Transfemoral access is the most frequently used vascular approach in chronic total occlusion percutaneous coronary interventions (CTO-PCI). The aim of this study was to evaluate the safety and feasibility of a transradial access CTO-PCI program and its impact on angiographic and clinical results and length of hospital stay.
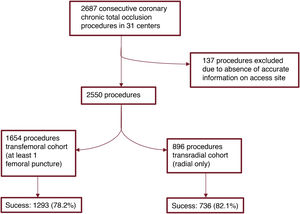
MethodsRetrospective multicenter cohort study including 2550 consecutive CTO-PCI procedures included in a multicenter registry with accurate information on vascular access. A total of 896 procedures were performed as radial-only access while 1654 were performed through at least 1 femoral puncture. Clinical and angiographic data were collected.
ResultsThe mean age was 66.3± 11.4 years. The mean Japan-chronic total occlusion score (2.7±0.3) was similar in the 2 groups. Successful revascularization was achieved in 2009 (79.6%) cases, 78.2% and 82.1% in the femoral and radial access cohorts, respectively (P=.002). Periprocedural in-hospital complications were observed in 5.1% and 2.3% (P=.02), with fewer access site-dependant vascular complications in the transradial cohort (2.3% vs 0.2%; P=.009). The mean length of hospital stay was significantly shorter in the transradial access group (0.89±1.4 vs 2.2±3.2 days, P<.001).
ConclusionsA transradial program for CTO-PCI is safe and effective in most CTO lesions. The transradial strategy has fewer vascular complications and shorter length of hospital stay without compromising the success rate.
Keywords
Chronic total occlusions (CTO) are one of the most challenging scenarios in percutaneous coronary intervention (PCI).1 Currently, transfemoral access is the most frequently used vascular approach in CTO-PCI,2–4 as it enables use of larger-bore guiding catheters and increases backup support and maneuverability.
The development of new materials and techniques over the past few years has substantially improved the efficacy of CTO-PCI5,6 and contemporary registries report success rates of more than 80%, mainly employing transfemoral access.7,8
The adoption of a transradial approach in CTO-PCI is progressively gaining attention as it provides comparable success rates in more simple lesions, while significantly reducing bleeding and access site complications.4,9,10 Compared with transfemoral access, transradial PCI allows early ambulation, facilitates same-day hospital discharge, and has been linked to greater cost reduction.11–13 However, consistent data on the outpatient management of patients undergoing transradial CTO-PCI are currently lacking.
The aim of our study was to evaluate the safety and feasibility of a transradial access PCI program in CTO and its impact on length of hospital stay and same-day hospital discharge.
METHODSFrom January 2015, a prospective registry of CTO-PCI procedures was created through the Iberian registry, including 31 hospitals in 2 different European countries and endorsed by the Spanish Association of Interventional Cardiology and the Spanish Society of Cardiology. The Iberian CTO Registry was approved by the Ethics Committee of Valladolid-Este Health Area. Each hospital entered the data using an online platform. Informed consent for this study was not needed as all data were properly anonymized, complying with the requirements of the Law on Data Protection, and were accessible only to participating operators and registry coordinators. Informed consent for procedures was always obtained before CTO-PCI.
Between January 2015 and March 2021, 2687 percutaneous CTO revascularization procedures were consecutively included. The criteria for CTO-PCI were similar among participants and required the presence of viability in the corresponding myocardial segments and at least 1 of the following: inducible ischemia, clinically symptomatic angina, or occlusion of a proximal coronary vessel associated with left ventricular systolic dysfunction.
Accurate information on vascular access was assessed and 2 cohorts were compared according to the presence or absence of at least 1 femoral puncture. Hence, the radial cohort was composed of the addition of 1 radial or 2 radial access procedures and the femoral cohort included 1 femoral, 2 femoral or 1 femoral and 1 radial access procedures. Vascular access was performed by physician preferences following their own local protocols.
A total of 2550 procedures were recorded with accurate access site information, consisting of 896 procedures included in the transradial cohort and 1654 in the transfemoral cohort (figure 1).
Definitions and outcomesA CTO lesion was defined as an obstruction of a native coronary artery with TIMI flow grade 0 for an estimated duration of more than 3 months.14
Successful percutaneous revascularization was defined as final residual stenosis<20% and TIMI flow grade ≥ 2 after stent implantation based on visual evaluation of angiograms.
Primary safety endpoints included periprocedural and in-hospital complications (death, myocardial infarction, stent thrombosis, need for urgent revascularization, cardiac tamponade, stroke, contrast-induced nephropathy, and vascular site complications). Vascular access site complications were recorded only if considered major, defined as those requiring surgery, percutaneous treatment, or blood transfusion. Vascular site hematoma was not considered as a vascular site complication if no intervention was required. Contrast-induced nephropathy, periprocedural type-IV myocardial infarction and stent thrombosis were defined as per guidelines.15–17
Major adverse cardiac events were defined as the combination of all-cause mortality, myocardial infarction, stroke, and revascularization. Rehospitalization at 24hours and 30 days and major adverse cardiac events at 30 days were recorded. Additional safety endpoints included the volume of contrast media employed, fluoroscopy time, and radiation exposure.
Statistical analysisCategorical variables are expressed as frequencies and percentages and continuous variables as mean±standard deviation. Chi-square tests or Fisher exact tests were used as appropriate to compare categorical variables between the 2 groups, while the Student t-test was used to compare continuous variables. Statistical significance was established at a P value <.05 and all test were 2-tailed. Multivariate analysis was performed by logistic regression modelling and propensity score derived from the model. Statistical analyses were performed with JMP 9.0 from SAS Institute and R 4.1.3 from The R Foundation for propensity score.
The study protocol was approved by the Institutional Review Board, which complied with the Helsinki Declaration.
RESULTSBaseline characteristicsBetween January 2015 and March 2021, 2687 percutaneous CTO revascularization procedures were performed in 2360 patients and were consecutively included in the registry. After selection of all the procedures with accurate information on the access-site, 2550 interventions were included in the final analysis. Baseline clinical characteristics are displayed in table 1. Mean age was 66.3±11.4 years. Patients in the radial cohort had a lower proportion of male sex, a higher rate of diabetes mellitus and a lower rate of previous coronary interventions, both percutaneous and surgical, and presented more frequently with CCS grade III-IV angina.
Baseline clinical characteristics
| Characteristic | Global (n=2550) | Femoral (n=1654) | Radial (n=896) | P |
|---|---|---|---|---|
| Age | 66.3±11.4 | 66.8±11.5 | 64.2±11.1 | .2 |
| Male sex | 2040 (80.0) | 1384 (83.7) | 655 (73.1) | <.001 |
| Hypertension | 1754 (68.8) | 1140 (68.9) | 614 (68.6) | .4 |
| Diabetes mellitus | 734 (28.8) | 444 (26.8) | 290 (32.3) | .0059 |
| Dyslipidaemia | 1701 (66.7) | 1116 (67.5) | 581 (64.8) | .18 |
| Smoking | 1050 (41.2) | 696 (42.1) | 114 (39.6) | .3 |
| CKD | 291 (11.4) | 164 (10.7) | 84 (12.7) | .12 |
| Peripheral arteriopathy | 248 (9.7) | 164 (9.9) | 84 (9.4) | .37 |
| Stroke | 143 (5.6) | 95 (5.7) | 47 (5.3) | .8 |
| LVEF, % | 50.7±16 | 50.2±4 | 51.8±6 | .03 |
| Previous CABG | 156 (6.1) | 121 (7.3) | 35 (3.9) | <.001 |
| Previous PCI | 1279 (50.2) | 898 (54.3) | 381 (42.5) | <.001 |
| Previous MI | 752 (29.5) | 486 (29.4) | 266 (29.7) | .09 |
| Symptoms | ||||
| No symptoms | 334 (13.1) | 233 (14.1) | 101 (11.3) | .002 |
| CCS class I-II | 1410 (55.3) | 935 (56.5) | 475 (53.0) | |
| CCS class III-IV | 806 (31.6) | 486 (29.4) | 320 (35.7) | |
| Inducible ischemia | 1155 (45.3) | 780 (47.1) | 375 (41.8) | .03 |
CCS, Canadian Cardiovascular Society; CKD, chronic kidney disease, LVEF, left ventricle ejection fraction; CABG, coronary artery bypass grafting; MI, myocardial infarction; PCI, percutaneous coronary intervention.
The data are expressed as No. (%) or mean±standard deviation.
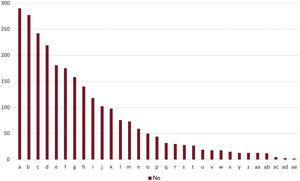
There were clear differences in the volume of cases reported to the registry from the different participant centers. The number of procedures for each center and general study flow chart are summarized in figure 1 and figure 2.
Angiographic characteristicsAngiographic features are displayed in table 2. More than one CTO and previous attempts were more frequent in the transfemoral cohort. In contrast, severe calcification and blunt stump proximal stop were more common in the transradial cohort. There were no significant differences in mean Syntax score (22.2±10.5 vs 21.9±10.9) or mean Japan-chronic total occlusion (J-CTO) score (2.7±0.3 vs 2.7±0.3) between the 2 cohorts. Difficult CTO lesions, identified as J-CTO score> 2, had a similar frequency.
Angiographic characteristics
| Overall | Femoral | Radial | P | |
|---|---|---|---|---|
| (n=2550) | (n=1654) | (n=896) | ||
| Number of vessels | 1.7±0.8 | 1.7 | 1.7 | .9 |
| Multivessel disease | 1451 (56.9) | 941 (56.8) | 510 (56.9) | .9 |
| ≥ 1 CTO | 375 (14.7) | 268 (16.2) | 107 (11.9) | .001 |
| Syntax score | 17 [10-23] | 17 [10-24] | 17 [10-23] | .9 |
| Site | ||||
| LAD | 859 (33.7) | 556 (33.6) | 303 (33.8) | |
| RCA | 1271 (49.8) | 888 (53.7) | 383 (42.8) | .001 |
| LCX | 420 (16.5) | 210 (12.6) | 210 (23.5) | |
| Blunt stump | 1265 (49.6) | 758 (45.8) | 507 (56.6) | .001 |
| CTO length, mm | 24.5±17 | 25.5±18 | 22.9±20 | .003 |
| Severe calcification | 586 (23.0) | 327 (19.4) | 264 (29.3) | <.001 |
| Good distal lumen | 2017 (79.1) | 1275 (77.1) | 739 (82.5) | <.001 |
| Previous attempts | 367 (14.4) | 277 (16.8) | 90 (10.0) | <.001 |
| J-CTO | 2.7±0.3 | 2.7±0.3 | 2.7±0.3 | .9 |
| J-CTO> 2 | 1457 (57.3) | 949 (57.5) | 508 (56.7) | .7 |
CTO: chronic total occlusion; LAD: left anterior descending coronary artery; RCA: right coronary artery; LCX: left circumflex coronary artery.
The data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The right coronary artery was the most frequent CTO location in both groups, followed by the left anterior descending artery. No differences were found in the frequency of left anterior descending coronary artery-sited CTO but right coronary artery and left circumflex coronary artery differed between the cohorts.
Procedural characteristics and outcomesProcedural data are summarized in table 3. Bilateral vascular access was more common in the transfemoral cohort (71.3% vs 27.4%; P <.001), as was the retrograde or hybrid approach. No differences were found in the number or length of stents, and contrast media volume and fluoroscopy time were lower in the transradial cohort.
Procedure details
| Overall | Femoral | Radial | P | |
|---|---|---|---|---|
| (n=2550) | (n=1654) | (n=896) | ||
| Bilateral access | 1425 (55.9) | 1179 (71.3) | 246 (27.4) | <.001 |
| Antegrade approach | 2024 (79.5) | 1202 (72.7) | 822 (91.8) | |
| Retrograde/hybrid approach | 489 (19.2) | 425 (25.7) | (64)7.1 | .004 |
| Antegrade catheter diameter, Fr | 6.8±0.7 | 7.1±0.6 | 6.3±0.5 | <.001 |
| Retrograde catheter diameter, Fr | 6.2±0.8 | 6.3±0.8 | 5.9±0.6 | <.001 |
| IVUS | 512 (20.0) | 392 (23.7) | 120 (13.4) | <.001 |
| Stent length, mm | 48±33 | 49±35 | 47±29 | .4 |
| No. of stents | 1.7±0.9 | 1.7±1 | 1.7±0.9 | .4 |
| Stent diameter | 2.7±0.9 | 2.7±0.4 | 2.8±1.4 | .1 |
| Contrast volume, mL | 252±153 | 263±170 | 231±110 | <.001 |
| Fluoroscopy time | 40±36 | 45±40 | 32±28 | <.001 |
IVUS, intravascular ultrasound.
The data are expressed as No. (%) or mean±standard deviation.
Procedural success was attained in 79.6% of cases overall and was more frequent in the transradial cohort (78.2% vs 82.1%, P=.002). Of note, when more complex cases only were selected by J-CTO score> 2, a trend to a higher success rate was found in the transradial cohort (76.42% vs 79.8%, P=.1) but this difference was not statistically significant (the distribution of J-CTO score and success rate between the 2 cohorts are provided in figure 1 and 2 of the supplementary data). After exclusion of the antegrade approach, among the 489 cases performed by the retrograde or hybrid approach, the procedural success rate dropped to 67.7% but no differences were found between the 2 cohorts (67.9% vs 66.7%, P=.8).
We performed an additional analysis excluding 723 procedures performed via 1 femoral and 1 radial access. The success rate was 78.9% vs 82.1%, P=.08, showing the same tendency in favor of transradial access.
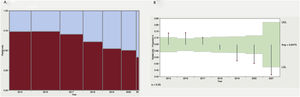
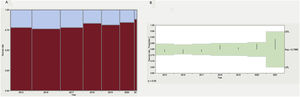
Throughout the study, there was a clear tendency toward an increase in the frequency of transradial access. From 2015 to 2021, the percentage of transradial access increased from 25% of the procedures to 52% and, in parallel, a slight but nonsignificant increase in the success rate was observed. The results by year are summarized in figure 3 and figure 4.
Vascular access selection during the study and success rate. A: proportion of radial-only vs transfemoral access during the study. B: analysis of means for proportions showing a significant tendency to adopt a radial-only strategy during the study. UDL, upper decision limit; LDL, lower decision limit.
Periprocedural complications occurred in 4.1% of patients overall; 5.1% in the transfemoral cohort and 2.3% in the transradial cohort (P <.02). The most common complications were access-site complications (2.3% vs 0.2%; P=.009) and cardiac tamponade (0.7% vs 0.3% P=.4).
To attenuate the imbalance between populations, both regression modelling and propensity score were performed to add statistical value to the analysis. We fitted 2 multivariable logistic regression models with procedural success and vascular complications as outcome variables, and all the clinical and anatomical variables were considered potential modifiers. Transradial access was independently related to a higher success rate (odds ratio [OR], 1.33; 95% confidence interval [95%CI], 1.03-1.72) and produced fewer vascular complications (OR, 0.17; 95%CI, 0.009-0.82). Other predictors for vascular complications were previous coronary artery bypass grafting (CABG) (OR, 3.3; 95%CI, 1.03-9.39) and female sex (OR, 3.9; 95%CI, 1.71-9.03). Predictors for procedure failure were previous PCI (OR, 0.63; 95%CI, 0.51-0.80), previous CABG (OR, 0.63; 95%CI, 0.42-0.96), and female sex (OR, 0.65; CI96%, 0.46-0.91).
We generated a propensity score derived from the regression model, following “full optimal marching” for each procedure in the radial-only cohort to show the effect of vascular access in the treated group. Transradial access was found to be the sole independent predictor of fewer in-hospital vascular complications (OR, 0.22; 95%CI, 0.051-0.978; P=. 047).
Length of stay was significantly lower in the transradial cohort (2.2±3.2 vs 0.89±1.4; P=.03) and same-day regime was possible in 2.2% of cases performed in the transfemoral cohort and 7.4% cases in the transradial cohort (P <.001).
During follow-up, no differences in major adverse cardiac events were found between groups. Death from any cause occurred in 3.1% and 3.7% patients, respectively, and target lesion failure and target vessel failure occurred in 2.1% and 2.8% and 5.8% and 6.7% patients, respectively. Stent thrombosis was recorded in 0.4% cases in the transfemoral cohort and 0.3% cases in the transradial group. Technical and clinical results are summarized in table 4.
Technical and clinical results
| Overall | Femoral | Radial | P | |
|---|---|---|---|---|
| (n=2550) | (n=1654) | (n=896) | ||
| Procedure success | 2029 (79.6) | 1293 (78.2) | 736 (82.1) | .002 |
| In-hospital complications | ||||
| Total | 105 (4.1) | 84 (5.1) | 21 (2.3) | .02 |
| Access site | 40 (1.5) | 38 (2.3) | 2 (0.2) | .009 |
| Cardiac tamponade | 15 (0.6) | 12 (0.7) | 3 (0.3) | .4 |
| Stroke | 19 (0.07) | 19 (1.2) | 0 (0.0) | .8 |
| Length of stay, d | 2.0±2.6 | 2.2±3.2 | 0.89±1.4 | .03 |
| Same-day regimen | 102 (3.8) | 36 (2.2) | 66 (7.4) | <.001 |
| Follow-up | ||||
| Death (any) | 85 (3.5) | 51 (3.1) | 34 (3.7) | .3 |
| MI | 37 (1.5) | 22 (1.3) | 15 (1.7) | .9 |
| TLF | 61 (2.7) | 35 (2.1) | 26 (2.8) | .9 |
| TVF | 156 (6.5) | 96 (5.8) | 60 (6.7) | .4 |
| ST | 10 (0.4) | 7 (0.4) | 3 (0.3) | .5 |
MI, myocardial infarction; TLF, target lesion failure; TVF, target vessel failure; ST, stent thrombosis.
The data are expressed as No. (%) or mean±standard deviation.
The main findings of our study are summarized as follows: first, the transradial approach for CTO-PCI is safe and reduces in-hospital complications and length of stay. Second, transradial access is feasible and allows percutaneous revascularization of complex CTO lesions with no compromise in success rates compared with the transfemoral approach.
Although no differences in Syntax or J-CTO scores were assessed, transradial procedures had a lower rate of previous ICP or CABG, and fewer cases with more than 1 CTO or previous attempts. This suggests that easier cases could be more prone to be scheduled for transradial access a priori (even showing a higher success rate in the transradial cohort), but after we adjusted the analysis according to the predicted difficulty, either by selecting J-CTO>2-only cases or by selecting hybrid or retrograde procedures, we found no difference in the success rate. Another explanation could be that this higher proportion of previous PCI or CABG might not reflect a higher anatomical complexity a priori, but rather a lack of available vascular access, as both transradial PCI and CABG may limit the patency of the radial artery for subsequent procedures.
Currently, transradial PCI represents the vascular access of choice as it consistently improves outcomes across the whole spectrum of CAD.4,9,10,18,19 Nevertheless, CTO-PCI is still frequently performed via the femoral artery in routine clinical practice.
Previous studies have evaluated the feasibility of a transradial approach in CTO-PCI with encouraging results.3,4,9,10 In a single-center experience including 585 patients, Tanaka et al.3 reported similar success rates with either transradial or transfemoral CTO-PCI, although revascularization was less frequently achieved in patients with more complex lesions (J-CTO score> 2) treated via transradial access.
In the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS-CTO),7 although no differences in procedural success rate were observed, transradial procedures showed lower complexity scores than transfemoral procedures. On the other hand, a recent multicenter registry including more than 5000 patients described higher procedural success rates with a transradial vs a transfemoral approach (79.1% vs 75%, P=.001). However, information on lesion complexity was not recorded in that study.2 Technical success was similar for transradial and transfemoral CTO-PCI in 1253 patients in the RECHARGE registry, even in more complex lesions.9 Of importance, access-site selection in these previous studies was made at the operatoŕs discretion, considering the patient́s anatomical and clinical characteristics and so individual bias cannot be excluded.
Very recently, a well-designed controlled clinical trial compared transradial and transfemoral access for CTO-PCI in 616 patients.20 As far as we know, this was the first randomized controlled trial attempting to answer this important question. The results showed no differences in the success rate with fewer vascular complications in the transradial cohort, but in this study, although all procedures were performed by 4 highly experienced operators (with> 100 CTO-PCI per year each), the representation of more complex techniques for CTO-PCI such as hybrid or retrograde approach were underrepresented, and 94% of transradial and 96% of transfemoral procedures were performed via the antegrade approach with antegrade wiring and antegrade dissection and reentry.
Until recently, overnight observation after PCI was the standard of care. However, a same-day discharge strategy is increasingly being adopted worldwide, as it provides comparable safety results and significantly reduces health care-associated costs, while increasing in-patient bed capacity and patient comfort.21–23 Transradial PCI facilitates same-day discharge as it allows early mobilization and reduces the risk of access-site complications. Indeed, substantial cost savings have been described with transradial compared with transfemoral access.11–13 Ambulatory management following PCI has been previously assessed in all-comer populations including patients with complex coronary artery disease.11,24 Previously, few single-center studies had evaluated same-day discharge in CTO-PCI,25,26 but recently, an analysis of the British Cardiovascular Intervention Society evaluating 21 330 patients who underwent CTO-PCI from 2007 to 2014 found transradial access as the main independent factor associated with same-day discharge.27
LimitationsOur study has several limitations. First and most important, the nonrandomized nature of multicenter registries makes validation of the data, at the very least, difficult. Registry inclusion is not mandatory for each intervention, so the inclusion rate and homogeneity of the data were not validated by an external clinical research organization. The data were introduced in each participating center without independent analysis of angiograms in a core laboratory. The transfemoral and transradial approaches were not homogeneously distributed among the whole territory and were very cath lab-dependent. In contrast, these findings represent real life clinical practice but, because real technical difficulty is not always well reflected in complexity scores, more complicated cases may have been performed through femoral access.
Second, there is no record on echo-guidance for femoral puncture, a technique that has proven its efficacy in reducing vascular site complications in transfemoral access.
Third, as transradial access significantly increased during the study period in parallel with the success rate from 2015 to 2021, we cannot exclude the effect of a hypothetical learning curve, even when most of the operators were previously experienced interventional cardiologists. This effect may favor transradial access, as more experienced operators can improve their results after gaining confidence with newer devices and techniques that can facilitate transradial CTO-PCI.
Fourth, information on the reason for admission was not recorded in the study. Most of the CTO-PCI procedures were scheduled in an outpatient regimen, but we cannot exclude significant differences in the proportion of procedures performed during admission for acute coronary syndromes that could eventually lead to longer hospital stay.
Fifth, vascular site complications were not recorded in the study if they did not require percutaneous or surgical repair or blood transfusion, and so we cannot exclude the possible existence of differences in minor vascular site complications.
CONCLUSIONSA transradial approach for CTO-PCI is safe and effective in most CTO lesions and reduces postprocedural complications. The adoption of a transradial protocol for CTO-PCI may have important implications for health care resource management as it shortens the length of hospital stay and enables same-day hospital discharge in an increasing number of elective procedures.
FUNDINGThe REBECO Registry is funded by an unconditional grant from the Spanish Association of Interventional Cardiology and the Spanish Society of Cardiology.
AUTHORS’ CONTRIBUTIONSA. Diego-Nieto, J. Núñez-García and J. Martín-Moreiras designed the study, collected records, and supervised the work overall. A. Diego-Nieto performed the statistical analysis and wrote the first draft of the manuscript. I. Amat-Santos and J.A. Fernández-Díaz coordinate the registry. All authors have performed procedures, recorded data in the registry, and reviewed and approved the final manuscript.
CONFLICTS OF INTERESTI. Amat-Santos is proctor for Boston Scientific, P. Salinas-Sanguino received speaker fees and support for attending meetings from Boston Scientific, Biomenco and Abbott; A. Regueiro received speaker fees from Terumo, Cordis and Boston Scientific and participates on Boston Scientific advisory board; M. Pan received speaker fees from Abbott, Asahi, Boston Scientific and Phillips; N. Gonzalo receives a research grant, speaker and consulting fees from Abbott Vascular and speaker fees from Boston Scientific; A. Jurado-Román receives speaker fees from Biomenco and Boston Scientific; M. Sabaté received consulting fees from Abbott Vascular and iVascular; S. Ojeda received consulting fees from WorldMedical, Edwards Lifesciences and Medtronic and speaker fees from Abbott Vascular, Boston Scientific, Terumo and Phillips, and participates on Medtronic and Edwards Lifesciences advisory boards; J. Sanchis received speaker fees from Biotronik, Abbott Vascular and Boston Scientific; J. Escaned received speaker fees from Abbott, Boston Scientific and Phillips, and participates on Boston and Phillips advisory boards; J. Martín-Moreiras is proctor for Boston Scientific, World Medica and Teleflex. None of the remaining authors declare conflicts of interest.
J. Sanchis is the Editor-in-Chief of Revista Española de Cardiología; the journal's editorial procedures have been followed to guarantee impartial handling of the manuscript.
- -
Although the radial artery is the vascular access of choice for the immense majority of PCI, CTO-PCI are commonly performed via the femoral artery due to its inherent difficulty and the need for large bore catheters. Data on the effectiveness of transradial CTO-PCI in different contexts are scarce.
- -
Transradial CTO-PCI is not only feasible but is also related to fewer in-hospital complications and shorter length of stay without lowering the effectiveness rate, even in anatomically complex cases. Radial access might become the vascular access of choice for most CTO-PCI procedures.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2022.05.019