve patient prognosis.17,21 In the present population the VE/VCO2 slope value was a more valuable prognostic marker than VO2max. This may be partly due to the patients' intermediate functional deterioration, as shown by the VO2max reached (19 [5] mL/kg/min) which was significantly above the cut-off value of 12 mL/kg/min indicated by Peterson et al.21 Several authors report the prognostic value of measuring ventilatory inefficiency in response to exercise via the VE/VCO2 slope, rating it even higher than that of VO2max, especially in populations showing intermediate functional deterioration.24,30-32 The latter studies involved populations in which under 50% of patients were treated with BB. In the present study the mean VE/VCO2 slope value was 34 (6), close to the prognostic cut-off point obtained (>35, which is similar to that previously published).17,30-32 Thus, the present results indicate that, in patients treated with BB and with intermediate functional deterioration, the loss of ventilatory efficiency during exercise (the value of the VE/VCO2 slope) could be a better long-term prognostic marker than VO2max. de Groote et al,33 who studied a large population (n=407) in which 93% of patients received BB, reported BNP and VO2max (measured as a percentage of that predicted) to be of independent prognostic value. These results agree with those of the present study in that, despite the fact that BNP concentration has been shown a determinant of the functional capacity and the VO2max reached,34,35 the prognostic information it provides complements that offered by the cardiopulmonary exercise test. Nonetheless, the study by de Groote et al does not take the VE/VCO2 slope value into account; this was examined in the present study and it was found to be of greater prognostic value than the VO2max. In addition, the population studied by the latter authors showed greater functional deterioration (VO2max, 15.2 [4.8] mL/kg/min), which might determine a greater prognostic value for VO2max. This shows that the VE/VCO2 slope may be of greatest value in populations showing intermediate functional deterioration, while VO2max may be more reliable in populations showing greater deterioration.
Limitations
The main limitation of this study lies in the characteristics of the population examined, which prevent the results to be extrapolated to others. The present population included relatively young, clinically stable outpatients with severe ventricular dysfunction, and intermediate functional deterioration; correct medium-long term risk stratification is of great importance in such patients. The findings presented may be of use in the management of similar patients in heart transplantation programs; in such programs, patients who do not meet the criteria for inclusion on the transplant list following the optimization of treatment, but which are at higher risk, should be monitored more carefully. Another limitation is the small size of the study population (due to the characteristics selected), although to some extent this is compensated by the long follow-up period. Finally, the rate of events may appear low, but it reflects that which might be expected for similar populations following current therapeutic guidelines.36 The possible effects of the type of BB administered could not be studied due to the small population size.
CONCLUSIONS
In outpatients with heart failure who show severe ventricular dysfunction and intermediate functional deterioration, for whom a heart transplant in the short term is not indicated, and for whom treatment has been optimized (including the administration of BB), the persistence of a BNP concentration of >102 pg/mL and ventilatory inefficiency in response to exercise expressed as a VE/VCO2 slope of >35 indicate a greater long-term risk of complications.
ABBREVIATIONS
ACEi: angiotensin converting enzyme inhibitor
ARA-II: angiotensin II receptor antagonist
BB: beta-blocker
BNP: B-type natriuretic peptide
GFR: glomerular filtration rate
LVEF: left ventricular ejection fraction
ROC curve: receiver operating characteristic curve
VE/VCO2: ventilatory efficiency (minute ventilation/carbon dioxide production)
VO2max: maximal oxygen consumption
Correspondence:
Dr. D.A. Pascual Figal. Benabia, 7. 30110 Murcia. España.
E-mail: dapascual@servicam.com
Received March 12, 2007.
Accepted for publication October 31, 2007.