The findings of the 2011 Spanish Catheter Ablation Registry are presented.
MethodsData were collected in two ways: retrospectively using a standardized questionnaire, and prospectively from a central database. Each participating center selected its own preferred method of data collection.
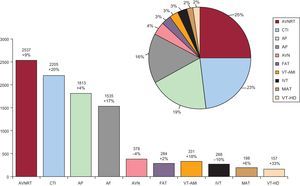
ResultsSixty-six Spanish centers voluntarily contributed data to the survey. Some 9662 ablation procedures were analyzed, averaging 146 (104) per center. The three main conditions treated were atrioventricular nodal reentrant tachycardia (n=2537; 26%), typical atrial flutter (n=2205; 23%) and accessory pathways (n=1813; 19%). Atrial fibrillation was the fourth most common substrate treated (n=1535; 16%) and showed a slight increase over figures for 2010. Ventricular arrhythmia ablation has increased considerably. The overall success rate was 94%; major complications occurred in 2.2% and overall mortality was 0.04%.
ConclusionsData from the 2011 registry show a continued increase in the number of ablations performed with a generally high success rate and few complications. The use of complex substrate ablation continues to grow.
Keywords
.
IntroductionThis is the Spanish Catheter Ablation Registry for 2010. Its publication completes 11 years of uninterrupted activity on the part of the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 The registry covers all of Spain, is voluntary, and is published annually. The participants include most Spanish electrophysiology laboratories, making it one of the few large-scale observational catheter ablation registries.
Since it started, the registry's objectives have been to observe and describe developments in interventional treatment of cardiac arrhythmias in Spain and provide reliable information on the type of activity undertaken and the facilities available at arrhythmia units. Thanks to its uninterrupted publication, we have been able to determine prospectively the developments in ablation procedures in Spain over the last decade.
MethodsData collection involves a choice between two approaches, both of which have been available since the registry began; one is prospective, the other, retrospective. The retrospective method has always been the most commonly used. This involves completing a questionnaire sent to all interventional electrophysiology laboratories in January and available on the Working Group website (www.arritmias.org). The prospective method uses a standardized database which is provided by the registry and requires patients be added individually. Whichever system is used, data remain completely anonymous—even to registry coordinators—and the Spanish Society of Cardiology guarantees participating centers cannot be identified.
The information collected relates to equipment and personnel in arrhythmia units, procedures performed, and demographic characteristics of patients. As in previous years, human resource data only correspond to public-sector centers and the epidemiological variables presented only correspond to patients from centers submitting data prospectively.
We analyzed the same 10 arrhythmia substrates as in previous years: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways (AP), atrioventricular node (AVN) ablation, focal atrial tachycardia, cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia, atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia (VT) associated with postinfarction scarring (VT-AMI), and VT associated with nonischemic heart disease (VT-NAMI). We analyzed a series of variables common to all substrates, including number of patients and procedures performed, success rate, type of ablation catheter used, and number and type of procedure-related complications, including periprocedural death. We also collected a series of specific variables for certain substrates. These included the anatomical location of AP, the location and mechanism of atrial tachycardia, and VT type.
As in previous registries, the success rate is based on end-of-procedure data. We cannot determine the recurrence rate because follow-up is not analyzed. As different therapeutic approaches with different objectives are used for the AF and VT-AMI substrates, success/failure criteria may vary as a function of technique. Hence, these substrates are excluded from our analysis of the overall success of ablation procedures. For all substrates, only ablation-related complications occurring during postprocedure hospitalization were reported.
Statistical AnalysisQuantitative variables are presented as mean (standard deviation). Differences between quantitative variables were assessed using the Student t test for dependent and independent variables, as appropriate. Differences between categorical variables were measured using the chi-square test and the Fisher exact test. We considered P<.05 statistically significant. Statistical analysis was performed using an SPSS 15.0 database.
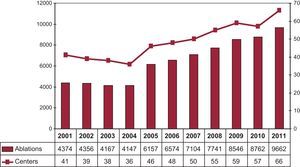
ResultsIn all registries, except in 2010, the number of participating centers (Appendix) has exceeded that of the previous year. This year has been no exception, with a noteworthy 16% increase (Figure 1). Of the 66 centers, 54 (82%) belong to the public health care system and 12 are private. The retrospective data collection system was once again the preferred method. Only 8 centers (12%) collected data prospectively.
Figure 1. Change in the number of centers participating and procedures recorded in the Spanish Catheter Ablation Registry.
Most of the participating centers are tertiary (88%) and university (70%) hospitals. Data was reported by the cardiology department in all cases; 71% of centers offered cardiac surgery (Table 1).
Table 1. Characteristics and Infrastructure of the 66 Electrophysiology Laboratories Participating in the 2011 Registry.
| no. % | |
| University hospitals | 46 (70) |
| Level | |
| Tertiary | 58 (88) |
| Secondary | 8 (12) |
| Health care system | |
| Public | 54 (82) |
| Fully private | 12 (18) |
| Department responsible | |
| Cardiology | 66 (100) |
| Cardiac surgery | 47 (71) |
| Availability of laboratory | |
| Exclusive use | 47 (71) |
| Days electrophysiology lab available (median) | 4 |
| Digital polygraphy | 66 (100) |
| Digital radiology | 50 (76) |
| NFNS * | 56 (84) |
| Magnetic navigation | 3 (4.5) |
| Robot navigation | 1 (1.5) |
| Cryoablation | 26 (39.5) |
| Intracardiac echocardiography | 20 (30) |
| Device implantation | |
| No | 17 (26) |
| ICD | 4 (6) |
| ICD and pacemaker | 43 (65) |
| Scheduled ECV | |
| No | 20 (30.3) |
| ECV | 33 (50) |
| ICV | 1 (1.5) |
| ECV and ICV | 12 (18.2) |
ECV, external cardioversion; ICD, implantable cardioverter-defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
* At least one NFNS.
As in previous registries, epidemiologic characteristics were only available for data collected prospectively. In 2011, 8 centers used this method (1 more than in 2010), with 1544 ablation procedures (16% of the total).
Patient mean age was 42 (13) years. The youngest patients were those undergoing AP ablation (34 [14] years) and the oldest were those undergoing AVN ablation (72 [7] years). Predominantly women underwent AVNRT ablation (73%); AF (71%) and VT (69%) ablation (associated or not with structural heart disease) were predominantly performed on men. These data are practically identical to those reported in previous registries.6, 7, 8, 9, 10 Similarly, 36% of patients had a history of structural heart disease whereas presence of left ventricular dysfunction was generally limited to patients undergoing AVN ablation and VT ablation associated with heart disease. The same distribution was observed in implantable automatic defibrillator recipients.
Infrastructure and ResourcesTable 1, Table 2 show the technical and human resources available in laboratories participating in the registry, as well as their activities.
Table 2. Change in Human Resources in Public Hospital Laboratories Participating in the Registry Since 2003.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
| Staff physicians, no. | 2.2 | 2.2 | 2.2 | 2.3 | 2.4 | 2.5 | 2.6 | 2.8 | 2.6 |
| Full-time physicians, no. | 1.4 | 1.6 | 1.7 | 1.8 | 2.1 | 2.1 | 2.1 | 2.3 | 2.2 |
| Fellowship students/year, no. | 0.6 | 0.7 | 0.6 | 1.3 | 0.6 | 0.6 | 0.8 | 0.75 | 0.7 |
| RN, no. | 1.6 | 1.6 | 1.7 | 1.7 | 2 | 2.2 | 2.2 | 2.4 | 2.3 |
| TAR, no. | 0.2 | 0.2 | 0.2 | 0.3 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 |
RN, registered nurse; TAR, technical assistant radiologist.
A total of 47 centers (71%) had ≥1 laboratory exclusively dedicated to electrophysiology and 7 centers (11%) had 2. As in previous years, the laboratory was available for a mean 3.9 (1.4) days/week (median, 4). Only 3 of the 12 private centers has a laboratory exclusively dedicated to electrophysiology.
External electric cardioversion was performed in 68% of laboratories and internal cardioversion in 20%. Most laboratories (74%) are also equipped for cardiac pacing device implantation—mainly of defibrillators. In 65% of laboratories, both defibrillators and pacemakers are implanted; only defibrillators are implanted in 6%, and only pacemakers in 3%.
All centers can conduct digital polygraphy, 76% digital radiology, and 54.5% portable fluoroscopy. One nonfluoroscopic navigation system (NFNS) is available in 84% of centers; 19 centers have 2, and 1 center has 3. Some 94.6% of public centers have an NFNS vs only 42% of private centers.
The number of remote navigation systems has remained stable since 2008. Only 3 centers have a magnetic navigation system and 1 has a robot navigation system. The number of centers offering intracardiac echocardiography has also remained stable (20). Echocardiographic ablation continues to be available at just 1 center; the use of cryoablation is slowly expanding (it is now available in 26 centers).
Slight changes have taken place in the health care staff dedicated to electrophysiology laboratories. Some 72% of centers have >1 full-time physician and 37% have >2. Two healthcare centers have as many as 5 full-time staff physicians. Some 83% of laboratories have ≥2 full-time registered nurses. Some 24 centers have fellowship students (vs 20 in 2010) and, among these centers, the mean is 1.75 per center (1 hospital has 6).
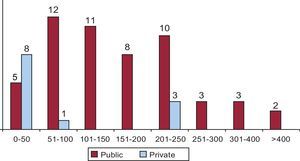
ResultsIn 2011, 66 centers have submitted data. This constitutes the highest level of participation since the registry began (Figure 1, Figure 2). Some 9662 ablations have been reported, which represents a mean of 146 (104) procedures/center (median, 126 [range, 4-491]). Only 4 of the private centers performed >50 ablations/year; 3 of these performed >200 procedures. Five public centers performed >300 ablations; 2 of these performed >400.
Figure 2. Number of electrophysiology laboratories in the Spanish Catheter Ablation Registry by number of ablation procedures performed during 2011.
Excluding AF and VT-AMI substrate ablations, the overall success rate was 94% (7389/7840). The number of complications reported for all procedures (including AF and VT-AMI ablations) was 211, which represents 2.2%. Four deaths (0.04%) were reported: 2 patients with AF ablation (1 secondary to cardiac taponade, 1 thrombotic occlusion of the left main coronary artery), 1 VT-AMI ablation (due to electromechanical disassociation), and 1 AP ablation (due to aortic rupture at 48h postprocedure in a patient with Ehler-Danlos syndrome). Iatrogenic atrioventricular (AV) block occurred in 13 patients (0.13%) who required permanent pacemaker implantation: 5 during AVNRT ablation, 4 during AP ablation, 2 during VT-NAMI ablation, and 2 during VT-AMI ablation.
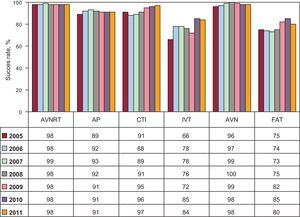
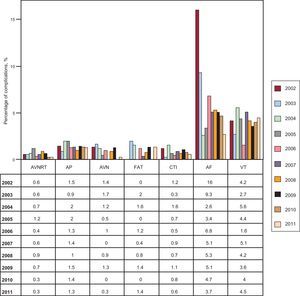
Figure 3, Figure 4 show overall results in terms of success and complication rates, and compare these with previous years. Percentage success rates for the different substrates remain stable, except for IVT (for which they have improved markedly). Incidence of complications has remained stable for all substrates except AF, for which they have fallen from 16% in 2002 to 2.7% in 2011.
Figure 3. Change in percentage success rates for catheter ablation since 2005 by substrate treated. AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT: focal atrial tachycardia; IVT, idiopathic ventricular tachycardia.
Figure 4. Percentage of complications in catheter ablation since 2002 by substrate treated. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
The most frequently treated substrate is AVNRT, followed by CTI and AP (Figure 5). The number of procedures has increased for all substrates except AVN and IVT. The number of AF procedures has increased by 17% with respect to 2010 and accounts for 16% of the total (AF is the fourth most frequently treated substrate). The least treated substrate continues to be VT-NAMI, although in the last 2 years the number of procedures has increased considerably.
Figure 5. Relative frequency of different conditions treated by catheter ablation in Spain during 2011. For each substrate, we show the percentage change with respect to the 2010 registry. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with acute postinfarction myocardial scarring; VT-HD, ventricular tachycardia associated with heart disease.
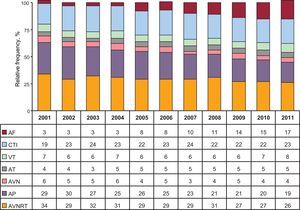
Changes in the relative frequency of the substrates treated since 2001 are shown in Figure 6. In the last decade, AVNRT ablation and AP ablation have fallen whereas AF ablation has increased.
Figure 6. Change in the relative frequency of different conditions treated since 2001. AF, atrial fibrillation; AP, accessory pathways; AT, atrial tachycardia; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
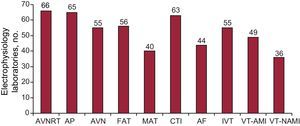
In 2011, AVNRT is the only substrate treated in all centers, followed by AP (98.5%) and CTI (95.5%) (Figure 7). The substrate treated by the fewest centers continues to be VT-NAMI (54.5%). The number of centers performing AF ablation has risen from 40 to 44, which represents 67% of all centers and 72% of public sector centers.
Figure 7. Number of electrophysiology laboratories participating in the Spanish Catheter Ablation Registry that treat each of the substrates. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute postinfarction myocardial scarring; VT-NAMI, ventricular tachycardia not associated with acute postinfarction myocardial scarring.
The following sections analyze the data for each arrhythmic substrate.
Atrioventricular Nodal Reentrant TachycardiaThis was the most commonly treated substrate and ablation was performed in all centers. A total of 2537 ablations were performed, 26.3% of all procedures. The mean number of AVNRT procedures/center was 38 (24), range, 2 to 122. The success rate was 98.4% (2496/2537), and 39 centers (59%) achieved 100% success. Complications occurred in 8 cases (0.3%): 5 patients (0.2%) presented AV block requiring permanent pacemakers; 2, vascular access complication; 1, pericardial effusion with taponade.
The most commonly used ablation catheter was the conventional 4-mm tip radiofrequency catheter and there was a slight decrease in the use of other catheters. In this context, the drastic increase in the use of 8-mm tip catheters by comparison with the 2010 registry is astonishing (60 vs 22), as is the decline in the use of irrigated tip catheters (13 vs 92). The use of cryoablation catheters has remained stable (67 procedures).
Cavotricuspid IsthmusThe second most frequent procedure was CTI ablation. A total of 2205 ablation procedures were performed (mean 33 [25]). These were successful in 2139 cases (97%); 63 of the 66 centers (95.5%) treated this substrate; 27 centers reported 100% success. Major complications occurred in 15 cases (0.7%): 13 patients presented vascular complications and there was 1 episode of heart failure and 1 stroke.
Use of the 4-mm tip ablation catheter was rare (4.9%) in this substrate. Irrigated tip catheters were used in 1171 procedures, 8-mm tip catheters in 935, and cryoablation catheters in 11.
Accessory PathwaysThis was the third most frequently treated substrate. A total of 1813 AP ablation procedures were performed in 65 hospitals, with a mean of 27 (17) procedures/center (range, 1-78). There were 1644 successful procedures (90.7%) and only 9 of the 57 centers that performed >10 AP ablations reported 100% success. Major complications occurred in 21 cases (1.2%): 11 patients presented vascular complications; 3, pericardial effusion; 2, myocardial infarction (1 due to dissection of the anterior descending artery); 4, AV block requiring permanent pacemaker implantation; and there was 1 death. Vascular complications included 1 case of significant aortic regurgitation and 1 aortic rupture at 48h postprocedure in a patient with Ehler-Danlos syndrome, which was the cause of the 1 recorded death.
Conventional ablation catheters were not used in 242 cases (13.3%). Irrigated tip catheters were used in 137 procedures, 8-mm tip catheters in 61, and cryoablation catheters in 42.
The ablated AP location was reported in all cases. As in previous registries, the most frequent locations were the left ventricular free wall (55%) and the inferior paraseptal pathways (23.2%). The locations least-often treated continued to be the peri-Hisian or superior paraseptal pathways (7.2%). Procedure success depended on AP location: 93.4% (931/997) success was reported for ablations in the left free wall, 88.7% (252/284) for the right free wall, 80.8% (105/130) for the peri-Hisian or superior paraseptal pathways, and 87.4% (368/421) for the inferior paraseptal pathways.
Atrioventricular Node AblationThis substrate continues to be fourth in the number of procedures per year. The total number of procedures was 378; 98.4% were successful, with only 1 vascular complication.
Conventional ablation catheters were not used in 74 cases: 8-mm tip catheters were used in 40 procedures and irrigated tip catheters in 34. This year, as in 2010, cryoablation catheters were not used in the treatment of this substrate.
Focal Atrial TachycardiaA total of 284 focal atrial tachycardia ablation procedures were performed, with a success rate of 83.5% (237/284) and a mean of 4.3 procedures per center. This substrate was treated in the right atrium in 53 centers but in the left atrium in only 37 centers. The origin of focal atrial tachycardia was reported in all cases and the procedure success rate was higher for those originating in the right atrium, 87.6% (169/193), vs 75.6% (68/90) for those in the left atrium.
Complications occurred in 4 cases (1.4%): 2 patients presented pericardial effusion and 2 had vascular complications.
More special catheters were used in 2011 than in 2010: 119 vs 77. In 95 of these cases irrigated tip catheters were used; in 8, cryoablation catheters; and in 16, 8-mm tip catheters.
Macroreentrant Atrial Tachycardia/Atypical Atrial FlutterThis substrate was treated in 40 centers (60%), with a total of 198 procedures (mean, 5 [range, 1-13] procedures/center). The procedure was successful on 151 occasions (76%). Complications occurred in 5 cases (2.5%): 3 patients presented femoral vascular complications; 1, cardiac taponade; and 1, acute pulmonary edema.
The origin of macroreentrant atrial tachycardia was reported for all procedures: 106 right-origin and 92 left-origin cases; success rates were 81% and 70%, respectively. Catheters other than the conventional 4-mm tip were used in 80% of cases, most of them irrigated tip catheters (87%) and the rest 8-mm tip catheters (13%).
Atrial FibrillationIn total, 1535 AF ablation procedures (range, 4-128) were performed in 44 (66.6%) of the participating centers. This represents a mean 33 procedures/center, although 10 laboratories performed <10 procedures and 23 performed <25 ablations. Eight centers performed >50 AF ablations and 4 of these performed >100 procedures.
The treatment technique used was indicated in 1534 procedures (99%). Ostial electrical disconnection was performed in 17% of cases; circumferential isolation with disconnection in 80%; and circumferential isolation with discharge reduction in the remaining 3%. In 27 procedures, the vena cava superior was electrically disconnected.
Almost all centers (88.5%) used irrigated tip ablation catheters. A total of 110 (7%) cryoenergy balloon ablation procedures were performed; 19 used single-shot technology (Pulmonary Vein Ablation Catheter, PVAC™, Ablation. Frontiers, Carlsbad, California, United States) and 48 (3%) used 8-mm tip catheters.
Complications were reported in 57 cases (3.7%): significant pericardial effusion/cardiac tamponade (33); acute coronary syndrome (2); vascular access (15); stroke (4); phrenic nerve palsy (1); pulmonary vein stenosis (1); and pulmonary hemorrhage (1). Two deaths (1.3/mil) were reported: 1 due to thrombotic occlusion of the left main coronary artery and the other due to cardiac taponade complicated by multiorgan failure.
Idiopathic Ventricular TachycardiaA total of 268 IVT ablation procedures were reported for 55 centers (mean, 4.8 [range, 1-22] ablations/center). Success was achieved in 224 procedures (83.5%) and only 5 (1.8%) complications were reported: 3 cases of tamponade and 2 of femoral pseudoaneurysm.
The type of VT ablated was reported for 268 procedures: 170 occurred in the right ventricular outflow tract and 47 in the left ventricular outflow tract; 26 were fascicular and 25 were reported as “other location”. Success rates for these procedures were 84%, 85%, 84%, and 76%, respectively.
The 4-mm tip catheter was used in 51% of cases, irrigated tip catheters in 48%, and 8-mm tip catheters in the remaining 1%.
Ventricular Tachycardia Associated With Postinfarction ScarringA total of 49 (74%) centers performed 331 VT-AMI ablation procedures (6.7 [range, 1-34] ablations/center). The complications reported (n=19; 5.7%) were vascular access (8); cardiac tamponade (7); stroke (1); heart failure due to aortic valve damage (1); and complete AV block (2). One patient died after cardiac tamponade due to electromechanical disassociation.
The type of ablation performed was reported in all cases: 63 used a “conventional” approach and 268 used a substrate approach. Irrigated tip ablation catheters were used for these ablation types in practically all cases.
The success rate reported for the conventional approach (noninducibility of clinical tachycardia after ablation) was 85.7%.
Only 3 epicardial procedures have been reported, 2 of which were successful.
Ventricular Tachycardia Not Associated With Postinfarction ScarringA total of 157 ablation procedures were performed for this substrate in 36 laboratories (54.5%).
The VT types ablated were: arrhythmogenic cardiomyopathy (31); branch-branch (11); non-ischemic dilated cardiomyopathy (69), and “other” (46). Success rates were 90%, 91%, 72%, and 82%, respectively. Nine procedures were epicardial; 8 of these were immediately successful. Complications occurred in 4 cases, 2 with taponade and 2 with complete AV block.
Irrigated tip ablation catheters were used in 78% of procedures and 4-mm tip catheters in the rest.
DiscussionThe 2011 ablation registry saw an increase in the number of participating centers, making it increasingly representative of the current situation in Spain. Some 66 centers have taken part, surpassing the 59 centers that contributed in 2009–our record to date. Although the mean number of procedures/center has fallen slightly, a total of 9662 procedures has been reached, which more than surpasses the 8762 ablations recorded in 2010.
The trend to increase staff dedicated to electrophysiology laboratories seen in 2010 has not been maintained and figures have fallen back to the levels of 2009. The total number of fellowship students continues to fall slightly, although the number of centers with students in training has increased marginally. Exclusive dedication of the electrophysiology laboratory occurs principally in public sector centers.
The percentage of laboratories with access to an NFNS has held steady at the 2009 level of around 80%. The number of centers with magnetic or robot navigation has not increased.
As the number of ablations has risen considerably in 2011 (by 11.3% with respect to 2010), there has been a corresponding increase in the number of cases of each substrate. However, the 4 substrates that have increased most are VT-NAMI (33%), CTI (20%), VT-AMI (18%) and AF (17%). As in recent years, AF ablation continues to increase in number, growing more rapidly than the total number of procedures. However, the number of centers performing >50 AF procedures per year has decreased by 1. Circumferential isolation with disconnection as the objective is the technique most often used by participating centers. The rate of complications associated with AF ablation continues to fall and in 2011 is <4% for the first time.
Treatment of ventricular arrhythmias associated with heart disease continues to increase but, in contrast to 2010, IVT ablations did not increase. In VT-AMI ablation, the substrate approach is four times more common than the “conventional” approach. The reported number of cases of epicardial approach to VT remains low.
Hence, as we said in 2010, the “nonconventional” substrate procedures—such as AF or ventricular arrhythmias—continue to increase.
The use of irrigated tip catheters also continues to increase. These are the most commonly used catheters in treating the AF, macroreentrant atrial tachycardia, VT-AMI and VT-NAMI substrates. The use of the cryoenergy balloon in AF ablation has increased but remains a minority option.
ConclusionsAs in previous years, the Spanish Catheter Ablation Registry contains one of the largest samples of ablation procedures reported in international publications, surpassing the 9500 ablations performed last year. Ever more complex substrates are treated, maintaining the very high success rate with low rates of complication and mortality.
Once again, increases in the number and complexity of the ablations performed have not been translated into increases in the number of healthcare staff dedicated to this technique.
Conflicts of interestNone declared.
Acknowledgements
The coordinators of the registry would like to express their thanks to all participants in the 2011 Spanish Catheter Ablation Registry who voluntarily and disinterestedly submitted the data on the procedures they performed. They also wish to thank Ignacio García-Bolao—one of the registry coordinators until 2010—and Cristina Plaza, for their excellent, untiring, administrative work.
Appendix. Electrophysiology Laboratories That Participated in the 2011 Spanish Catheter, by Autonomous Community and Province (the name of the doctor responsible for the registry is given in parentheses)| Andalusia | Córdoba: Hospital Reina Sofía (Dr. F. Mazuelos); Granada: Hospital Virgen de las Nieves (Dr. M. Álvarez); Huelva: Hospital Blanca Paloma (Dr. P. Moriña), Hospital Juan Ramón Jiménez (Dr. P. Moriña); Jaén: Complejo Hospitalario (Dra. R. Cózar); Málaga: Hospital Quirón (M. Álvarez), Hospital Virgen de la Victoria (Dr. A. Barrera); Sevilla: Hospital Nisa Aljarafe (Dr. E. Díaz Infante), Hospital Virgen Macarena (Dr. E. Díaz Infante), Hospital Virgen del Rocío (Dr. A. Pedrote), Hospital Nuestra Señora de Valme (Dra. D. García Medina) |
| Aragon | Zaragoza: Hospital Lozano Blesa (Dr. G. Rodrigo), Hospital Miguel Servet (Dr. A. Asso), Clínica Quirón (Dr. A. Asso) |
| Canary Islands | Las Palmas: Hospital Dr. Negrín (Dr. E. Caballero), Hospital Insular (Dr. F. Segura), Clínica Santa Catalina (Dr. J.C. Rodríguez Pérez); Tenerife: Hospital Nuestra Señora de La Candelaria (Dr. R. Romero), Hospital Universitario de Canarias (Dr. A. Rodríguez) |
| Cantabria | Hospital Marqués de Valdecilla (Dr. F. Rodríguez) |
| Castile-La-Mancha | Toledo: Hospital Nuestra Señora del Prado (Dr. A. Macías), Hospital Virgen de la Salud (Dr. P. Calderón) |
| Castile and León | Burgos: Complejo Asistencial (Dr. F.J. García); Leon: Hospital de León (Dra. M.L. Fidalgo); Salamanca: Hospital Clínico Universitario (Dr. J.L. Moríñigo); Valladolid: Hospital del Río Hortega (Dr. B. Herreros); Hospital Clínico Universitario (Dr. J. Rubio) |
| Catalonia | Barcelona: Hospital de Bellvitge (Dr. X. Sabaté), Hospital Clínic (Dr. L. Mont), Hospital Germans Trias i Pujol (Dr. O. Alcalde), Hospital del Mar (Dr. J. Martí), Hospital de la Santa Creu i Sant Pau (Dra. C. Alonso), Hospital Sant Joan de Déu (Dra. G. Sarquella Brugada), Hospital Vall d’Hebron (Dra. N. Rivas), Hospital Mútua de Terrassa (Dra. S. Ibars), Clínica Dexeus (Dr. A. Moya), Clínica Pilar San Jordi (Dr. J. Brugada), Clínica Sagrada Família (Dr. A. Moya), Clínica Teknon (Dr. E. Rodríguez) |
| Community of Madrid | Fundación Jiménez Díaz (Dr. J.M. Rubio), Hospital 12 de Octubre (Dr. R. Salguero), Hospital Gregorio Marañón (Dr. A. Arenal), Hospital La Paz (Dr. R. Peinado), Hospital Puerta de Hierro (Dr. I. Fernández Lozano), Hospital Ramón y Cajal (Dr. R. Matía), Hospital Clínico San Carlos (Dr. N. Pérez Castellano), Hospital de Getafe (Dr. A. Pastor), Grupo Hospitales de Madrid (Dr. J. Almendral), Fundación Hospital Alcorcón (Dr. E. Esteban) |
| Chartered Community of Navarre | Clínica Universitaria de Navarra (Dr. I. García Bolao), Hospital de Navarra (Dra. N. Basterra) |
| Valencian Community | Alicante: Hospital General (Dr. J.G. Martínez), Hospital de San Juan (Dr. J. Moreno); Castellón: Hospital General (Dr. E. Domínguez); Valencia: Hospital Clínico (Dr. A. Martínez) |
| Extremadura | Badajoz: Hospital Infanta Cristina (Dr. M. Doblado) |
| Galicia | A Coruña: Hospital Universitario de A Coruña (Dra. L. Pérez), Hospital Clínico Universitario de Santiago (Dr. J.L. Martínez Sande) |
| Balearic Islands | Mallorca: Clínica Rotger (Dr. X. Viñolas), Hospital Son Llàtzer (Dr. X. Fosch) |
| Basque Country | Vizcaya: Hospital de Cruces (Dr. A. Bodegas), Hospital de Basurto (Dra. M.F. Arcocha); Álava: Hospital Txagorritxu (Dr. J. Pindado) |
| Principality of Asturias | Hospital Central de Asturias (Dr. J.M. Rubín) |
| Region of Murcia | Hospital Santa María del Rosell (Dr. I. Gil), Hospital Virgen de la Arrixaca (Dr. A. García Alberola) |
Received 30 May 2012
Accepted 3 June 2012
Corresponding author: Valladares 3, 1. C, 41010 Sevilla, Spain. erdiazin@gmail.com