The exponential increase in coronary interventions plus the generalization of the radial approach represent the ideal scenario for starting outpatient angioplasty programs with the aim of reducing the costs while maintaining safety. This article reports data from a multicenter Spanish registry on fully ambulatory transradial angioplasty in selected patients for the first time.
MethodsProspective registry of elective outpatient transradial-ulnar angioplasty in patients with stable coronary disease. Patients were discharged the same day and were followed up at 24hours and 30 days. Safety and feasibility were analyzed.
ResultsOf the 723 patients included (76% male; age, 66.6±10.5 years), 533 (73.7%) were finally discharged after 4 to 12hours of surveillance. Among the remaining 190 (26.7%) patients, the most common reason for hospitalization was clinical instability after the procedure (60.5%). Independent predictors of admission were a history of peripheral artery disease, a higher baseline creatinine level, ad hoc performance of the procedure, and multivessel disease. At 24hours, there was 1 major adverse event in 1 patient (0.19%), who required hospitalization for major bleeding not related to vascular access. At 30 days, there were 3 major adverse events (0.56%): 1 subacute stent thrombosis, 1 revascularization of a vessel other than the treated vessel, and 1 minor stroke. Eight patients (1.5%) required admission at 30 days.
ConclusionsThe application of an outpatient transradial-ulnar angioplasty program with discharge after 4 to 12 hours’ surveillance is safe and feasible in well-selected patients.
Keywords
During 2014, more than 67 000 percutaneous coronary intervention (PCI) procedures were performed, with an upward trend over the last decade.1 Most hospitals routinely admit patients for at least 1 night after PCI, and thus the activity of cardiac catheterization laboratories places a burden on the few hospital beds available, which results in increased costs per procedure. Similarly, the availability of beds can influence the waiting list for PCI for many patients. However, about 75% of these procedures were performed outside the setting of ST-segment elevation acute myocardial infarction. There is also a clear trend toward the use of radial access in most Spanish hospitals (75% of procedures),1 with the support of increasingly experienced operators. If to this is added the availability and better utilization of more effective antithrombotic therapies and improvements in materials and devices, it is now possible to safely implement PCI programs with same-day discharge. This strategy has been mainly studied in European and North American hospitals since the mid-1990s2 using different designs, vascular access, settings, and types of patients. Several observational3,4 and randomized5,6 studies have shown good results.
However, the results of Spanish early discharge programs after PCI have not yet been reported. This article presents the results of a prospective multicenter registry which assessed the short-term and 30-day safety of same-day outpatient PCI in selected patients.
METHODSDesignA prospective multicenter registry was performed in the setting of standard clinical practice with the participation of 3 tertiary centers with extensive experience in radial access, understood as 85% or more of the procedures being performed via this access route per year. Each center had implemented a PCI outpatient program. The registry included patients undergoing outpatient PCI between January 2013 and September 2015 in each participating hospital. Patient data from each center were included in a shared database. The researchers from each participating hospital prospectively reviewed clinical events. The ethics committee of the hospital that sponsored the registry evaluated and approved the study and performed data analysis. All patients were informed of their inclusion in the study.
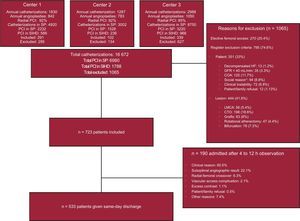
Study PopulationTable 1 shows the registry inclusion and exclusion criteria. All patients meeting these criteria were eligible for same-day discharge. Table 1 also shows the criteria for admission after PCI. Patients who were admitted formed a second analysis group to characterize the reasons for and predictors of admission. The main study group comprised patients who underwent same-day admission and discharge after 4 to 12hours of surveillance according to the protocol and standard practice of each center. All patients underwent elective PCI (scheduled or ad hoc) using radial or ulnar access for stable coronary disease of 1 or more vessels. Before PCI, all patients should receive antiplatelet therapy with at least aspirin and clopidogrel or another P2Y12 inhibitor and could receive the loading dose of the second antiplatelet agent in the cardiac catheterization laboratory. Medical staff reassessed the patients before discharge and by telephone or in person at 24 hours and 30 days. If there were vascular access complications (hematoma), the patients were reassessed in person. The computerized medical records of each patient were also reviewed in the event of complications or prespecified adverse events. Figure shows the study flow chart.
The Registry Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Chronic ischemic heart disease: stable angina or silent ischemia Elective PCI (scheduled/ad hoc) Intention to use radial-ulnar access | Patient Symptomatic decompensated HF GFR<40 mL/min Chronic oral anticoagulation Absence of caregiver at home, inability to understand the procedure, or home far from health resources (>60min) Clinical instability Patient or family refusal |
| Lesion-procedure Procedure on LMCA CTO Procedure Aortocoronary graft procedure Procedure with rotational atherectomy Complex procedure in bifurcation Elective femoral access |
| Admission criteria after PCI | |
|---|---|
| Clinical instability after PCI: persistent chest pain, HF, arrhythmias, syncope Complication during PCI Patient or family refusal Radial-to-femoral crossover Acute occlusion of main vessel or secondary branch>1 mm Residual dissection No reflow/final TIMI<3 Perforation Residual thrombus Major complication with vascular access (no mild or moderate hematomas) Use of contrast>400 mL |
CTO, chronic total occlusion; GFR, glomerular filtration rate; HF, heart failure; LMCA, left main coronary artery; PCI, percutaneous coronary intervention; TIMI, Thrombolisis in Myocardial Infarction.
Study flow chart. COA, chronic oral anticoagulation; CTO, chronic total occlusion; GFR, glomerular filtration rate; HF, heart failure; LMCA, left main coronary artery; PCI, percutaneous coronary intervention; SIHD, stable ischemic heart disease; SP, study period. * Absence of caregiver at home, inability to understand the procedure, or home far from health resources (>60min).
The main aim of the study was to assess feasibility and short-term safety from the end of the procedure to discharge and at 24hours and 30 days.
FeasibilityThe percentage success rate of PCI was calculated to assess the feasibility of outpatient PCI in selected patients. Success was defined as the absence of complications with optimal angiographic outcomes and periprocedural and postprocedural clinical stability during the observation period. This definition corresponded to the percentage of patients who were finally discharged after their being eligible for inclusion in the registry.
SafetyAny complications were recorded before discharge, at 24 hours, and at 30 days. Major complications and minor complications were analyzed separately:
- •
Major cardiovascular adverse events: these included the following aspects as major complications, as defined by the recommendations of the Academic Research Consortium (ARC).7
- –
Death: all-cause mortality.
- –
Q-wave or non–Q-wave acute myocardial infarction: periprocedural acute myocardial infarction and spontaneous acute myocardial infarction, defined as elevated troponin levels more than 3 times the normal upper limit or more than the normal upper limit respectively, the appearance of new Q waves, left bundle branch block, ST-segment elevation or dynamic changes of the ST/T wave segment, and typical symptoms of myocardial ischemia. Sudden cardiac death prior to the determination of biomarkers is also included in this section.
- –
Stent thrombosis: definite, probable, and possible.
- –
Need for repeat revascularization of the target lesion: guided or not by the clinical picture with a repeat PCI procedure or surgery.
- –
Need for repeat revascularization of the target vessel: guided or not by the clinical picture, with a repeat PCI procedure or surgery in the same target vessel before or after the 5mm proximal or distal to the target lesion.
- –
Need for repeat revascularization of another vessel: ischemia-guided or not in a vessel other than the target vessel, providing this procedure is not part of the scheduled procedure.
- –
Major bleeding: defined according to the Bleeding Academic Research Consortium (BARC 3 or 5).8
- –
Stroke: transient ischemic attack or ischemic/hemorrhagic stroke defined as a general or focal transient or persistent neurological abnormality resulting from brain, spinal cord, or retinal vascular damage.
- –
Contrast-induced kidney failure needing admission or treatment with renal support techniques.
- –
Vascular access complications requiring surgical treatment or admission or involving major bleeding.
- –
- •
Minor complications were those related to vascular access not requiring admission or surgical treatment and not involving major bleeding. Hematomas were classified according to the EASY classification.9
Within the aim of safety, the need for urgent care and admission were recorded.
Other DefinitionsElective outpatient PCI: scheduled outpatient procedure or immediately after diagnosis (ad hoc), with discharge within 12 hours after an observation period.
Seven analysis groups were established to assess reasons for admission: suboptimal angiographic result, clinical instability (eg, angina, periprocedural complications, recurrent chest pain, arrhythmias, syncope), patient or family refusal, vascular access complications, radial-to-femoral crossover, excess of contrast agent (> 300mL), and miscellaneous other reasons.
Statistical AnalysisQualitative variables are expressed as frequency and percentage and were analyzed using the parametric chi-square test or the Fisher exact test (nonparametric) when needed according to the distribution of the variable analyzed. Quantitative variables are expressed as mean ± standard deviation or median [interquartile range] according to the distribution of the variable. The normality of the distribution of the variables was assessed using the Kolmogorov-Smirnov test and they were compared using the Student t test. The medians of time were analyzed using the nonparametric Mann-Whitney U test. A P value of < 0.05 was used as a cutoff for statistical significance for a 95% confidence interval (95%CI). Variables associated with admission were determined using univariable analysis. Independent predictors of admission were identified using logistic regression analysis, after the inclusion of variables with a P value < 0.1 in the univariable analysis. All analyses were conducted using the SPSS 17.0 software package for Windows (SPSS Inc., Chicago, Illinois, United States).
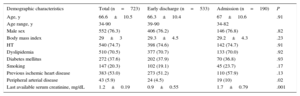
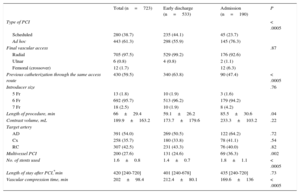
RESULTSPatients and ProcedureTable 2 shows the baseline characteristics of the 723 patients finally included in the study and their comparison according to early discharge or admission. The mean age of the population was 66.6±10.5 years, 76% were male, and there was a high percentage of diabetes (37.5%). The most frequent characteristics of the patients were a history of peripheral artery disease and a high baseline creatinine level. Table 3 shows the procedural characteristics. Patients were admitted more frequently after unscheduled procedures, longer and more complex procedures, or those requiring multivessel revascularization.
Baseline Characteristics and Comparison Between Early Discharge Group and Patients Requiring Admission
| Demographic characteristics | Total (n=723) | Early discharge (n=533) | Admission (n=190) | P |
|---|---|---|---|---|
| Age, y | 66.6±10.5 | 66.3±10.4 | 67±10.6 | .91 |
| Age range, y | 34-90 | 39-90 | 34-82 | |
| Male sex | 552 (76.3) | 406 (76.2) | 146 (76.8) | .82 |
| Body mass index | 29±3 | 29.3±4.5 | 29.2±4.3 | .23 |
| HT | 540 (74.7) | 398 (74.6) | 142 (74.7) | .91 |
| Dyslipidemia | 510 (70.5) | 377 (70.7) | 133 (70.0) | .92 |
| Diabetes mellitus | 272 (37.6) | 202 (37.9) | 70 (36.8) | .93 |
| Smoking | 147 (20.3) | 102 (19.1) | 45 (23.7) | .17 |
| Previous ischemic heart disease | 383 (53.0) | 273 (51.2) | 110 (57.9) | .13 |
| Peripheral arterial disease | 43 (5.9) | 24 (4.5) | 19 (10) | .02 |
| Last available serum creatinine, mg/dL | 1.2±0.19 | 0.9±0.55 | 1.7±0.79 | .001 |
HT, hypertension.
Values are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Procedural Characteristics
| Total (n=723) | Early discharge (n=533) | Admission (n=190) | P | |
|---|---|---|---|---|
| Type of PCI | < .0005 | |||
| Scheduled | 280 (38.7) | 235 (44.1) | 45 (23.7) | |
| Ad hoc | 443 (61.3) | 298 (55.9) | 145 (76.3) | |
| Final vascular access | .87 | |||
| Radial | 705 (97.5) | 529 (99.2) | 176 (92.6) | |
| Ulnar | 6 (0.8) | 4 (0.8) | 2 (1.1) | |
| Femoral (crossover) | 12 (1.7) | 12 (6.3) | ||
| Previous catheterization through the same access route | 430 (59.5) | 340 (63.8) | 90 (47.4) | < .0005 |
| Introducer size | .76 | |||
| 5 Fr | 13 (1.8) | 10 (1.9) | 3 (1.6) | |
| 6 Fr | 692 (95.7) | 513 (96.2) | 179 (94.2) | |
| 7 Fr | 18 (2.5) | 10 (1.9) | 8 (4.2) | |
| Length of procedure, min | 66±29.4 | 59.1±26.2 | 85.5±30.6 | .04 |
| Contrast volume, mL | 189.9±163.2 | 173.7±179.6 | 233.3±103.2 | .22 |
| Target artery | ||||
| AD | 391 (54.0) | 269 (50.5) | 122 (64.2) | .72 |
| Cx | 258 (35.7) | 180 (33.8) | 78 (41.1) | .54 |
| RC | 307 (42.5) | 231 (43.3) | 76 (40.0) | .82 |
| Multivessel PCI | 200 (27.6) | 131 (24.6) | 69 (36.3) | .002 |
| No. of stents used | 1.6±0.8 | 1.4±0.7 | 1.8±1.1 | < .0005 |
| Length of stay after PCI,*min | 420 [240-720] | 401 [240-678] | 435 [240-720] | .73 |
| Vascular compression time, min | 202±98.4 | 212.4±80.1 | 169.6±136 | < .0005 |
AD, anterior descending artery; Cx, circumflex artery; PCI, percutaneous coronary intervention; RC, right coronary.
Values are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
During the study period, a total of 16 672 cardiac catheterization procedures and 6980 PCI procedures were performed in 3 hospitals, 1788 (25.6%) of which were performed in the setting of stable ischemic heart disease. In total, 40.5% of these patients met the inclusion criteria. A total of 190 (26.3%) patients were admitted after PCI. Of the 533 (73.7%) patients who were discharged home, 128 (23.6%) lived in a municipality without a hospital. In predischarge assessment, 8 patients (1.5%) had vascular complications without need for admission; 7 with moderate hematoma and 1 with radial occlusion at discharge without digital ischemia.
The Figure shows the different reasons for admission and the percentage of patients admitted for each one. Median length of stay was 1 [1-2] days.
Univariable analysis showed that predictors of admission were peripheral vascular disease, high baseline creatinine levels, and ad hoc multivessel procedures. Multivariable analysis showed that these variables were also independent predictors of admission. However, a history of previous catheterization using the same access route was a protective factor (Table 4).
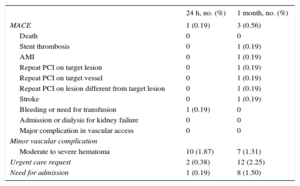
Events and Complications After 24Hours and 1 Month (n=533) of Follow-up
| 24 h, no. (%) | 1 month, no. (%) | |
|---|---|---|
| MACE | 1 (0.19) | 3 (0.56) |
| Death | 0 | 0 |
| Stent thrombosis | 0 | 1 (0.19) |
| AMI | 0 | 1 (0.19) |
| Repeat PCI on target lesion | 0 | 1 (0.19) |
| Repeat PCI on target vessel | 0 | 1 (0.19) |
| Repeat PCI on lesion different from target lesion | 0 | 1 (0.19) |
| Stroke | 0 | 1 (0.19) |
| Bleeding or need for transfusion | 1 (0.19) | 0 |
| Admission or dialysis for kidney failure | 0 | 0 |
| Major complication in vascular access | 0 | 0 |
| Minor vascular complication | ||
| Moderate to severe hematoma | 10 (1.87) | 7 (1.31) |
| Urgent care request | 2 (0.38) | 12 (2.25) |
| Need for admission | 1 (0.19) | 8 (1.50) |
AMI, acute myocardial infarction; MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention.
Table 5 shows clinical events and recorded complications. The primary safety endpoint (major adverse cardiovascular events) was reached in 0.19% of patients at 24hours and in 0.57% at 30 days. No deaths were recorded at 24hours or at 30 days. At 24hours, 1 patient needed readmission (major bleeding unrelated to vascular access, due to a 4g/dL decrease in hemoglobin caused by rectal bleeding) and 2 needed medical care in the emergency room. Both patients had chest pain, which ruled out an ischemic origin. At 30 days, 8 patients were readmitted and another 12 were treated in the emergency room. Three major adverse cardiovascular events were recorded: 1 patient had a definite subacute stent thrombosis that developed into non—ST-segment acute myocardial infarction, 1 patient had unstable angina that needed PCI on a vessel other than the target vessel, and 1 patient had a minor stroke 5 days after PCI. The other patients admitted at 30 days did not need another angiographic reassessment and were admitted for various reasons such as chest pain or decompensated heart failure. Regarding minor complications, 1.8% of hematomas were recorded at 24hours and 1.3% at 30 days, without the need for surgical intervention or admission and without major bleeding.
Predictors of Admission after PCI in Patients Initially Selected for Outpatient PCI
| Univariable analysis | |||
|---|---|---|---|
| Variable | Relative risk | 95%IC | P |
| Peripheral artery disease | 1.67 | 1.15–2.43 | .014 |
| Last serum creatinine level | 1.72 | 1.22–2.41 | .002 |
| Multivessel PCI | 1.49 | 1.16–1.92 | .001 |
| Ad hoc PCI | 2.28 | 1.54–3.37 | .0001 |
| Previous catheterization through the same access route | 0.61 | 0.48–0.79 | .0001 |
| Multivariable analysis | |||
|---|---|---|---|
| Variable | Odds ratio | 95%CI | P |
| Peripheral artery disease | 2.16 | 1.15–4.10 | .023 |
| Last serum creatinine level | 1.88 | 1.32–2.68 | .002 |
| Multivessel PCI | 1.75 | 1.22–2.49 | .002 |
| Ad hoc PCI | 3.98 | 1.65–9.61 | .002 |
| Previous catheterization through same access route | 0.51 | 0.37–0.72 | .0001 |
95%CI, 95% confidence interval; PCI, percutaneous coronary intervention.
This article reports data from a Spanish multicenter registry on the safety of outpatient PCI programs for the first time. The sample size was one of the largest published to date. Previous studies included patients admitted 24hours before the procedure; in this registry, patients were admitted and discharged the same day. The results clearly demonstrate the safety and feasibility of outpatient transradial PCI in well-selected patients, with a major adverse cardiovascular event rate of 0.19% at 24hours and with 74% of eligible patients being discharged.
Scope and Safety of Outpatient Percutaneous Coronary InterventionCurrently, a vast number of medical and surgical procedures are safely performed on an outpatient basis.10 It should be noted that an overnight stay in hospital is associated with a 0.5% risk of an adverse drug reaction or up to a 1.6% risk of infection.11 In 2009, the Society of Cardiovascular Angiography and Interventions/American College of Cardiology published a consensus document12 which established the recommendations for outpatient PCI. Similar criteria were used in this registry. However, there are no recommendations in the European revascularization guidelines.13
Patients with stable ischemic heart disease account for more than 25% of the activity of cardiac catheterization laboratories: of these, up to 40.5% could benefit from the application of the type of outpatient PCI programs described above. The data also show that most of the eligible patients (74%) are discharged. In total, PCI procedures comprise around 10% of all cardiac catheterization laboratory activity, which in numerical terms represents an increase in the availability of beds and can produce overall cost savings without compromising patient safety.14,15
The feasibility of outpatient PCI is determined by ischemic and hemorrhagic risk factors.
Although the risk of ischemic complications appears to be more closely associated with procedural outcomes than with the type of target lesion and target vessel,16,17 acute stent thrombosis, which is probably the most dreaded complication, is clearly associated with various factors such as acute coronary syndrome or PCI in complex lesions.18–20 Some studies have included patients with acute coronary syndrome21 (25% in the EASY study22), with a higher rate of major adverse cardiovascular events than the total rate. However, complex lesions were not included in previous studies. Future research could address outpatient PCI for more complex lesions, given the current improvements in materials and increasingly experienced operators.
Hemorrhagic risk mainly depends on the vascular access route. In this regard, radial access is clearly superior to femoral access.24,25 The EPOS study26 found a vascular complications rate of 6.1% within 24 hours in patients discharged the same day after transfemoral PCI using manual compression for hemostasis. Similarly, although the largest registry of same-day discharge after PCI (98% femoral access)27 found a low rate of vascular complications, the rate was 3 times higher in discharged patients (0.75% vs 0.25%, P< .001) despite vascular closure devices being used more frequently in this group and being used in more than 50% of patients in both groups. Although the systematic use of vascular closure devices can reduce complications (0.8% in the study by Antonsen et al.28), it also increases costs. No major vascular complications were recorded in the present registry. The only documented major bleeding episode was unrelated to vascular access. Approximately 1.5% of patients had hematomas > 5cm, all of which were superficial and did not need treatment other than standard compression bandages and local measures. The low event rate is in line with the findings of previously published studies and meta-analyses,21,23,27 in which the rate was around 1% at 24 hours and 30 days.21
Regarding length of stay after PCI, major complications usually occur within 4 to 6 hours or 24 hours after the procedure.16 Thus, careful patient selection after 4 to 12 hours of surveillance, possibly in dedicated “radial lounge”,29 appears to be both sufficient and safe.
Finally, when these programs are implemented, certain comorbidities should be taken into account, such as chronic kidney failure, severe left systolic ventricular dysfunction, or oral anticoagulation therapy, as well as certain social conditions, such as distance to a hospital with emergency services and family or caregiver support in the first 24 hours after PCI.
LimitationsSeveral limitations of this registry should be taken into account. On the one hand, the data were obtained from 3 hospitals each with their own outpatient PCI programs, rather than having a program in common. On the other hand, common inclusion and exclusion criteria were established for the registry. In addition, data from the 3 hospitals were collected in a shared database. Because we did not conduct a systematic survey of patient acceptance and opinion, it cannot be concluded from this study that outpatient PCI is more comfortable for patients, although previous studies15 have confirmed their acceptance. Patient follow-up was not always conducted in person; thus, some vascular complications, although not severe ones, may have been underestimated. The potential intervention bias inherent to prospective registries is another limitation. Finally, although a cost analysis was not conducted, previous studies suggest savings of up to 50% per procedure.14
CONCLUSIONSOutpatient PCI using radial-ulnar access with discharge after 4 to 12hours of surveillance is reliable and safe in well-selected patients. In Spain, the current exponential increase in PCI in general and the increased use of radial access makes the application of these programs potentially available to most of the patients with stable ischemic heart disease and could reduce waiting times and costs per procedure.
- –
Some trials and several registries have previously reported favorable safety data on same-day PCI using radial and femoral access, as well as in different clinical situations and within very heterogeneous programs.
- –
These programs, however, are not widely implemented in Europe.
- –
This article reports data from a multicenter Spanish registry on the safety of fully ambulatory same-day PCI programs for the first time.
- –
The registry included “truly” ambulatory patients, in the sense that the patients were admitted for PCI and discharged the same day. The sample size was one of the largest published to date and used contemporary data.
- –
Safety was demonstrated. The objective is to promote this practice in Spain.
The authors wish to thank the nursing staff of the participating cardiac catheterization and interventional cardiology units for their excellent work in patient care and their invaluable help in data collection.
CONFLICTS OF INTERESTNone declared.