Aortic stenosis (AS) is the most common single-valve disease according to the latest European registry known as the Valvular Heart Disease II Survey and accounts for 41.2% of the entire cohort studied.1 The increase in the prevalence of this condition is proportional to age, with the registry showing that 26.5% of patients with AS were older than 80 years. It is estimated that the prevalence will rise in upcoming decades in Europe due to the aging population and the decrease in rheumatic fever cases in developing countries. Indeed, the proportion of AS patients has increased almost 7% over the past 2 decades in Europe, and the number of patients older than 80 years with AS has increased by almost 20% since 2001.1 Clinical practice guidelines currently recommend intervention as early as possible in symptomatic patients due to the poor prognosis.2 Nevertheless, many patients are classified as asymptomatic and, therefore, valve repair is only indicated if left ventricular ejection fraction is low or if conventional exercise testing is not tolerated. If patients meet neither condition, only outpatient follow-up and conservative treatment are recommended.2 Early intervention in symptomatic patients is based on studies in a relatively young population with a mean age around 65 years, few comorbidities, and low surgical risk.3 However, decision-making in valve repair in asymptomatic patients is not entirely straightforward. Even the elderly population may be mistakenly classified as asymptomatic because they have reduced their physical activity to avoid symptoms or because they have symptoms that are mild or hard to differentiate from those arising from comorbidities, such as aging, frailty, obesity, or others.4,5 To answer this question, 3 clinical trials are currently underway to evaluate the best timing for invasive treatment of AS (EARLY TAVR [NCT03042104], EASY-AS [NCT04204915], EVoLVeD [NCT03094143]2), and published results are available for the RECOVERY3 and AVATAR6 trials.
Oxygen uptake or cardiopulmonary exercise testing (CPET) is a noninvasive functional assessment technique used in cardiology for 40 years, with the earliest studies performed in heart failure with reduced left ventricular ejection fraction.7 This test has improved considerably over the years and provides a large amount of highly valuable diagnostic and prognostic information. The advantage of CPET is that it estimates exercise capacity and evaluates an individual's pathophysiologic responses in relation to the increase in the metabolic needs of the body, as it analyzes gas exchange (mainly O2 and CO2) and other ventilatory variables.7 Its indications have not previously included the study of valve diseases due to a lack of data, but the clinical assessment of valve disease by CPET has been considered an option since 2017.7 Despite the clinical evidence available, the usefulness of CPET is not mentioned in the 2017 clinical guidelines for the US or in the recent clinical recommendations for valve disease issued by the European Society of Cardiology.2,8,9 This omission is noteworthy, because the pathophysiology of valve disease, such as retrograde pulmonary arterial hypertension and decreased cardiac output, can be analyzed by CPET and may unmask symptoms of apparently asymptomatic valve disease, stratify risk, and aid decision-making on valve repair in individuals with no clear symptoms.10 When a patient has aortic valve disease, good cardiovascular accommodation is crucial to an increase in cardiac output, which may sometimes be 5- to 6-fold the baseline value.5 Patients with aortic valve disease would have issues when managing this necessary increase in cardiac output, which progresses to increased retrograde pulmonary pressure or an inability to increase output.5
The increased incidence and prevalence of asymptomatic severe AS may lead to an excess health care burden in the future, as patients with moderate AS and extensive valve calcification require clinical follow-up at least every 6 or 12 months.2 It is also crucial to properly classify patients with symptomatic or asymptomatic severe AS, because progress is poor after the onset of symptoms. At present, the only test recommended to unmask these symptoms is the conventional exercise test, with the limitations this study may entail.2,9 This is supported by the results of a 2009 meta-analysis with 491 patients from 7 studies showing that the result of a normal exercise test implied, on the one hand, a low risk of cardiac events at 12 months of follow-up (odds ratio=0.12; 95% confidence interval [95%CI], 0.07-0.21; P=.001) and, on the other, was shown to be a protective predictor against sudden cardiac death during follow-up (odds ratio=0.23; 95%CI, 0.03-1.01; P=.05).11 However, the conventional exercise tests used to follow-up patients with asymptomatic severe AS do not distinguish between ending the test due to aortic valve disease symptoms (ventilatory issue), muscle fatigue, or not achieving adequate exertion despite symptoms.
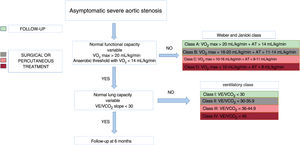
CPET has gained traction as a useful tool to study AS, as using a gas analyzer to measure pulmonary ventilation and respiratory gas exchange provides an objective, more specific approximation of the patient's clinical condition.7 Like the conventional exercise test, the CPET has proven to be safe in patients with AS when done under the supervision of qualified personnel.12 In 2014, Dhoble et al.4 evaluated which CPET parameters had prognostic impact in patients with asymptomatic severe AS. After a mean follow-up of 5.1±4.2 years in 155 patients, those who had peak oxygen uptake (pVO2)> 80% of the age-and sex-predicted level had longer survival than those with pVO2 <80% of the age-and sex-predicted level (hazard ratio=0.87; 95%CI, 0.80-0.93; P <.001). Furthermore, the same authors showed that total survival was longer both in patients with pVO2> 19 and> 15mL/kg/min (men and women, respectively) and in participants with an O2 pulse and values> 13 and> 11mL/beat (men and women, respectively). In 43 patients with asymptomatic severe AS, Levy et al.5 found that the best cutoff for pVO2 was 14mL/kg/min. Patients with values below this cutoff had more events during follow-up.
The pulmonary response variables determined by CPET include the slope consisting of the quotient between minute ventilation and CO2 production (VE/VCO2 slope). This marker of ventilatory efficiency has greater prognostic value for the appearance of cardiovascular events in patients with heart failure, and its prognostic value has been similar, and even higher in some studies, to that of pVO2.7 Several studies have shown that this variable also has prognostic value in severe AS.5,7,13 For instance, studies by our group have shown that VE/VCO2 slope> 31.19 was predictive of combined event (heart failure, syncope, and mortality) at 6 months of follow-up in asymptomatic patients with severe AS.13
Multiple studies have evaluated early aortic valve replacement in asymptomatic patients. In 2020, the RECOVERY trial3 reported that patients treated by this method had lower cardiovascular mortality than those in the conservative treatment arm. Additionally, the AVATAR trial6 showed that patients with asymptomatic severe AS treated by aortic valve replacement had a lower primary composite endpoint (all-cause death, acute myocardial infarction, stroke, or hospitalization due to heart failure) than the control group. Banovic et al.6 performed conventional exercise tests in all of these patients but did not use the CPET in their study due to the heterogeneity of the various sites involved, which could have led to patients being falsely identified as asymptomatic, due to the limitations of this technique. Likewise, recent data have revealed that young patients (between age 50 and 65 years) with asymptomatic severe AS treated with aortic valve replacement do not regain a similar life expectancy to that of the general population.14,15 Therefore, the utmost caution is needed when deciding on aortic valve replacement in certain patients or in patients with certain comorbidities because survival or quality of life may be poorer than expected.
Based on current data, our group proposes that patients with asymptomatic severe AS and a normal CPET could undergo regular follow-up with no risk of major events. Nevertheless, we believe that patients with pathologic age- and sex-predicted pVO2 and VE/CO2 slope are at an increased risk of events and, therefore, these parameters may aid therapeutic decisions, as proposed in the algorithm depicted in figure 1. Omitting the CPET from the clinical guidelines for these patients could deprive health care professionals of useful information when evaluating the prognosis and treatment of patients with AS.8 The CPET includes a series of parameters offering information to assess, from a general viewpoint, the behavior of the cardiovascular, respiratory, and metabolic energy systems. Consequently, for patients with “asymptomatic” severe AS, a baseline test should be considered, in order to determine the patient's actual functional capacity as objectively as possible. The technique is not very costly, time-consuming, or cumbersome, as it only requires a reasonable learning curve and a thorough understanding of cardiovascular pathophysiology. In conclusion, CPET is an essential decision-making instrument for patients with AS.
This article has received no funding.
CONFLICTS OF INTERESTP. Avanzas is associate editor of Revista Española de Cardiología; the editorial procedure established by the journal has been followed to ensure impartial management of the manuscript. The authors declare no conflicts of interest.