The correct response is 3, ventricular tachycardia with suspicion of right ventricular disease.
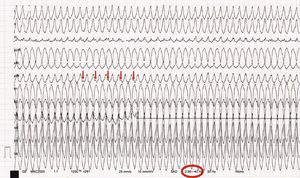
Close examination of the ECG reveals positive P waves, not associated with the tachycardia, in leads II and aVF, suggesting a ventricular origin (Figure 1, arrows) and so ruling out options 2 and 4.
Changes in biomarkers of myocardial injury and ST-segment abnormalities (particularly in right precordial leads using ECG filters that are not recommended [0.01 – 40/50Hz]) after cardioversion of ventricular tachycardia may lead to false diagnosis of an acute coronary event. Of note is the suboptimal filtering in the ECG taken during tachycardia and after cardioversion (Figure 1, circle). Therefore, there are no objective data to support option 1.
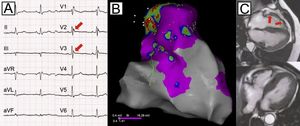
When the QRS axis lies between 0° and 60° and is similar in the 12 leads during ventricular tachycardia and sinus rhythm, an arrhythmic origin between the His region and the low right ventricular outflow tract should be suspected.1 This area is often affected in right ventricular dysplasia. The relationship with prior exercise-induced syncope and documented arrhythmia, the origin of this arrhythmia, and the appearance of epsilon waves in subsequent ECGs (Figure 2A, arrows) led to diagnosis of right ventricular cardiomyopathy, confirmed by electroanatomic mapping (Figure 2B) and cardiac magnetic resonance imaging (Figure 2C).2
.