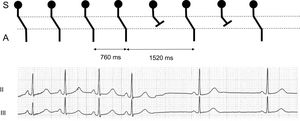
The correct answer is number 3. As shown in Figure 1, the P-P cycle exactly doubles. This finding strongly suggests a 2:1 sinoatrial (S-A) block. Sympathovagal imbalance and respiratory sinus arrhythmia would have generated a gradually lengthening and shortening of the P-P cycle in a cyclical fashion, usually corresponding to the phases of the respiratory cycle or other autonomic reflexes. Thus, answers 1 and 2 are incorrect. A concealed atrioventricular (A-V) node reentry cannot explain sinus node depression. Moreover, the ECG would have shown a trigger, preceding the pause, such as a Wenckeback phenomenon or a premature atrial impulse.1 For this reason, answer 4 is incorrect.
The sinus impulse is only recorded by the ECG once it has left the sinus node and activated the atrium, thereby resulting in the P wave.2 Delay in conduction at the S-A junction, such as that occurring during a first-degree S-A block is, therefore, not visible electrocardiographically. Second-degree S-A blocks can be revealed by a careful analysis of the ECG. A Wenckebach conduction defect at the S-A level will present as progressive acceleration of the P-P intervals, analogously to the progressive acceleration of the R-R intervals in an A-V Wenckebach disturbance. Pause is less than twice the preceding P-P cycle.3 In contrast, an abrupt doubling of the P-P cycle excludes a second-degree Mobitz type 2 or a 2:1 S-A block. It is worth noting that sinus bradycardia and 2:1 S-A block are indistinguishable on an ECG, unless an abrupt change in heart rate clarifies the underlying mechanism. Advanced S-A block will be revealed by a pause that is a multiple of> 2 of the P-P cycle. ECG of third-degree S-A block is analogous to sinus arrest.