Keywords
INTRODUCTION
The rapid increase in the incidence of cardiovascular disease (CVD), which has taken on epidemic proportions in developing countries,1,2 has led to debate as to whether findings from research in the developed world are applicable in the developing world.
The present article reviews a series of studies in the United States, Spain, Colombia, and Ecuador which suggest that the etiophysiopathology and the specific importance of risk factors for CVD, particularly metabolic syndrome and pregnancy induced hypertension, differ between developed and developing countries.
THE "EPIDEMIOLOGIAL TRANSITION"
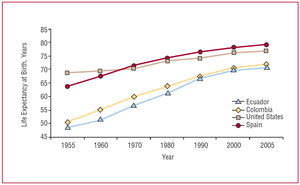
Differences in the epidemiological profile of diseases affecting developed and developing countries can be due to diverse geographical, environmental, demographic, socio-economic, and ethnic characteristics.3 Until a few years ago, the leading causes of death in developing countries, particularly in childhood, were malnutrition, tropical, and perinatal diseases (Table 1).4-6 Adequate control of these diseases has led to an increase in life expectancy in Ecuador from 48.4 to 70.8 years in 2005.7 In Colombia, life expectancy has increased from 55 to 72.2 years over the last 50 years.7 These data compare to increases in life expectancy in the United States and Spain from 68.9 to 77.1 and 63.9 to 79.3 years, respectively, for the same period (Figure 1).7 The ageing of Colombia's population is reflected in the fact that, in 1951, 2.8% of the population was aged 65 years or over compared to 4.4% in 1993.8
Figure 1. Changes in life expectancy at birth in Spain, the United States, Colombia, and Ecuador for the period 1955-2005. In the United States and Spain, life expectancy has stabilized in the last few decades after reaching a plateau at around 75 years. In the Andean countries, an increase in life expectancy can be observed for the same period.
Whilst the incidence of CVD is tending to stabilize or decrease in the developed world9-11 and prognosis is improving,12 in the developing world the incidence is increasing. Mortality data from Ecuador shows that over a period of barely 20 years, cerebrovascular disease rose from ninth to second place as a leading cause of death between 1975 and 1995.13 In the same year, hypertension (in third place), diabetes mellitus (DM) in fifth place, and acute myocardial infarction (AMI) in eighth place, also became some of the leading causes of death. Together, these 3 disease caused 3 times more deaths than pneumonia, which was the leading cause of death in 1995 (Table 1).13 A similar pattern has been observed in Colombia, where AMI, cerebrovascular accident, and DM caused 213 150 deaths (19.6%) over the period 1997-2001.8 In combination, mortality from CVD was greater than that from violent causes and CVD is among the 10 leading causes of death in both men and women (Table 2).14 The question that arises is what has caused this shift. Is it only increased access to health care and the quality of that care?
Several studies have looked at the epidemic behavior of CVD in underdeveloped countries.15,16 The INTERHEART study17 aimed to identify the effect of modifiable risk factors associated with a first AMI and included 12 461 patients with a first acute coronary event and 14 637 controls from 52 developed and developing countries, including Colombia. The study showed that a raised apo B/apo A1 ratio, smoking, diabetes, hypertension, abdominal obesity, psychosocial stress (calculated using a combination of scores relating to depression, stress in the workplace or at home, and financial stress) were all positively associated with having an AMI, while the adequate consumption of fruit and vegetables, moderate alcohol consumption, and exercise were all associated with a lower risk of having such an event. The study also showed that there were no significant differences in the prevalence of these risk factors between developed and developing countries.17 High-calorie, high-fat diets which are low in fiber have become commonplace in recent years in developing countries18 and this, coupled with the increasing physical inactivity which has accompanied urbanization, has helped to produce the increase in obesity, particularly abdominal obesity,19 which has been observed in Latin American countries (Figure 2).19-21 Abdominal obesity together with 2 other risk factors constitutes the metabolic syndrome (MS) which has been defined by the International Diabetes Federation (IDF)22 as: hypertension (>130/85 mm Hg), raised triglycerides (>150 mg/dL), reduced HDL cholesterol (HDL-C, <50 mg/dL in women and <40 mg/dL in men), and fasting plasma glucose >100 mg/dL.
Figure 2. Prevalence of overweight and obesity in different Latin American countries, Spain, and the United States. BMI indicates body mass index.
Recent studies have consistently shown that MS is associated with an increased risk of CVD and type 2 diabetes.23-25 It is also important to note the IDF's insistence on abdominal obesity as an essential element in the diagnosis of MS and their use of different cut points for waist circumference according to country and race.22,26
BIOLOGICAL MECHANISMS UNDERLYING THE METABOLIC SYNDROME
In Figure 3, we present a proposed general outline which relates socioeconomic factors to some of the biological mechanisms involved in the onset of MS. The response to the socioeconomic model imposed in Iberoamerican countries has been a massive migration from the countryside to industrialized urban centers. In Colombia, the process of urbanization has been further accelerated by the forced displacement of entire rural communities fleeing the armed conflict.27 Currently, over 70% of the population lives in urban centers.28 The process of urbanization is also a response to modernization and the attractions of the new, western lifestyle for rural populations.18
Figure 3. Mechanisms possibly participating in the genesis of metabolic syndrome and cardiovascular mortality in developing countries. Inequalities deriving from the consumerist society lead to rapid urbanization which causes profound changes in eating habits and physical activity. These in turn produce obesity, particularly abdominal obesity, which sets off a chain of physiopathological events leading to endothelial dysfunction and an increase in diseases such as hypertension, type 2 diabetes mellitus and metabolic syndrome. These contribute to the increase in mortality due to coronary events. IL-6 indicates interleukin-6; NADPHox, nicotinamide adenine dinucleotide phosphate oxidase; CRP, C-reactive protein; IR, insulin resistance; TNFα, tumor necrosis factor alpha.
Urbanization has been accompanied by radical modifications in lifestyle, including29,30:
1. A shift from a diet which is rich in vegetables, cereals, and fruit to a western, fast-food diet, with a high fat and calorie and low fiber content (hamburgers, french fries, pizza, soft drinks).
2. A reduction in physical activity associated with the mechanization of daily activities and changes in leisure activities, particularly in children. Thus, in cities, the washing machine, gas cookers, elevators, the subway, computers, and "Play Stations" have replaced the collection of firewood, the sowing and harvesting of food, and traditional games which required physical effort.
The result of these changes has been an increase in the prevalence of obesity, initially abdominal obesity. The populations of developing countries are often short in stature, probably as a result of having only limited nutritional resources for generations.31 They also present a characteristic phenotype, particularly among men, who are characteristically "short and tubby." Visceral adipocytes produce a low-grade chronic inflammatory state characterized by an increase in the circulating concentrations of interleukin-6 (IL-6), tumor necrosis factor-alpha (TNFα), and C-reactive protein (CRP).32,33 This low grade inflammation leads to dysfunction of the endothelial cells, which lose their vasodilatory, antithrombotic, and antiatherogenic properties34,35; this is apparently a widespread biological response in humans.36-39 The question then is why the populations of developing countries should be more sensitive to this process. We suggest that this is a result of the lower exposure time among the populations of developing countries to the new lifestyles associated with modernization. The shorter the exposure time, the less adapted the population, and the greater the risk of an inflammatory response at lower levels of abdominal obesity. This is in turn associated with an increased risk of type 2 diabetes and CVD. Figure 4 shows data which illustrate the positive relationship between plasma levels of inflammation markers and waist circumference in healthy individuals in Colombia and in individuals with hypercholesterolemia with and without MS. We have also reported that increased levels of inflammatory
Figure 4. Behavior of tumor necrosis factor alpha (TNFα and flow-mediated vasodilatation in healthy individuals and individuals with hypercholesterolemia with and without metabolic syndrome. Plasma levels of TNFα and flow-mediated vasodilatation, in healthy Colombian individuals and those with hypercholesterolemia with and without metabolic syndrome. Increases in TNFα levels parallel increases in waist circumference, while the endothelial function is significantly reduced. WC indicates waist circumference; MS, metabolic syndrome.
markers and increased risk of pregnancy induced hypertension and CVD are present in the Andean population at lower levels of abdominal obesity.40-42 We have also shown that the the leukocyte count and concentrations of ultrasensitive CRP were significantly greater in individuals with a waist circumference >88 cm,43 and that CRP concentration is a risk factor for essential hypertension and pregnancy induced hypertension in the Andean population.40-42 It is well-known that the Hispanic population in the United States and that the Hindu population in the United Kingdom are at greater risk for low-grade chronic inflammation, type 2 DM, and cardiovascular mortality than the Caucasian populations of those countries.36-39,44 However, it is currently not clear whether these differences are due to genetic or socioeconomic factors, as these groups migrated relatively recently to developed countries and have therefore only had a short exposure to risk factors and are anyway usually in lower socioeconomic categories. Although there are no data from studies which have specifically investigated this problem, we believe that length of exposure to the new living conditions generated by urbanization and modernity is an important risk factor for minority populations in developed countries.45-48
The recent large-scale migration of indigenous Ecuadorians to Spain provides an excellent opportunity to study this possibility. Amongst the population of Colombia, which includes a range of well-defined, different races, though also substantial intermixing between races, we did not find the marked differences in prevalence of MS between races that has been observed in developed countries.49,50 The Pima Indians provide a striking example of the relationship between environment and genetics: as indigenous Indians living in the United States and exposed to a consumer society lifestyle they experienced an explosive increase in obesity, MS, type 2 diabetes, and CVD, whilst the Pima Indians living in Mexico within a more traditional lifestyle did not experience this dramatic increase.45-48 At the same time, there have been important developments in epigenomics, or the study of the impact of environment in the expression of genes participating in the metabolism of nutrients and energy.51
HEALTH CARE INFRASTRUCTURE, INFECTION, AGEING AND CARDIOVASCULAR RISK
Although abdominal obesity is considered the most important risk factor for the low-grade chronic inflammation associated with the development of endothelial dysfunction, MS, atherosclerosis, type 2 DM, and CVD, it appears that the presence of other factors such as chronic infections, which are very frequent in developing countries due to inadequate health care systems, could also play a part.52,53 Several studies have shown that recent infection of the lower respiratory tract and the urinary tract increases the risk of CVD.54,55
In Iberoamerican countries, the bad habits and defects of the two worlds have collided: lack of potable water, defective waste and sewage removal, high rates of intestinal parasitism, non-preventable infections, and tropical diseases are all still present, but are now coupled with diets which are high in saturated fats and refined flours, more smoking, higher rates of physical inactivity, and obesity.56
In recent decades, the proportion of elderly has also increased.8 The ageing process involves greater activity of the renin-angiotensin system, a hormone which has 3 important effects in humans57-60:
1. It increases the oxidative stress in the vascular wall, which causes increased inactivation of oxygen free radicals and therefore alters the balance of these substances, leading to endothelial dysfunction.61
2. It blocks the insulin intracellular signaling routes, producing insulin resistance, hyperinsulinism, and an increased risk of hyperglycemia, MS and DM.
3. It stimulates the production of pro-inflammatory cytokines, such as TNFα, in adipocytes and endothelial cells. This in turn activates metalloproteinase 2, an enzyme which breaks down the stable atherosclerotic plaque, thereby producing an atherothrombotic profile which is key to the presentation of acute myocardial infarction.62
Altered endothelial function is essential to the development of atherosclerotic plaque, the pro-coagulant state, increased vascular tone, and arterial hypertension and insulin resistance, all of which are associated with MS and increased risk of CVD.34,35,63
METABOLIC SYNDROME: ETIOLOGICAL AND DIAGNOSTIC DIFFERENCES
In the populations of Colombia and Ecuador,43,64,65 there appears to be an increased risk of MS at a lower grade of abdominal obesity than that set out in the Third Panel on the Treatment of Adults in the United States' National Cholesterol Education Program (ATP-III).66 Among Colombian males serving in the army, it was found that a waist circumference of 88 cm had greater sensitivity and specificity than the 94 cm recommended in Caucasian subjects to identify individuals with the so-called atherogenic profile, a profile characterized by an increase in triglyceride levels, insulin and glucose, and low levels of HDL cholesterol (HDL-C).43 In male employees of the Ecuador Petrol Company, it was found that a waist circumference of 90 cm best identified individuals meeting other criteria for a diagnosis of MS.65 A cut-point of 90 cm had a sensitivity and specificity of 83.9% and 70.3%, respectively, with positive and negative predictive values of 60.2% and 88.6%, respectively. In contrast, when the threshold recommended by the ATP-III for North Americans (102 cm) was used, sensitivity was barely 23.2%, with a specificity of 96%.65 These results indicate that when diagnosing MS in these Andean populations it is more convenient to use the IDF criteria. We later demonstrated that 50% of individuals with a history cardio-cerebrovascular events (n=670) had a diagnosis of MS independently of the diagnostic criteria used (ATP-III or IDF),64 making discussion as to which criteria to use irrelevant in this population. However, in individuals with no prior history of cardio-cerebrovascular events (n=583), use of the IDF criteria led to a diagnosis of MS in 41.4% of those studied compared to 31.2% using the ATP-III criteria (P<.0001). At present, no prospective studies have been performed to determine whether a diagnosis of MS in these populations is associated with greater risk of CVD or DM2. In a recent study performed in Spain, Alegría et al67 determined that the raw prevalence of MS in the adult working population of Spain was 10.2%, and that it was higher in individuals with any type of fasting glucose alteration and in those with a higher body mass index.
Ford recently included data from cohort studies in the United States in a systematic review to estimate the relative risk for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome in the general adult population, and using the definitions of MS proposed by the ATP-III and the World Health Organization (WHO).23 Using the ATP-III definition, the combined relative risk was 1.2 (95% confidence interval [CI], 0.90-1.78) for all cause mortality, 1.6 (95% CI, 1.3-1.9) for cardiovascular disease, and 2.9 (95% CI, 1.9-4.5) for DM. The author concluded that, in the United States population, MS defined using the ATP-III or WHO criteria has limited predictive capacity for all-cause mortality or CVD, and that it is better at predicting development of type 2 DM.23 Recently, the same author showed that in 3601 North American adults of both sexes, the unadjusted prevalence of MS was 39.0% using the IDF criteria and 34.5% using the ATP-III definition.68 The difference was greater in American-Mexican males, who had an age-adjusted prevalence of 50% using the IDF criteria compared to 40.3% using the ATP-III definition. It had been previously shown that this group was at greater risk of developing type 2 DM and CVD.19,27 This group's socioeconomic conditions are poorer than those of other ethnic groups, and they have also lived in the United States for only a few years, and therefore have only been exposed to a highly consumerist society for a relatively short time.69 Katzmarzyk et al70 recently evaluated the ability of the ATP-III and IDF criteria to predict all-cause mortality and cardiovascular mortality in 20 789 non-Hispanic males. Mean age at study entry was 43.3 years, and the prevalence of MS at study commencement was 19.7% using the ATP-III criteria and 30.0% using the IDF criteria. A diagnosis of MS was associated with a relative risk (RR) of death from any cause 1.3 (95% CI, 1.1-1.6) when the ATP-III criteria were used and 1.2 (95% CI, 1.0-1.4) using the IDF criteria. The RR for death from CVD was 1.7 (95% CI, 1.3-2.3) using the ATP-III criteria and 1.6 (95% CI, 1.2-2.2) using the IDF criteria. To determine the impact of abdominal obesity on mortality, individuals with a waist circumference <94 cm and >102 cm were evaluated. A direct relationship was found between waist circumference and an increased RR of death from CVD, particularly in individuals who also had 2 or more metabolic risk factors (94-102 cm: 1.5; 95% CI, 1.0-2.3; >102 cm: 2.3; 95% CI, 1.5-3.4). In males over 18 years of age who participated in the National Health and Nutrition Examination Survey (NHANES), the prevalence of MS using the ATP-III definition was 24.3% and 38.6% using the IDF definition. The population attributable fraction for MS varied from 8.0% to 9.1% for all-cause mortality, and from 16.1% to 20.5% for mortality associated with CVD, whichever criteria were used. These data are similar to those reported recently in the Hoorn study24 which showed that a diagnosis of MS doubled the risk of CVD, regardless of which criteria were used to define MS.
Lawlor et al71 analyzed data from a cohort of 3589 British women aged 60-79 with no history of CVD, and reported the prevalence of MS to be 48% using the IDF criteria and 29% using the ATP-III criteria. The age-adjusted RR for MS was similar using the IDF and ATP-III criteria. The authors found that, using either of the definitions, MS showed a modest association with risk of CVD; after correcting for smoking, physical inactivity, and socio-economic position, the association decreased to 1.25 and 1.27, respectively. The authors concluded that MS is only weakly associated with CVD risk and questioned the importance of MS as a risk factor for CVD. With regard to the proposal set out here for a socio-economic pathology, it is interesting to note that the most important confounding factor in the association between MS and CVD risk was socio-economic position. This factor was more important than smoking and physical inactivity, not only in terms of attenuating the impact of MS on CVD risk, but also in terms of reducing the linear association between CVD risk and insulin resistance, triglyceride levels, HDL-C, and the waist-hip ratio. Other studies have shown that MS prevalence is inversely related to socio-economic level, although statistical significance was not reached.67
Our studies in Colombia and Ecuador, although cross-sectional in design, support the IDF notion of the MS as clinically useful and suggest that health-care teams in those countries should use it to help identify individuals who could benefit from multifactorial preventive programs to reduce the risk of CVD and type 2 DM. The differences with results from North America, the United Kingdom, and Spain may be due to the socio-economic differences between those countries and the Andean populations covered in our studies. The idea that the interaction between socio-economic conditions and the classic cardiovascular risk factors depends on the degree of development of a given society and the length of exposure to the consumer society, and that it is this interaction that determines the overall degree of risk for CVD, is what we have proposed should be called the "socioeconomic pathology," to differentiate it from the study of individual risk factors in isolation.
REGIONAL DIFFERENCES IN THE ONSET OF PREGNANCY INDUCED HYPERTENSION
Pregnancy induced hypertension (PIH) has physiopathological characteristics which are similar to those of atherosclerosis and CVD but, unlike them, it has a rapid onset and evolution, with clinical manifestations appearing during the second half of the pregnancy and resolving abruptly after childbirth.72 There are enormous differences between developed and developing countries in the incidence of PIH and its contribution to maternal mortality. Mortality in the USA and Europe is 10 per 100 000 live births, in Latin America it is 220 per 100 000 live births and in Africa it is 430 per 100 000 live biths.73 These figures appear to be determined by the marked socio-economic differences, and by the deficient health-care systems and sanitary conditions in developing countries coupled with fact that nutritional resources, especially of dietary minerals, are inadequate to meet the greater demand occasioned by the growth of the fetus.72,74-76 The level of socio-economic development in developed countries means that adequate prenatal control is available for most women during pregnancy. This includes the early diagnosis and treatment of urinary, vaginal and oral infections, as well as access to an adequate diet and the necessary mineral and vitamin supplements.74 In Ecuador and Colombia, a high proportion of women do not have access to adequate prenatal control, and infections and diet deficiencies are neither detected nor corrected. This is a socioeconomic pathology which leads to a high risk of PIH and maternal mortality.72 In these Andean countries, early diagnosis and effective treatment of sub-clinical vaginal and urinary infections during pregnancy, and adequate dietary supplements with calcium and linoleic acid, reduce the risk of PIH to levels similar to those observed in developed countries.77-82 When nutritional and infectious factors have been controlled in these women, obesity, dysglycemia, and dyslipidemia become the main risk factors for preeclampsia (PE).77,78 Thus, about 95% of the risk for PIH in Colombian and Ecuadorian women could be controlled by diagnosing and curing oral, urinary and vaginal infections, assuring an adequate intake of macronutrients and vitamin and mineral supplements, and by using diet and physical exercise to control excess weight gain and lipid and glucose alterations.72 The remaining 5% of risk for PIH may be due to genetic and immunologic factors, including polymorphic alterations in the nitric oxide synthase gene, which is important in these countries.83 Further support for the proposal set out here is provided by the fact that in the populations of Colombia84 and Ecuador,85 the levels of asymmetric dimethylarginine (ADMA), an endogenic inhibitor of nitric oxide synthase, plays no part in the development of PIH, whilst several European studies demonstrated that ADMA plays an important role in PIH.86,87 The difference may be due to environmental factors, such as malnutrition and infections, which reduce the impact of ADMA as a risk factor for PIH in Colombian and Ecuadorian women. On the basis of these findings, we propose that the fundamental cause of the increased risk for PIH among populations of developing countries are the social and economic inequalities which impede the provision of adequate health care and prenatal control. This in turn would explain the enormous regional differences seen in the incidence and mortality due to PIH.72
HYPOTHESES AND PERSPECTIVES
The current epidemic of obesity, DM and CVD in developing countries appears to be a natural human biological response to the imposition of lifestyles for which we are not particularly well adapted. Our proposal is that the differences in the patterns of CVD morbimortality rates between the developed and the developing world are dependent on the length of exposure to the socio-economic pathology and the degree of adaptation to that pathology. If this proposal, which requires further study, is confirmed, it could lead to fundamental changes in health policy and preventive programs for CVD and type 2 DM, for example by taking into account that diagnostic criteria and preventive and treatment strategies should not necessarily be uniform in populations with different levels of socioeconomic development and in which there are enormous social and economic inequalities. For Iberoamerican countries, the big challenge will be to carry out large-scale, prospective research which will allow them to develop their own diagnostic criteria and the most useful preventive and therapeutic strategies. The recent large-scale migrations of native Ecuadorians to Spain will provide an interesting model for the study of the interaction between genetics and environment, and will have important repercussions for the Spanish health care system.
COLCIENCIAS provided financial support for project 6566-04-12914.
Correspondence: Dr. P. López-Jaramillo.
Instituto de Investigaciones. Fundación Cardiovascular de Colombia.
Calle 155.a, n.° 23-58. Tercer piso. Floridablanca. Santander. Colombia.
E-mail: jplopezj@fcv.org