Fast ventricular tachycardias in the ventricular fibrillation zone in patients with an implantable cardioverter-defibrillator are susceptible to antitachycardia pacing (ATP) termination. Some manufacturers allow programming 2 ATP bursts: before charging (BC) and during (DC) charging. The aim of this study was to describe the safety and effectiveness of ATP BC and DC for fast ventricular tachycardias in the ventricular fibrillation zone in patients with an implantable cardioverter-defibrillator in daily clinical practice.
MethodsData proceeded from the multicenter UMBRELLA trial, including implantable cardioverter-defibrillator patients followed up by the CareLink monitoring system. Fast ventricular tachycardias in the ventricular fibrillation zone until a cycle length of 200ms with ATP BC and/or ATP DC were included.
ResultsWe reviewed 542 episodes in 240 patients. Two ATP bursts (BC/DC) were programmed in 291 episodes (53.7%, 87 patients), while 251 episodes (46.3%, 153 patients) had 1 ATP burst only DC. The number of episodes terminated by 1 ATP DC was 139, representing 55.4% effectiveness (generalized estimating equation-adjusted 60.4%). There were 256 episodes terminated by 1 or 2 ATP (BC/DC), representing 88% effectiveness (generalized estimating equation-adjusted 79.3%); the OR for ATP effectiveness BC/DC vs DC was 2.5, 95%CI, 1.5-4.1; P <.001. Shocked episodes were 112 (45%) for ATP DC vs 35 (12%) for ATP BC/DC, representing an absolute reduction of 73%. The mean shocked episode duration was 16seconds for ATP DC vs 19seconds for ATP BC/DC (P=.07).
ConclusionsThe ATP DC in the ventricular fibrillation zone for fast ventricular tachycardia is moderately effective. Adding an ATP burst BC increases the overall effectiveness, reduces the need for shocks, and does not prolong episode duration.
Keywords
The benefit of implantable cardioverter-defibrillators (ICD) in reducing cardiac arrest has been demonstrated in many studies.1–4 Initial ICD therapy is usually antitachycardia pacing (ATP) for slow ventricular tachycardias (VT) while fast VT and ventricular fibrillation (VF) are treated with high-energy shocks. Most (66%-76%) of the ventricular arrhythmias detected in the VF zone are fast monomorphic VT5–8 that can be terminated by ATP without the need for high-energy shocks.9–11 Several studies have demonstrated that empirically programming 1 ATP burst in the fast VT zone is highly effective in terminating fast VT with cycle length (CL) between 320 and 240 milliseconds (ms) suggesting that ATP may reduce the need for high-energy shock without increasing morbidity.6–8,12,13 However, published data suggest that ATP effectiveness is lower if VT CL <270ms,7 while the effectiveness of increasing the number of ATP bursts for very fast VT is still a matter of debate.8,14 Furthermore, short CL is a predictor of ATP failure and VT acceleration.11,15 Finally, in the case of ineffective ATP, devices require redetection and capacitor charging before shock delivery, which leads to longer episode duration and may increase the risk of syncope. In addition, several studies have shown that shocks are not harmless and may lead to a 3-fold increase in mortality risk.16–18
The possibility of programming ATP bursts before charging (BC) and/or during charging (DC) in the VF zone (EnTrust study19) was developed to avoid delay in high-energy shock administration in cases of ATP failure while maintaining the potential for harmless VT termination in the VF zone. The effectiveness of this type of programming has not been evaluated in a broad population of patients in daily clinical practice. The aim of this study was to evaluate the effectiveness and safety profile of ATP BC and/or ATPDC in ICD patients with fast VT detected in the VF zone and to describe predictors of effectiveness in our population.
MethodsStudy Design and ObjectivesWe analyzed data from the UMBRELLA trial, a multicenter prospective observational study including ICD patients followed up by the CareLink monitoring system. Patients who had episodes of sustained monomorphic VT detected in the VF zone were enrolled. We compared the safety and effectiveness of a single ATP burst DC with a strategy of 2 successive ATP sequences (ATP BC/ATP DC) for termination of VT episodes (CL 200-320ms). We performed univariate and multivariate analyses to describe predictors of ATP effectiveness.
The UMBRELLA RegistryThe present investigation was developed within the framework of the National UMBRELLA Registry (Incidence of Arrhythmias in Spanish Population With a Medtronic Implantable Cardiac Defibrillator Implant, NCT01561144). This registry is a prospective and retrospective study of the population implanted with a Medtronic ICD in Spain. The prospective part of the UMBRELLA study (since 2011) includes all patients implanted with a Medtronic ICD in Spain with prospective collection of all arrhythmic events and ICD interventions via the CareLink monitoring system. All patients implanted with a Medtronic ICD before 2011 and already followed up via the CareLink system were included in the UMBRELLA registry, their clinical and demographic characteristics were collected at the time of ICD implant, and all the arrhythmic events and ICD interventions reported by the monitoring system were included. These patients have been followed up prospectively since 2011. In the present investigation, patients proceeded from both the study and the registry. All the information retrieved from the ICD during CareLink monitoring was analyzed. The episodes recorded were reviewed by a committee of reviewers. Further description of this registry has been reported elsewhere.20
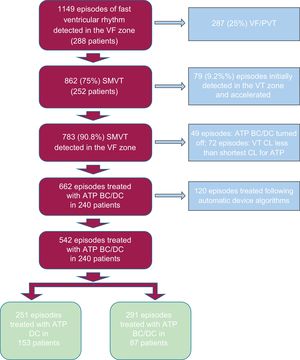
Upon completion of this subanalysis, the UMBRELLA study had 1645 patients from 38 centers and 6829 episodes of VT. Among 1645 patients, 288 experienced 1149 episodes of ventricular rhythm detected in the VF zone. Of them, 662 were sustained monomorphic VT that received ATP BC/ATP DC. Of 662 episodes, 120 were eliminated from the analysis to avoid selection bias (see below for details). The remaining 542 episodes in 240 patients were analyzed in the present study (Figure 1). Ventricular events excluded from the study were mostly VF/polymorphic VT (287 [25%]) or slow VT accelerated to the VF zone after ATP burst (79 [9.2%]). The study was carried out with ethical approval. Written informed consent was obtained from all patients.
Selection algorithm for ventricular arrhythmias episodes detected in the VF zone. ATP, antitachycardia pacing; BC, before charging; CL, cycle length; DC, during charging; SMVT, sustained monomorphic ventricular tachycardia; VF, ventricular fibrillation; PVT, polymorphic ventricular tachycardia.
Following predetermined criteria, arrhythmia was classified as VT when starting with a sudden change in heart rate, had regular R–R intervals, and the morphology of the electrocardiogram differed from native ventricular conduction. Arrhythmia CL was reported as the mean of the 8 intervals preceding detection. Episodes of ventricular origin with CL between 320-200ms detected in the VF zone were included in the study.
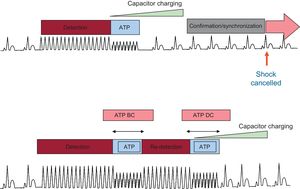
Only episodes with ATP BC/ATP DC programmed ON were included. Episodes were divided based on 2 program modalities for the ATP BC/ATP DC feature (Figure 2)21. Initial ATP DC feature programming (ATP DC or ATP BC/ATP DC) was at the clinician's discretion. Patients and episodes were divided into 2 groups based on the initial device programming.
Implantable cardioverter-defibrillator functioning algorithm for ATP BC and DC. ATP DC only (upper panel) and BC/DC (lower panel). ATP, antitachycardia pacing; BC, before charging; DC, during charging. Modified with permission from Schwab et al.21
The first modality (ATP DC) consists of 1 ATP burst during charging: after detection, the ICD starts charging and simultaneously delivers 1 ATP burst. If 4 out of the first 5 intervals after the capacitor charge end are not in the VT zone, the shock is aborted, otherwise a high-energy shock is delivered with no further delay. The second modality (ATP BC/ATP DC) programs 1 ATP burst BC: after detection, the ICD delivers 1 ATP burst without starting charging. This is followed by a redetection algorithm that, if the VT persists, starts charging while the second burst is delivered. This algorithm slightly prolongs the time to shock delivery. Nevertheless, it allows the administration of 2 ATP bursts, it introduces a redetection algorithm between the first and second burst, and it avoids capacitor charging if the first burst is effective. The number of intervals needed for detection was nominally set at 12/16 after the first burst in the ATP BC/ATP DC group. The remaining device features were programmed at the physician's discretion, according to the patient's characteristics and underlying heart disease.
The ATP BC/ATP DC feature is enhanced by 3 automatic algorithms that, based on the effectiveness of the first ATP burst in an episode, are able in subsequent episodes to switch from ATP DC to ATP BC and vice versa or to switch off ATP. This automatic programming could lead to erroneous interpretation of the effectiveness of ATP. Hence those episodes following an automatic change were eliminated from the analysis, 90% of them resulted from an automatic switch from ATP DC to ATP BC/ATP DC after 1 episode of VT treated efficaciously with ATP DC. The aim of this switch is to save battery drain, thus avoiding charge, and to deliver 2 ATP bursts (ATP BC and ATP DC) if necessary. The episodes were eliminated from the analysis because they introduced a selection bias and could overestimate ATP BC/ATP DC effectiveness.
When available, the far-field electrocardiogram before detection was reviewed to aid in rhythm classification. Episode duration was measured from the first tachycardia beat to the first nontachycardic beat. Acceleration was defined as a CL reduction greater than 10% after therapy. Episodes in the VT or fast VT zone accelerated after an ATP burst and detected in the VF zone were excluded.
All episodes with high ventricular rate recorded in the ICD were reviewed by an Episodes Review Committee. The committee was composed of 6 experts, divided into 3 pairs. The committee classification algorithm has been previously detailed.20
Statistical AnalysisContinuous variables are expressed as mean±standard deviation or median [interquartile range, IQR], according to whether they followed a normal distribution or not, and categorical variables are presented as numbers and percentages. The Student t test or Mann-Whitney U-test were used for normal or nonnormal continuous variables, and the chi-square or Fisher exact test were used as appropriate for categorical variables. To adjust ATP efficacy estimation so as to take into account multiple episodes per patient, the generalized estimating equation (GEE) method was used22; in particular, we verified that our clustered data were not balanced and had no logical ordering for observations within a cluster, and we therefore used an exchangeable correlation matrix. Variables known to be related to ATP effectiveness or whose relationship had been previously published were included in a univariate analysis. Multivariate analysis was performed by using logistic regression GEE-adjusted analysis, including the dimension of time as a covariate as the time elapsed between baseline and each episode. Any variable in the preceding univariate analyses with P <.2 was included in the model. Statistical significance was set at P <.05 (2-tailed). Data were analyzed using SPSS 18.3 for Windows (SPSS Inc).
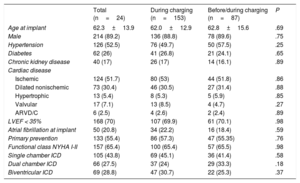
ResultsStudy Population and Characteristics of the Ventricular Tachycardia EpisodesA total of 240 patients with structural heart disease were included in the study and were followed up for 38 months (median [IQR, 25-52]). Baseline characteristics are shown in Table 1. Patients were divided into 2 groups based on the initial programming of the ATP DC feature. No differences were observed between patients programmed with 1 ATP DC vs those with ATP BC/ATP DC. During the follow-up, 542 episodes of sustained monomorphic VT registered in the VF zone were treated by ATP BC/ATP DC. The median number of episodes per patient was 1 [IQR, 1-2] and the maximum number of episodes was 28 episodes in a single patient.
Patients’ Baseline Characteristics
| Total (n=24) | During charging (n=153) | Before/during charging (n=87) | P | |
|---|---|---|---|---|
| Age at implant | 62.3±13.9 | 62.0±12.9 | 62.8±15.6 | .69 |
| Male | 214 (89.2) | 136 (88.8) | 78 (89.6) | .75 |
| Hypertension | 126 (52.5) | 76 (49.7) | 50 (57.5) | .25 |
| Diabetes | 62 (26) | 41 (26.8) | 21 (24.1) | .65 |
| Chronic kidney disease | 40 (17) | 26 (17) | 14 (16.1) | .89 |
| Cardiac disease | ||||
| Ischemic | 124 (51.7) | 80 (53) | 44 (51.8) | .86 |
| Dilated nonischemic | 73 (30.4) | 46 (30.5) | 27 (31.4) | .88 |
| Hypertrophic | 13 (5.4) | 8 (5.3) | 5 (5.9) | .85 |
| Valvular | 17 (7.1) | 13 (8.5) | 4 (4.7) | .27 |
| ARVD/C | 6 (2.5) | 4 (2.6) | 2 (2.4) | .89 |
| LVEF < 35% | 168 (70) | 107 (69.9) | 61 (70.1) | .98 |
| Atrial fibrillation at implant | 50 (20.8) | 34 (22.2) | 16 (18.4) | .59 |
| Primary prevention | 133 (55.4) | 86 (57.3) | 47 (55.35) | .76 |
| Functional class NYHA I-II | 157 (65.4) | 100 (65.4) | 57 (65.5) | .98 |
| Single chamber ICD | 105 (43.8) | 69 (45.1) | 36 (41.4) | .58 |
| Dual chamber ICD | 66 (27.5) | 37 (24) | 29 (33.3) | .18 |
| Biventricular ICD | 69 (28.8) | 47 (30.7) | 22 (25.3) | .37 |
ARVD/C, arrhythmogenic right ventricular dysplasia/cardiomyopathy; ICD, implantable cardioverter-defibrillator; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Data are expressed as No. (%) or mean±standard deviation.
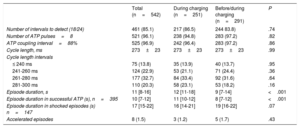
Implantable cardioverter-defibrillator programming is shown in Table 2. All the episodes included in the study had at least 1 ATP burst before shock; of these, 251 episodes had 1 ATP burst only, during capacitor charging (ATP DC), while 291 episodes had 2 ATP bursts: 1 BC and 1 DC (ATP BC/ATP DC). The number of intervals needed for detection was set at 18/24 in 85.1% of the episodes, without differences between the 2 groups.
Implantable Cardioverter-defibrillator Programming and Ventricular Tachycardia Episode Characteristics
| Total (n=542) | During charging (n=251) | Before/during charging (n=291) | P | |
|---|---|---|---|---|
| Number of intervals to detect (18/24) | 461 (85.1) | 217 (86.5) | 244 83.8) | .74 |
| Number of ATP pulses=8 | 521 (96.1) | 238 (94.8) | 283 (97.2) | .82 |
| ATP coupling interval=88% | 525 (96.9) | 242 (96.4) | 283 (97.2) | .86 |
| Cycle length, ms | 273±23 | 273±23 | 273±23 | .99 |
| Cycle length intervals | ||||
| ≤ 240 ms | 75 (13.8) | 35 (13.9) | 40 (13.7) | .95 |
| 241-260 ms | 124 (22.9) | 53 (21.1) | 71 (24.4) | .36 |
| 261-280 ms | 177 (32.7) | 84 (33.4) | 92 (31.6) | .64 |
| 281-300 ms | 110 (20.3) | 58 (23.1) | 53 (18.2) | .16 |
| Episode duration, s | 11 [8-16] | 12 [11-18] | 9 [7-14] | <.001 |
| Episode duration in successful ATP (s), n=395 | 10 [7-12] | 11 [10-12] | 8 [7-12] | <.001 |
| Episode duration in shocked episodes (s) n=147 | 17 [15-22] | 16 [14-21] | 19 [16-22] | .07 |
| Accelerated episodes | 8 (1.5) | 3 (1.2) | 5 (1.7) | .43 |
ATP, antitachycardia pacing.
Data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The main characteristics of the VT episodes are shown in Table 2. The mean VT CL was 273±23ms, with no differences between the 2 groups. The distribution of CL intervals between the 2 groups is also shown in Table 2. No differences were observed across any CL intervals.
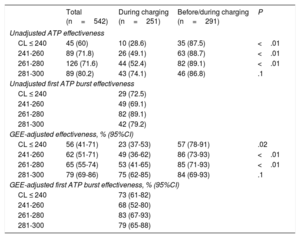
Antitachycardia Pacing EffectivenessOverall, ATP therapy effectiveness was 72.9%, terminating 395 out of 542 episodes of VT in the VF zone (Table 3).
Effectiveness of Antitachycardia Pacing and Shock Reduction
| Total (n=542) | During charging (n=251) | Before/during charging (n=291) | P/OR | |
|---|---|---|---|---|
| Unadjusted ATP effectiveness | 395 (72.9) | 139 (55.4) | 256 (88) | <.001 |
| Unadjusted first ATP burst effectiveness | 202 (69.4) | |||
| GEE-adjusted effectiveness, % (95%CI) | 67.3 (61.7-72.5) | 60.4 (53.3-67.1) | 79.3 (71.6-85.3) | 2.5 (1.5-4.1) <.001 |
| GEE-adjusted first ATP burst effectiveness, % (95%CI) | 63.7 (55.1-71.6) | |||
| Episodes terminated by shock | 147 (27.1) | 112 (44.6) | 35 (12) | <.001 |
| GEE-adjusted for high-energy shock termination, % (95%CI) | 32.7 (27.5-38.3) | 39.6 (32.9-46.7) | 20.7 (14.7-28.4) | 0.4 (0.24-0.66) <.001 |
| Total number of shocks | 174 | 133 | 41 | <.001 |
| Mean number of shocks per episode | 0.32 | 0.53 | 0.14 | <.001 |
| Mean number of shocks per episode (episodes with shock) | 1.18 | 1.19 | 1.17 | .43 |
| Shocks in episodes with successful ATP | 20 (5.1) | 19 (13.6) | 1 (0.4) | <.001 |
95%CI, 95% confidence interval; ATP, antitachycardia pacing; GEE, generalized estimating equation; OR, odds ratio.
Unless otherwise indicated, data are expressed as No. (%).
The number of episodes terminated by 1 ATP burst DC was 139, representing 55.4% effectiveness (GEE-adjusted, 60.4%; 95%CI, 53.3-67.1), while the number of episodes terminated by 1 or 2 ATP bursts BC/DC was 256, representing 88% effectiveness (GEE-adjusted, 79.3%; 95%CI, 71.6-85.3). In the group of episodes with programmed ATP BC/ATP DC, 2 ATP bursts were delivered in 89 episodes (30.6%). In this group, the first ATP burst (ATP BC) was effective in 202 episodes (69.4%, GEE-adjusted, 63.7%; 95%CI, 55-72).
The univariate GEE-adjusted odds ratio (OR) of ATP effectiveness for the ATP BC/ATP DC group vs ATP DC group was 2.5 (95%CI, 1.5-4.1; P <.001). Table 3 shows data of crude and GEE-adjusted ATP effectiveness.
Globally, crude ATP effectiveness ranged from 60% for very fast VT (CL ≤ 240ms) to 80% for VT between 281 and 300ms (Table 4). Crude ATP effectiveness was consistently higher across all CL in the ATP BC/ATP DC group vs ATP DC group, but this difference was not statistically significant for VT between 281 and 300ms. The GEE-adjusted analysis resulted in the same significant difference for faster VT and similar effectiveness for VT with slower CL (281-300ms).
Effectiveness of Antitachycardia Pacing by Tachycardia Cycle Length
| Total (n=542) | During charging (n=251) | Before/during charging (n=291) | P | |
|---|---|---|---|---|
| Unadjusted ATP effectiveness | ||||
| CL ≤ 240 | 45 (60) | 10 (28.6) | 35 (87.5) | <.01 |
| 241-260 | 89 (71.8) | 26 (49.1) | 63 (88.7) | <.01 |
| 261-280 | 126 (71.6) | 44 (52.4) | 82 (89.1) | <.01 |
| 281-300 | 89 (80.2) | 43 (74.1) | 46 (86.8) | .1 |
| Unadjusted first ATP burst effectiveness | ||||
| CL ≤ 240 | 29 (72.5) | |||
| 241-260 | 49 (69.1) | |||
| 261-280 | 82 (89.1) | |||
| 281-300 | 42 (79.2) | |||
| GEE-adjusted effectiveness, % (95%CI) | ||||
| CL ≤ 240 | 56 (41-71) | 23 (37-53) | 57 (78-91) | .02 |
| 241-260 | 62 (51-71) | 49 (36-62) | 86 (73-93) | <.01 |
| 261-280 | 65 (55-74) | 53 (41-65) | 85 (71-93) | <.01 |
| 281-300 | 79 (69-86) | 75 (62-85) | 84 (69-93) | .1 |
| GEE-adjusted first ATP burst effectiveness, % (95%CI) | ||||
| CL ≤ 240 | 73 (61-82) | |||
| 241-260 | 68 (52-80) | |||
| 261-280 | 83 (67-93) | |||
| 281-300 | 79 (65-88) | |||
95%CI, 95% confidence interval; ATP, antitachycardia pacing; CL, cycle length; GEE, generalized estimated equation.
Unless otherwise indicated, data are expressed as No. (%).
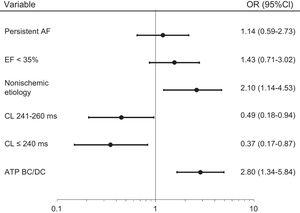
Multivariate GEE-adjusted analysis showed 3 variables significantly related to ATP effectiveness: programming ATP BC/ATP DC vs ATP DC only (OR, 2.8; 95%CI, 1.3-5.8; P <.001) and nonischemic cardiomyopathy vs other cardiac diseases (OR, 2.1; 95%CI, 1.1-4.5; P=.041) were associated with higher ATP effectiveness, while CL ≤ 240ms (OR, 2.67; 95%CI, 1.15-5.8; P=.03) and CL 241-260ms (OR, 2.04; 95%CI, 1.1-5.4; P=.03) were associated with lower ATP effectiveness (Figure 3).
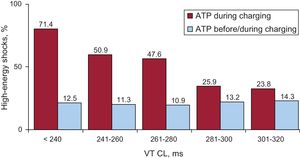
High-energy Shock ReductionOverall 147 episodes (27.1%) required high-energy shocks: 112 (44.6%) episodes treated with ATP DC vs 35 episodes (12%) treated with ATP BC/ATP DC (Table 3). Programming ATP BC/ATP DC was associated with a 73% (66%-79%) absolute risk reduction in the need for high-energy shock.
The GEE-adjusted OR for high-energy shocks in the ATP BC/ATP DC group vs ATP DC group was 0.4 (95%CI, 0.24-0.66; P <.001).
Significant high-energy shock reduction was observed for all CL intervals, including very fast VT with CL ≤ 240ms (Figure 4).
The ICD delivered high-energy shocks in 20 episodes (5.1%); although the ATP burst had been effective in terminating the VT, 19 of them occurred in the ATP DC group vs only 1 episode in the ATP BC/ATP DC group (P <.001). Analysis of the termination modality revealed that all these episodes had some ventricular paroxysmal beat after the ATP burst and the VT termination. These ventricular paroxysmal beats fell into the short redetection window after capacitor charging and triggered shock delivery.
The overall number of shocks and the mean number of shocks per episode were higher in the ATP DC group, while the mean number of shocks in shocked episodes showed no differences between the 2 groups.
The median episode duration was 11seconds [IQR, 8-16 s]. Episodes programmed with ATP BC/ATP DC were significantly shorter (Table 2).
The median episode duration for successfully ATP-terminated episodes was slightly longer in the ATP DC group, which could be explained by the different redetection algorithm. In fact, in the ATP DC group, the ICD waits for the complete capacitor charge and for the end of the redetection window before considering the episode terminated and aborting the shock. There was a nonsignificant trend to longer episode duration for shocked episodes in the ATP BC/ATP DC group vs ATP DC group: 19 s (16-22) vs 16 s (14-21); P=.07.
Acceleration of VT was low in both groups (Table 2), occurring in 5 VT episodes in the ATP BC/ATP DC group (1.7%) vs 3 episodes (1.2%) in the ATP DC group (P=NS). Of note, 2 out of 5 episodes of accelerated VT in the ATP BC/ATP DC group were treated successfully with the second ATP burst.
DiscussionMain FindingsThis is the first prospective multicenter study showing that adding a second ATP burst before capacitor charging in the VF zone is associated with a decrease in high-energy shocks and with higher ATP effectiveness compared with a single ATP burst during charging only.
Effectiveness of Antitachycardia PacingAntitachycardia pacing is an effective therapy for harmless fast VT termination, as shown by studies testing 2 or more ATP bursts in the VT and fast VT zone.14,23 Moreover, it has been observed that programming 2 or more ATP bursts in the fast VT zone is more effective in increasing global ATP effectiveness than the standard therapy with 1 ATP burst, leading to a reduction of high-energy shocks needed for VT termination.20
In the VF zone, the ICD has traditionally been programmed to avoid delay in shock delivery, given the concern about ATP effectiveness in this detection zone and the need for a quick definitive treatment. The Entrust study19 was the first nonrandomized trial designed to determine the effectiveness of ATP DC for fast VT detected in the VF zone. Episodes were not separated based on the type of ATP delivered (ATP DC or ATP BC). Despite the limited number of VT episodes included in the study (n=84), the effectiveness of ATP BC/ATP DC was nearly 70% for episodes with CL <300ms.
In our population, we observed that adding a second ATP burst before capacitor charging increased global adjusted ATP effectiveness from 60.4% to 79.3% for ATP BC/ATP DC. This finding may be explained by 2 factors. First, it is known that ATP is effective in terminating fast VT, so the addition of 1 more burst may be able to increase global ATP effectiveness, even in very fast VT. Second, the different algorithms of the 2 ATP strategies seem to play a critical role. The administration of the ATP burst BC is followed by a redetection algorithm that evaluates the persistence of the VT. In contrast, if ATP DC only is programmed, after the ATP burst the detection of ≥ 2 out of 5 intervals in the VT zone triggers shock delivery. This difference makes the ATP BC more specific in term of avoiding unnecessary shocks. This is particularly important when considering that a not insignificant number of VT in the VF zone shows delayed termination after the ATP burst or is followed by several ventricular extra beats that might confound an excessively sensitive redetection algorithm. This also helps to partially explain the higher observed ATP effectiveness for the first ATP burst in the ATP BC/ATP DC group vs ATP DC group (69.4% vs 55.4%). The difference observed was much lower when corrected by the GEE-adjustment and the remaining gap may be due to the role played by the different redetection algorithm, as reported previously. As explained in the methods section, we decided to exclude from the analysis those episodes accelerated from slow VT after 1 or more ATP bursts as they are not primarily fast VT; they come from an ineffective and proarrhythmic ATP burst leading to a considerably diminished effectiveness of ATP in this specific setting and a possible selection bias.
Nonischemic cardiomyopathy was related to significantly higher ATP effectiveness in our population. The efficacy of ATP for fast VT was initially described for ischemic patients; however, there is evidence that it is also a highly effective strategy for nonischemic patients, as reported by the PAINFREE II and the ADVANCE CRT-D Trial.7,24 In light of our results and of these previous studies, nonischemic patients seem to be good candidates for ATP termination of fast VT episodes.7,24
Short CL resulted in lower ATP effectiveness on multivariate analysis. Although the literature is controversial on this association11,20 we believe that there are many plausible explanations for lower ATP effectiveness in very fast VT. Nevertheless, lower global effectiveness in this CL range should not lead to conservative programming with only 1 ATP burst as we described higher effectiveness with ATP BC/ATP DC programming and shock reduction also in very fast VT episodes.
Shock ReductionWe observed that programming 2 ATP bursts before and during charging was associated with a 73% reduction in high-energy shocks compared with conventional programming of a single burst DC.
We also observed that programming 2 ATP bursts was related to a slight nonstatistically significant prolongation of the VT episode if there was ATP failure. The observed difference was due to the time needed for the delivery of the second ATP burst and was similar to the prolongation observed in previous published studies,7,25 which did not report an increased incidence of syncope.
Shock reduction is essential when optimizing ICD programming, since it has very important clinical implications.
It has been described that ICD shocks are associated with lower quality of life26 and they may be associated with worsening heart failure and increased mortality.18 For these reasons, a strategy to minimize the need for high-energy shocks would be advisable, even in the case of very fast VT. The addition of an ATP burst BC seems to help to avoid unnecessary shocks.
It is important to stress that we observed a considerable number of shocks delivered after an effective ATP burst, almost only in the ATP DC group, representing 13.6% of the shocks in this group, especially if there were ventricular extra beats after VT termination. This finding reinforces the importance of programming an ATP burst BC followed by a redetection window with good specificity. To improve ATP specificity, apart from programming 2 ATP bursts and 2 successive redetections, a new algorithm after the ATP burst DC has recently been developed, which seems to decrease the unnecessary shock delivery.27 Finally, ATP BC avoids the energy consumption represented by capacitor charging that dissipates if ATP is effective,28 influencing battery life.
In our study, most of the episodes had the number of intervals needed set at 18/24, while recent evidence suggests that programming longer detection intervals might reduce the likelihood of receiving ICD therapy, especially shocks.25 It is therefore possible that our study overestimated the effectiveness of the ATP, since a significant number of VT terminate spontaneously when detection intervals are longer. Nevertheless, we believe that, once the ICD has detected the VT episode, regardless of the length of the detection window, the optimization of ATP by programming bursts before and during charging is crucial to terminate the VT and avoid shocks. Based on recent evidence, it may be advisable to program prolonged detection windows and ATP bursts BC/DC to maximize effectiveness and reduce high-energy shocks.
LimitationsThe most important limitation lies in the absence of randomization and a control group. All the patients were enrolled in a nationwide observational study and the device programming depended on the clinical practice of each center. Patients were included prospectively; nevertheless the analysis performed is retrospective. The criteria that led to programming of 1 or 2 ATP bursts depended on the physician and could be related to clinical characteristics or features of the tachycardia episodes that could not be investigated in the present study.
Some other aspects of ICD programming were not homogeneous, such as the number of intervals needed to detect or the shortest CL for ATP administration. Finally, the criteria used to assess the safety of this programming algorithm are indirect and related mainly to high-energy shock reduction and to episode duration. We could not reliably collect data regarding syncopal events; therefore. they were not included in this study.
ConclusionsThis study suggests that programming 1 ATP burst BC in addition to a standard burst ATP DC in ICD patients who show fast VT in the VF zone is associated with a significant reduction in high-energy shocks. Moreover this type of programming does not seem to prolong episode duration and may avoid battery consumption due to capacitor charging in the case of ATP DC only. This strategy may help to optimize ICD programming in daily clinical practice.
CONFLICTS OF INTERESTNone declared.
- –
Most of the VT detected in the VF zone can be terminated by ATP without the need for high-energy shocks. Several studies have demonstrated that empirically programming 1 ATP burst in the fast VT zone is highly effective in terminating fast VT. These studies have shown that ATP is able to reduce the need for high-energy shocks without increasing morbidity. The possibility of programming ATP bursts before and/or during capacitor charging in the VF zone was developed to avoid delay in high-energy shock administration if there is ATP failure while maintaining the potential for harmless VT termination in the VF zone.
- –
This study suggests that programming 1 ATP burst BC in addition to a standard burst DC is associated with a significant reduction in high-energy shocks in patients with fast VT in the VF zone. This type of programming does not seem to prolong episode duration and may avoid battery consumption. This strategy may help to optimize ICD programming in daily clinical practice.
.