Recent randomized trials of the MitraClip system have reported controversial results in the treatment of patients with functional mitral regurgitation (FMR). The aim of the present study was to evaluate the safety and impact of MitraClip implantation on outcomes in FMR according to left ventricular (LV) status.
MethodsPatients with FMR undergoing MitraClip implantation in our center were retrospectively screened and divided into 2 groups according to LV ejection fraction (LVEF) and LV end-diastolic dimension: “very poor LV” (LVEF ≤ 20% and/or LV end-diastolic dimension ≥ 70 mm) and “poor LV” (LVEF> 20% and LV end-diastolic dimension <70 mm). Survival analysis of cardiovascular outcomes included hospital admission due to congestive heart failure, heart transplant, and cardiovascular death. Likewise, we compared the number of hospital admissions and functional class the year before and after the intervention.
ResultsFifty-eight consecutive patients with FMR were included (28 with very poor LV and 30 with poor LV). The mean follow-up was 19.5± 13 months. Patients with poor LV showed a significantly better event-free survival for cardiovascular events (log-rank 3.706, P=.010). One year after the intervention, both groups showed symptom improvement. Most of the patients were in New York Heart Association functional class I-II (100% poor LV and 84% very poor LV) and both groups showed a decrease in the number of hospital admissions due to congestive heart failure.
ConclusionsMitraClip implantation seems to be safe and effective in reducing FMR. Although patients with very low LVEF and/or very enlarged LV seemed to have worse cardiovascular outcomes, the intervention was safe and resulted in symptom improvement.
Keywords
Secondary or functional mitral regurgitation (FMR) due to left ventricular (LV) remodeling and dysfunction is present in up to one third of patients with mitral regurgitation (MR) and is the most prevalent valve disease in the general population.1,2 Despite the good results of mitral valve surgery for the treatment of patients with primary MR,3 its role in patients with isolated secondary or FMR is controversial (Class IIb recommendation).3 Percutaneous mitral valve repair with the MitraClip system is an alternative for those patients with symptomatic MR and high surgical risk. In Spain, the number of patients with MitraClip implantation is increasing, with FMR being the most treated type of MR (68% of interventions).4 Two recent randomized studies5,6 investigated the usefulness of percutaneous mitral valve repair with the MitraClip system in the setting of FMR with opposing results. While the Mitra-FR study5 observed no clinical benefit after MitraClip implantation compared with optimal medical therapy, the COAPT study6 demonstrated an improvement in symptoms and mortality in the group treated with MitraClip. The enlargement of the LV causes MR, and those patients with disproportionately higher MR than predicted by LV dimensions will be the best target for transcatheter mitral valve repair,7 which could partially explain the different results of these randomized studies. The Mitra-FR trial included patients with more advanced LV impairment, and consequently some of them may have “proportionate MR”; on the other hand, the larger LV and lower LV ejection fraction (LVEF) also suggest a more advanced stage of the cardiac disease. Indeed, the COAPT study excluded patients with a LVEF <20% and/or LV end-systolic diameter> 70mm. A recent study8 investigated the outcomes of MitraClip intervention in 2 groups of patients with FMR (high surgical risk vs nonhigh risk) and showed a substantial reduction in MR after the intervention, which was sustained at 1 year of follow-up, with an improvement in symptoms in both groups. As expected, the group with the highest surgical risk had higher mortality during follow-up. However, the influence of LVEF on outcomes after MitraClip implantation has remained controversial, with conflicting results.9–11 Classically, the surgical elimination of MR in patients with very dysfunctional LV has raised concerns due to a potential abrupt increase in afterload and transient myocardial dysfunction in these patients (afterload mismatch).12 However, some authors have reported successful outcomes after eliminating FMR with a MitraClip device in patients with severe11 and very severe LV dysfunction.10
The aim of this study was to evaluate the safety and impact of mitral valve repair with the MitraClip system on outcomes in FMR according to LV status.
METHODSThis was a single center observational study. Consecutive patients who underwent percutaneous mitral valve repair with the MitraClip system in our center were screened. The first 10 patients included in our MitraClip program were excluded from the present analysis to rule out the influence of the early learning curve. Only patients with FMR and a follow-up of at least 6 months were included. The study was approved by the Ethics Committee of our institution and complied with the Declaration of Helsinki.13
All the patients included in the MitraClip program at our center have a baseline visit at the cardiology outpatient clinic and are followed up in the same clinic after the intervention. The clinical records and echocardiographic images of the patients included were reviewed for the present analysis. LVEF was measured using the biplane Simpson method. The patient's demographic characteristics, New York Heart Association (NYHA) functional class and basic echocardiographic measurements before and after MitraClip implantation were recorded. Hospital records were reviewed in relation to hospital admission for congestive heart failure (CHF) the year before and after MitraClip implantation or heart transplant or death during the first year of follow-up. Survival analysis for cardiovascular outcomes included hospital admission due to CHF, heart transplant, or cardiovascular death during follow-up as cardiovascular endpoints.
The patients were divided into 2 groups according to LVEF and LV end-diastolic dimension (LVEDD): the first group included patients with worse LV status (LVEF ≤ 20%) and/or LVEDD ≥ 70mm (very poor LV group), and the second group included patients with LVEF> 20% and LVEDD <70mm (poor LV group).
Statistical analysisData are reported as percentages or as mean±standard deviation, as appropriate. A P value <.05 (2-sided) was considered statistically significant. Comparative analysis among groups was performed using the Student t test for independent samples of quantitative variables and the chi-square test to compare categorical variables. The paired Student t test was used for intragroup comparisons. Survival curves were estimated using the Kaplan-Meier product-limit estimator, and groups were compared using the log-rank test. Data were processed using SPSS version 19 (IBM, Armonk, New York, United States).
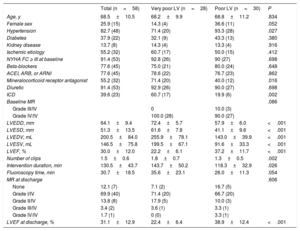
RESULTSSeventy-five patients underwent percutaneous mitral valve repair with the MitraClip system in our center between April 2012 and May 2018. The first 10 treated patients were excluded to rule out the possible influence of the early learning curve (April 2012–November 2013), and another 7 patients with pure degenerative MR were also excluded. Finally, 58 consecutive patients with FMR treated with a MitraClip system at our center were included. All patients had MR grade ≥ III/IV before the intervention. The very poor LV group included 28 patients: 7 with very low LVEF (≤ 20%), 9 with very severe LV enlargement (LVEDD ≥ 70 mm), and 12 with both parameters. The poor LV group included 30 patients with LVEF> 20% and LVEDD <70mm. Table 1 shows the baseline characteristics of the 2 study groups. Only the presence of hypertension was more prevalent in the poor LV group. The use of beta-blockers, angiotensin-converting-enzyme inhibitor (either angiotensin II receptor blocker or angiotensin II receptor blocker neprilysin inhibitor) and diuretics was similar in the 2 groups, with only the use of mineralocorticoid receptor antagonists being more prevalent in the very poor LV group. As expected, LV dimensions were significantly larger and LVEF was lower in patients with very poor LV. Regarding the intervention, there were no significant differences in MR reduction between the 2 groups, but patients with very poor LV (as a result of their larger LV) required a greater number of clips and longer interventions. Only 2 complications related to the intervention were observed: 1 esophageal erosion and 1 femoral hematoma without significant blood loss (no intervention was required to treat them). LVEF at discharge showed no significant differences compared with LVEF before MitraClip implantation (30.1±12.1% vs 31.1±12.9%, P=.279).
Baseline characteristics of included patients
| Total (n=58) | Very poor LV (n=28) | Poor LV (n=30) | P | |
|---|---|---|---|---|
| Age, y | 68.5±10.5 | 68.2±9.9 | 68.8±11.2 | .834 |
| Female sex | 25.9 (15) | 14.3 (4) | 36.6 (11) | .052 |
| Hypertension | 82.7 (48) | 71.4 (20) | 93.3 (28) | .027 |
| Diabetes | 37.9 (22) | 32.1 (9) | 43.3 (13) | .380 |
| Kidney disease | 13.7 (8) | 14.3 (4) | 13.3 (4) | .916 |
| Ischemic etiology | 55.2 (32) | 60.7 (17) | 50.0 (15) | .412 |
| NYHA FC ≥ III at baseline | 91.4 (53) | 92.8 (26) | 90 (27) | .698 |
| Beta-blockers | 77.6 (45) | 75.0 (21) | 80.0 (24) | .648 |
| ACEI, ARB, or ARNI | 77.6 (45) | 78.6 (22) | 76.7 (23) | .862 |
| Mineralocorticoid receptor antagonist | 55.2 (32) | 71.4 (20) | 40.0 (12) | .016 |
| Diuretic | 91.4 (53) | 92.9 (26) | 90.0 (27) | .698 |
| ICD | 39.6 (23) | 60.7 (17) | 19.9 (6) | .002 |
| Baseline MR | .086 | |||
| Grade III/IV | 0 | 10.0 (3) | ||
| Grade IV/IV | 100.0 (28) | 90.0 (27) | ||
| LVEDD, mm | 64.1±9.4 | 72.4±5.7 | 57.9±6.0 | <.001 |
| LVESD, mm | 51.3±13.5 | 61.6±7.8 | 41.1±9.6 | <.001 |
| LVEDV, mL | 200.5±84.0 | 255.9±78.1 | 143.0±39.9 | <.001 |
| LVESV, mL | 146.5±75.8 | 199.5±67.1 | 91.6±33.3 | <.001 |
| LVEF, % | 30.0±12.0 | 22.2±6.1 | 37.2±11.7 | <.001 |
| Number of clips | 1.5±0.6 | 1.8±0.7 | 1.3±0.5 | .002 |
| Intervention duration, min | 130.5±43.7 | 143.7±50.2 | 118.3±32.9 | .026 |
| Fluoroscopy time, min | 30.7±18.5 | 35.6±23.1 | 26.0±11.3 | .054 |
| MR at discharge | .606 | |||
| None | 12.1 (7) | 7.1 (2) | 16.7 (5) | |
| Grade I/IV | 69.9 (40) | 71.4 (20) | 66.7 (20) | |
| Grade II/IV | 13.8 (8) | 17.9 (5) | 10.0 (3) | |
| Grade III/IV | 3.4 (2) | 3.6 (1) | 3.3 (1) | |
| Grade IV/IV | 1.7 (1) | 0 (0) | 3.3 (1) | |
| LVEF at discharge, % | 31.1±12.9 | 22.4±6.4 | 38.9±12.4 | <.001 |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ARNI: angiotensin II receptor blocker neprilysin inhibitor; ICD, implantable cardioverter-defibrillator; LV, left ventricular; LVEDD, left ventricular end-diastolic diameter; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic diameter; LVESV, left ventricular end-systolic volume; MR, mitral regurgitation; NYHA FC, New York Heart Association functional class.
Data are expressed as no. (%) or mean±standard deviation.
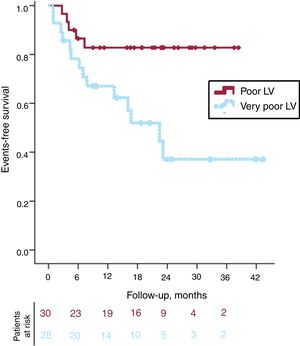
The mean follow-up was 19.5±13 months. During this period, 11 patients had at least 1 hospital admission due to CHF (9 in the very poor LV and 2 in the poor LV group), 2 patients underwent heart transplant (both in the very poor LV group), and 9 patients died due to cardiovascular events (4 in the very poor LV and 3 in the poor LV group): 1 cardiac shock, 5 end-stage CHF, and 3 sudden deaths (2 in the poor LV and 1 in the very poor LV). Another 8 patients died due to noncardiovascular causes (5 in the poor LV and 3 in the very poor LV group): 3 had renal failure, 2 had stroke, 1 had peritonitis, 1 committed suicide, and 1 died from thrombocytopenic purpura. Figure 1 shows the Kaplan-Meier survival curves for the cardiovascular endpoints in the 2 groups. Event-free survival curves showed significantly better outcomes for the poor LV group (log-rank 3.706; P=.010). Both groups showed an initial parallel loss of patients during the first 6 months, and after this initial period the remaining patients with poor LV remained stable during the rest of the follow-up. In contrast, patients with very poor LV showed a continuous reduction in event-free survival during follow-up.
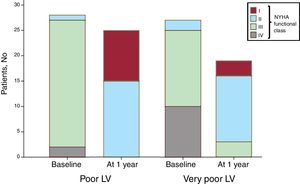
Clinical outcomes at 1 yearA cross sectional analysis was performed at 1 year after MitraClip implantation to evaluate clinical outcomes (n=55; 27 in the very poor LV and 28 in the poor LV group), showing symptom improvement in both groups (figure 2). At 1 year of follow-up, all the patients with poor LV were in NYHA I-II (vs 3.5%; n=1 at baseline), as were most (84%; n=16) of the patients with very poor LV (at baseline only 2 patients [7.4%] in the very poor LV group were in NYHA I-II).
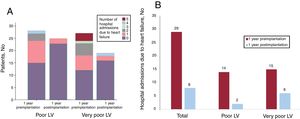
Figure 3A shows hospital admissions due to CHF before and after MitraClip implantation. During the year prior to the intervention, 15 patients (55.5%) with very poor LV and 13 patients (46.4%) with poor LV had at least 1 hospital admission due to CHF (range,1-5). During the first year after MitraClip implantation, only 3 (11.1%) and 2 (7.1%) patients, respectively, had a CHF episode requiring hospital admission (range,1-4). Figure 3B shows the total number of hospital admissions due to CHF including only those patients without death or heart transplantat during the first year after implantation. In both groups, the number of hospitalizations was substantially reduced, with a total decrease of 72.4% (21 fewer hospital admissions during the year after the implantation compared with the year prior the intervention).
Hospital admission due to heart failure. A: number of hospital admissions per patient during the year before the Mitraclip implantation compared with the first year after the intervention (including all the patients). B: total number of hospital admissions of all the 1-year survivors during the year before and 1 year after MitraClip implantation. LV, left ventricular.
Echocardiographic follow-up was available for 40 patients (18 with very poor LV and 22 with poor LV). The study was performed 11.9±1.9 months after the implantation. There were no significant differences between baseline LVEF and LVEF 1 year after implantation (29.6±11.0% vs 30.6±12.5%; P=.418). Most of the patients showed a sustained good result at follow-up with MR ≤ grade II/IV (82.5%; n=33) and without significant differences between groups (very poor LV 77.8%, n=14 vs poor LV 86.3%, n=19; P=.477).
Initial learning curveThe results of the excluded patients treated during the early learning curve were very different to those observed in the rest of our series; in the latter, no significant safety events were observed and 96% of the patients had a residual MR ≤ grade II/IV. The early learning curve took place at our center during the global learning curve of the technique. Almost all the patients treated during this period (April 2012–November 2013) had functional MR (9 out of 10) with severe MR and low LVEF (mean 24.2%±4.9%). Despite no deaths occurred during this early learning phase, there were 2 pericardial effusions with cardiac tamponade, 2 partial detachments, and 1 vascular complication. The final outcome of the intervention was also more modest in these early procedures with 3 patients having mild MR, 3 moderate MR, and 3 severe MR at discharge.
DISCUSSIONThe results of the present study suggest that MitraClip implantation is safe in all patients with FMR as depicted by the absence of procedural deaths. Venous vascular access, echo-guided transseptal puncture and the nonuse of contrast reduce the possibility of complications during implantation in experienced centers. Although patients with worse LV status (LVEF <20% and/or LVEDD> 70mm) showed worse midterm cardiovascular outcomes after MitraClip implantation than those with less advanced LV remodeling, symptoms improved in all patients, and no acute transient myocardial dysfunction was observed after the intervention. After 1 year of follow-up, both groups showed improvement in NYHA functional class and a reduction in the number of hospital admissions due to CHF.
Our results are consistent with those reported in the literature. Although the German registry11 included both functional and degenerative MR, clinical improvement was observed 1 year after MitraClip implantation, with patients with LVEF <30% showing slightly worse cardiovascular outcomes. The European registry9 showed a worse prognosis for patients with FMR and lower LVEF; however, they did not consider LV dimensions. In contrast, Barth et al.10 proposed a similar prognosis even in patients with LVEF <20%. However, they did not report any data on LV dimensions, and the follow-up was less than 3 months in almost 30% of the patients. The worse outcomes in patients with more impaired LV may explain, in part, the differences between the COAPT 6 and the Mitra-FR5 trials. Patients with remodeled LV but less severe MR (“proportionate MR”7) may not benefit from MitraClip implantation since LV function is the main problem and small changes in the amount of MR may not affect their prognosis or symptoms. Of note, all the patients included in our study had at least moderate to severe MR (≥ grade III/IV) and all the patients in the very poor LV group had severe MR (grade IV/IV). Although we cannot rule out the possibility that some patients included in the very poor LV group may have had proportionate MR,7 we believe that the more advanced cardiac disease may have played an important role in their worse cardiovascular outcomes.
Percutaneous mitral valve repair with the MitraClip system for FMR seems to be more effective in patients without extreme LV remodeling, as observed in the present and previous studies.6,9,11 While patients with very poor LV had worse cardiovascular outcomes and MitraClip implantation may have seemed to be less efficient in these patients, an improvement in functional class and a reduction in the number of hospital admissions due to CHF was also observed. This should be taken into account in terms of cost-effectiveness; on the one hand, MitraClip implantation might be useful to reduce the costs of hospital admissions and improve the quality of life of these very sick patients, and on the other hand, it could have implications in patient selection for percutaneous mitral valve repair within the context of a limited budget for this type of intervention in some countries. In our hospital, the average cost of a hospital admission due to CHF is around €5600, so its reduction in the group of survivors during the year after the MitraClip implantation saved around €117 600 due to fewer hospital admissions. Importantly, the emergence of noninvasive techniques makes the usefulness of this intervention more likely. Future larger studies are needed to determine the cost-effectiveness of the MitraClip procedure, taking into account these considerations since the survival of some patients may not improve but an improvement in symptoms and a reduction in the number of hospital admissions may justify this intervention and outweigh the cost of the device.
LimitationsThis was a single center study including a limited number of patients and, because it was an observational study, patients were treated according to criteria of their cardiologist. Despite the lack of statistically significant differences between the heart failure drugs, their dosages were not compared, and therefore we cannot exclude a difference in drug dosage between the 2 groups. The prognostic comparisons among the group of “poor LV” and “very poor LV” were not adjusted for the patients’ baseline characteristics. The MR quantification was performed by expert cardiologists on cardiac imaging, but the effective regurgitant orifice of the MR was not available for all the patients and consequently it was not included in the present study.
CONCLUSIONSMitraClip implantation seems to be safe and effective in reducing MR in patients with FMR and very severe LV dysfunction and remodeling. Patients with FMR and very low LVEF (< 20%) and/or very enlarged LV (LVDD> 70 mm) showed significantly worse cardiovascular outcomes after MitraClip implantation than those with less LV dysfunction and remodeling. However, despite this worse prognosis, the intervention resulted in an improvement in symptoms and a reduction in the number of hospital admissions regardless of LV status.
CONFLICTS OF INTERESTL. Sanchis, X. Freixa, and M. Sitges are proctors for Abbott for MitraClip implantation.
- -
The classic surgical treatment of FMR remains controversial.
- -
Percutaneous mitral valve repair with the MitraClip system seems to be useful for patients with FMR.
- -
The usefulness of percutaneous treatment of those patients with FMR and severely reduced LVEF remains unknown.
- -
We evaluated the safety and the impact of MitraClip implantation on outcomes in FMR according to LV status to investigate its usefulness for those patients with extreme LVEF values and dimensions.
- -
Patients with very poor LVEF during follow-up had worse event-free survival for cardiovascular events than those without extreme LVEF values.
- -
However, 1 year after the intervention, all patients with FMR (regardless of LV status) showed symptom improvement and a reduction in the number of hospital admissions due to CHF.