This article presents the findings of the 2012 Spanish Catheter Ablation Registry.
MethodsData were collected in 2 ways: retrospectively using a standardized questionnaire, and prospectively using a central database. Each participating center selected its own preferred method of data collection.
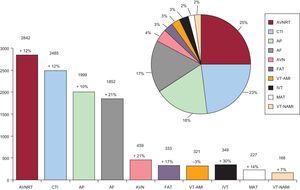
ResultsSeventy-four Spanish centers voluntarily contributed data to the survey. A total of 11 042 ablation procedures were analyzed, averaging 149 (103) per center. The 3 main conditions treated were atrioventricular nodal reentrant tachycardia (n=2842; 25.7%), cavotricuspid isthmus (n=2485; 23%), and accessory pathways (n=1999; 18%). Atrial fibrillation was the fourth most common substrate treated (n=1852; 17%), representing a slight increase. The number of ventricular arrhythmia ablation procedures was similar to that of 2011, but there was a decrease in procedures for ventricular tachycardia associated with postinfarction scarring. The overall success rate was 94.9%, major complications occurred in 1.9%, and the overall mortality rate was 0.04%.
ConclusionsData from the 2012 registry show that the number of ablations performed continued to increase. Overall, they also show a high success rate and a low number of complications. Ablation of complex substrates continued to increase, particularly in the case of atrial fibrillation.
Keywords
.
INTRODUCTIONWe present the Spanish Catheter Ablation Registry for 2011. Its publication completes 12 years of uninterrupted activity by the Spanish Society of Cardiology Working group on Electrophysiology and Arrhythmias.1–11 This is a voluntary registry covering all of Spain and is published annually. The majority of Spanish electrophysiology laboratories participate, making it one of the few large-scale observational catheter ablation registries.
The main objectives of the registry are to observe and describe developments in the interventional treatment of cardiac arrhythmias in Spain and provide reliable information on the type of activity carried out and the facilities available in arrhythmia units.
METHODSAs in previous years, 2 different systems were available for data collection: a prospective system and a retrospective system. The prospective approach uses a standardized database provided by the registry and requires patients to be added individually. The retrospective approach involves completing a standard questionnaire sent to all interventional electrophysiology laboratory in January 2013 and is also available on the Working Group on Electrophysiology and Arrhythmias website.12 Data acquired via either system remain anonymous—even to the registry coordinators—and the Spanish Society of Cardiology guarantees that the participating centers cannot be identified.
The information collected relates to equipment and personnel in arrhythmia units, procedures performed, and the demographic characteristics of the patients. As in previous years, data on human resources correspond only to public-sector centers and the epidemiological variables presented only correspond to patients from centers that submitted their data prospectively.
We analyzed the same 10 arrhythmic substrates as in previous records: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways (AP), atrioventricular node (AVN) ablation, focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant reentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia associated with postinfarction scar (VT-AMI), and ventricular tachycardia associated with nonischemic heart disease (VT-NAMI). We analyzed a series of variables common to all substrates: the number of patients and procedures performed, success rate, type of ablation catheter used, and the number and type of procedure-related complications, including periprocedural death. We also collected a series of specific variables for certain substrates, including the anatomical location of the AP, the location and mechanism of ATs, and the type of ventricular tachycardia (VT).
As in previous years, the success rate was based on end-of-procedure data (acute success rate). The number of recurrences could not be determined because follow-up was not analyzed. Because different therapeutic approaches with distinct objectives are used for the AF and VT-AMI substrates, success/failure criteria may vary as a function of technique. Hence, these substrates were excluded from the analysis of the overall success of the ablation procedures. Only those complications that occurred during the postprocedure hospital stay were reported.
Statistical AnalysisQuantitative variables are presented as mean (standard deviation). Differences between quantitative variables were assessed using the Student t test for dependent or independent samples, as appropriate. Differences between qualitative variables were analyzed using the chi-squared test and the Fisher exact test. A P value of <.05 was used as a cutoff for statistical significance. The statistical analysis was performed using an SPSS 15.0 database.
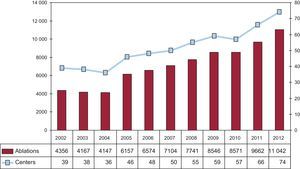
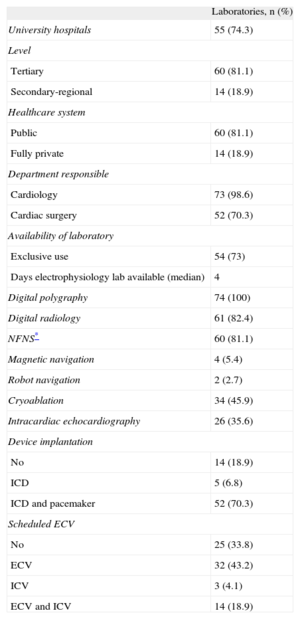
RESULTSFollowing the general trend in recent years, there was an increase in both the number of participating centers and the total number of ablations performed. Of the 74 participating centers (Appendix 2), 60 (81.1%) belonged to the public health care system and 14 were private; for the first time, there were over 10 000 ablation procedures (Fig. 1).
The retrospective data collection system was once again the preferred method. Only 8 centers (10.8%) collected data prospectively.
The majority of the participating centers were tertiary (81.1%) and university (74.3%) hospitals. Data from 73 of the 74 centers (98.6%) was provided by cardiology departments; 70.3% offer cardiac surgery (Table 1).
Characteristics and Infrastructure of the 74 Electrophysiology Laboratories Participating in the 2012 Registry
| Laboratories, n (%) | |
| University hospitals | 55 (74.3) |
| Level | |
| Tertiary | 60 (81.1) |
| Secondary-regional | 14 (18.9) |
| Healthcare system | |
| Public | 60 (81.1) |
| Fully private | 14 (18.9) |
| Department responsible | |
| Cardiology | 73 (98.6) |
| Cardiac surgery | 52 (70.3) |
| Availability of laboratory | |
| Exclusive use | 54 (73) |
| Days electrophysiology lab available (median) | 4 |
| Digital polygraphy | 74 (100) |
| Digital radiology | 61 (82.4) |
| NFNS* | 60 (81.1) |
| Magnetic navigation | 4 (5.4) |
| Robot navigation | 2 (2.7) |
| Cryoablation | 34 (45.9) |
| Intracardiac echocardiography | 26 (35.6) |
| Device implantation | |
| No | 14 (18.9) |
| ICD | 5 (6.8) |
| ICD and pacemaker | 52 (70.3) |
| Scheduled ECV | |
| No | 25 (33.8) |
| ECV | 32 (43.2) |
| ICV | 3 (4.1) |
| ECV and ICV | 14 (18.9) |
ECV, external cardioversion; ICD, implantable cardioverter-defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
As in previous registries, epidemiologic characteristics were only available for data collected prospectively. This year, 8 centers used this method (as in 2011), with a total of 1885 ablation procedures.
The mean age of the patients was 44 (15) years. The youngest were those undergoing AP ablation (38 [11] years) and the oldest were those undergoing AVN ablation (75 [8] years). AVNRT ablation was predominantly performed in women (79%), whereas AF (77%) and VT (72%) ablation (whether associated with structural heart disease or not) were predominantly performed in men. These data are virtually identical to those reported in previous registries.
Similarly, 40% of patients had a history of structural heart disease, whereas left ventricular dysfunction was generally limited to patients undergoing AVN and VT ablation associated with heart disease. The same distribution was observed in patients with automatic implantable cardioverter defibrillators.
Infrastructure and ResourcesTables 1 and 2 show the technical and human resources available in the laboratories participating in the registry, as well as their activities.
Change in Human Resources in Public Hospital Laboratories Participating in the Registry Since 2004
| 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 | 2005 | 2004 | |
| Staff physicians, no. | 2.7 | 2.6 | 2.8 | 2.6 | 2.5 | 2.4 | 2.3 | 2.2 | 2.2 |
| Full-time physicians, no. | 2.1 | 2.2 | 2.3 | 2.1 | 2.1 | 2.1 | 1.8 | 1.7 | 1.6 |
| Fellowship students/year, no. | 0.7 | 0.7 | 0.75 | 0.8 | 0.6 | 0.6 | 1.3 | 0.6 | 0.7 |
| RN, no. | 2.3 | 2.3 | 2.4 | 2.2 | 2.2 | 2 | 1.7 | 1.7 | 1.6 |
| TAR, no. | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 | 0.2 | 0.2 |
RN, registered nurse; TAR, technical assistant radiologist.
A total of 54 centers (73%) had at least 1 laboratory exclusively dedicated to electrophysiology and 10 centers (13.5%) had 2. As in previous years, the laboratory was available for a mean 3.7 (1.4) days/week (median, 4). Only 3 of the 15 private centers had a room exclusively dedicated to electrophysiology.
External electrical cardioversion was performed in 46 laboratories (62% of the total laboratories) and internal cardioversion in 23%. Compared with 2011, there was an increase in the number of centers with facilities for cardiac pacing device implantation: most laboratories (81%) were equipped for this procedure, mainly defibrillators. In 70.3% of laboratories, both defibrillators and pacemakers were implanted; defibrillators alone were implanted in 6.8% and pacemakers alone in 4.1%.
Digital polygraphy was available in all centers; 82.4% had digital radiology, and 55.4% had portable fluoroscopy. A nonfluoroscopic navigation system was available in 81.1% of the centers: 20 centers had 2, and 1 center had 3. Although there were few differences compared with previous registries, nonfluoroscopic navigation systems were more widespread among public-sector centers (89.8% vs 53.3% in private centers).
The number of remote navigation systems slightly increased compared with previous years. Four centers had a magnetic navigation system and 2 had a robotic navigation system. There was also a slight increase in the number of centers offering intracardiac echocardiography (26 centers). Echocardiographic ablation continued to be available in just 1 center, whereas a significantly greater number of centers offered cryoablation (34 centers; 45.9%).
The number of healthcare staff in electrophysiology laboratories remained largely unchanged. Some 73% of centers had more than 1 full-time physician, 40% had more than 2, and just 1 health center had 5 full-time staff physicians. Some 83% of laboratories had at least 2 full-time registered nurses. In total, 25 centers had fellowship students, with a mean of 1.76 per center (1 hospital had 8).
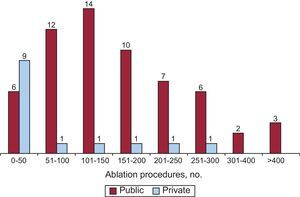
General ResultsIn total, 74 centers submitted data in 2012, constituting the highest level of participation since the registry began (Figs. 1 and 2). Some 11 042 ablations were reported, representing a mean of 149 (103) procedures/center (median, 128 [range, 6-457]). Just 5 private centers performed more than 50 ablations/year; 2 of these carried out more than 200/year. Five public centers performed more than 300 ablations; 3 of these performed more than 400.
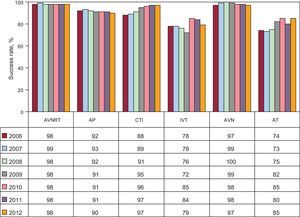
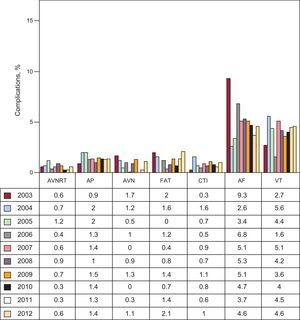
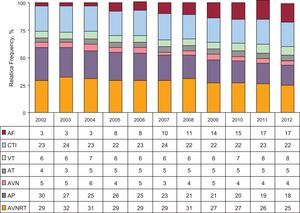
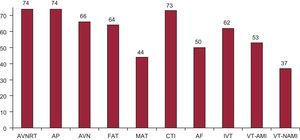
The overall success rate was 94.9% (8283/8725), excluding AF and VT-AMI substrate ablation. There was a total of 210 (1.9%) reported complications (vascular complications, atrioventricular block, stroke, effusion/tamponade, myocardial infarction, heart failure, and death) during the ablation procedures (including AF and VT-AMI). Five deaths were reported (0.04%): 2 patients with CTI ablation (one in a patient with advanced heart failure who developed acute pulmonary edema 48 h after the procedure, and another in a patient who had a massive stroke after withdrawal of anticoagulation prior to pacemaker implantation). Two deaths occurred in patients with VT-AMI ablation (due to electric storm or refractory shock in both cases) and another occurred in a patient with AF ablation secondary to perforation of the coronary sinus. Iatrogenic atrioventicular block occurred in 22 patients (0.19%) who required permanent pacemaker implantation: 10 occurred during AVNRT ablation, 4 during AP ablation, 1 during FAT ablation, 1 during CTI ablation, 1 during AT ablation, 1 during VT-NAMI ablation, and 4 during VT- AMI ablation. Figures 3 and 4 show the overall results in terms of success and complication rates compared with those of previous years. Percentage success rates for the different substrates remained stable, except for IVT ablation, for which they decreased from 84% to 79%, and for FAT ablation, for which they increased from 80% to 85%. The incidence of complications remained stable for all substrates except AVN (for which they increased from 0.3% to 1.1%), FAT (from 1.4% to 2.1%) and AF (from 3.7% to 4.6%). The most frequently treated substrate was AVNRT, followed by CTI and AP (Fig. 5). The number of ablation procedures increased for all substrates except VT-AMI, for which there was a 3% decrease compared with 2011. However, there was a very significant increase in AF, AP, FAT, AVN, and IVT ablation (there was a 30% increase in IVT ablation compared with 2011). The number of AF ablation procedures increased by 21% compared with 2011, accounting for 17% of all procedures (was the fourth substrate in order of frequency). The least treated substrate continued to be VT-NAMI, although the number of procedures increased considerably in the last 2 years.
Change in percentage success rates for catheter ablation since 2006 by substrate treated. AP, accessory pathways; AT: atrial tachycardia; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; IVT, idiopathic ventricular tachycardia.
Percentage of complications in catheter ablation since 2003 by substrate treated. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
Relative frequency of different conditions treated by catheter ablation in Spain during 2012. The percentage change for each substrate compared with the 2011 registry is shown. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with acute postinfarction myocardial scarring; VT-HD, ventricular tachycardia associated with heart disease.
Changes in the relative frequency of the substrates treated since 2002 are shown in Figure 6. In the last decade, AVNRT and AP ablation decreased, whereas AF ablation increased.
In 2012, AVNRT and AP were the only substrates treated in all centers, followed by CTI (98.6%) and AVN (89.2%) (Fig. 7). The substrate treated in the fewest centers continued to be VT-NAMI (50%). The number of centers performing AF ablation rose from 44 to 50, accounting for 67.6% of all centers and 71.6% public-sector centers.
Number of electrophysiology laboratories participating in the Spanish catheter ablation registry that treat each of the substrates. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute postinfarction myocardial scarring; VT-NAMI, ventricular tachycardia not associated with acute postinfarction myocardial scarring.
The following sections analyze the data for each arrhythmia.
Atrioventricular Nodal Reentrant TachycardiaThis was the most frequently treated substrate and ablation was performed in all centers. A total of 2842 ablation procedures were performed (25.7% of all procedures). The average number of procedures per center was 38 (24) (range, 1-105). The success rate was 98.2% (2792/2842) and 49 centers (66%) achieved 100% success rates. Complications occurred in 17 patients (0.6%): 10 patients (0.35%) had an atrioventricular block requiring permanent pacemakers, 6 patients developed vascular access complications, and 1 patient developed a pulmonary thromboembolism.
The most commonly used ablation catheter was the conventional 4-mm-tip radiofrequency catheter. An 8-mm-tip catheter was used in 20 patients, irrigated-tip catheter in 26, and cryoablation catheter in 65.
Cavotricuspid IsthmusThe second most frequent procedure was CTI ablation. A total of 2485 ablation procedures were performed (mean 34 [24]) and were successful in 2400 patients (96.6%). This substrate was treated in 73 of the 74 centers (98.6%) and 37 centers reported 100% success rates. Major complications occurred in 25 patients (1%): 17 patients developed vascular complications; 1 patient had an atrioventricular block requiring a permanent pacemaker, 2 patients had strokes, 1 patient developed pericardial effusion (without associated tamponade), 1 patient developed heart failure, 1 patient had a pulmonary thromboembolism, and 2 died. One of the 2 patients who died had decompensated heart failure; a few hours after ablation, the patient went into cardiogenic shock and died. The other death occurred in a patient who had a massive stroke after withdrawal of anticoagulation prior to pacemaker implantation.
The use of a 4-mm-tip ablation catheter was rare (5.6%) in this substrate. Irrigated-tip catheters were used in 1357 procedures, 8-mm-tip catheters in 965, and cryoablation catheters in 40.
Accessory PathwaysThis was the third most frequently treated substrate and was performed all centers. A total of 1999 AP ablation procedures were performed, with a mean of 27 (20) procedures per center (range, 1-97). There were 1816 successful procedures (90.8%) and only 4 of the 57 centers that performed more than 10 AP ablations reported 100% success rates. Major complications occurred in 28 patients (1.4%): 15 patients had vascular complications, 4 had an atrioventricular block requiring permanent pacemakers, 3 had strokes, 2 developed pericardial effusion, and 4 had myocardial infarctions.
Nonconventional ablation catheters were used in 328 patients (16.4%): irrigated-tip-catheters were used in 235 procedures, cryoablation catheters in 91, and 8-mm-tip catheters in 10.
The AP location was reported in all patients. As in previous registries, the most frequent locations continued to be the left ventricular free wall (51.2%) and inferior paraseptal pathways (25.3%). The locations least often treated continued to be the peri-Hisian or superior paraseptal pathways (8.3%). Procedural success depended on the AP location: 95% (972/1024) success was reported in the left free wall, 91.6% (286/312) in the right free wall, 86.4% (437/506) in the inferior paraseptal pathway, and 77% (127/165) in the peri-Hisian/superior paraseptal pathways.
This was the first year in which the register collected data on the type of conduction in the AP. In total, 58 centers submitted data: there was bidirectional conduction in 878 AP, exclusively anterograde conduction in 126, and exclusively retrograde conduction in 567.
Atrioventricular Node AblationIn total, 459 procedures were performed and success was achieved in 97.4% of the procedures. Complications occurred in 5 patients (1.1%): 3 patients presented vascular access complications; and 2, heart failure.
Nonconventional catheters were used in 98 cases: 8-mm-tip catheters were used in 38 procedures; and irrigated-tip catheters in 60.
Focal Atrial TachycardiaA total of 333 FAT ablation procedures were performed, with a success rate of 85.3% (284/333) and a mean of 6.2 (5.9) procedures per center. This substrate was treated in the right atrium in 61 centers, but in the left atrium in only 36. In total, 72 centers reported the origin of FAT and the procedural success rate was similar in both atria: 83% (195/235) for ablations in the right atrium vs 82.2% (74/90) for those in the left atrium. This was in contrast to previous years in which a higher success rate was reported for procedures in the right atrium.
Complications occurred in 7 patients(2.1%): 1 patient had an atrioventricular block requiring a permanent pacemaker, 2 developed vascular complications; and 4 had pericardial effusions.
As in 2011, the upward trend continued in the use of special catheters (156 in 2012 vs 119 in 2011): irrigated-tip catheters were used in 127 cases; cryoablation catheters in 23; and 8-mm-tip catheters in 6.
Macroreentrant Atrial Tachycardia/Atypical Atrial FlutterThis substrate was treated in 44 centers (59.5%), with a total of 227 procedures (mean, 5 [range, 1-15] procedures per center). The procedure was successful in 170 cases (74.8%). Complications occurred in 5 patients (2.2%): 1 patient developed femoral vascular complications, 2 had cardiac tamponade, 1 had acute pulmonary edema, and 1 had an atrioventricular block.
The origin of MAT was reported for all procedures: there were 109 cases of right origin; and 118, left origin; success rates were 81% and 68.3%, respectively. Catheters other than the conventional 4-mm tip were used in 87.6% of the procedures; an irrigated tip was used in most cases (90.4%) and an 8-mm tip in the remainder (9.6%).
Atrial FibrillationIn total, 1852 AF ablation procedures (range, 2-123) were performed in 50 (67.6%) of the participating centers. This represents a 21% increase compared with the previous registry, with a mean of 37 procedures per center. Ten laboratories performed less than 10 procedures and 19 laboratories less than 25. Eleven centers performed more than 50 procedures, and only 4 of these performed more than 100. Some 61.5% of the procedures (1139) were for paroxysmal AF and 37.5% (695) for persistent AF. Five centers reported 18 procedures for permanent AF. Of the procedures for persistent AF, 85 were for long-standing AF.
The treatment technique used was indicated in 1791 procedures (96.7%): ostial electrical disconnection was performed in 16.6% of patients, circumferential isolation with disconnection in 80.6%, and circumferential isolation with discharge reduction in the remaining 2.3%. In 37 procedures, the substrate was treated in the right atrium.
Almost all centers (76.8%) used irrigated-tip ablation catheters. There was a clear increase in the use of cryoenergy balloon ablation (350 procedures; 19%). An 8-mm-tip ablation catheter was used in only 4 procedures. Steerable sheaths were used in only 4 centers in 150 procedures (8% of all procedures).
Complications occurred in 87 patients (4.6%): significant pericardial effusion/cardiac tamponade in 42 patients, vascular access in 28, stroke in 7, phrenic nerve palsy in 7, and pulmonary vein stenosis in 2. One death (0.5%) occurred in the setting of tamponade secondary to perforation of the coronary sinus.
Idiopathic Ventricular TachycardiaA total of 349 IVT ablation procedures were reported in 62 centers (mean, 4.7 [range 1-28] ablations per center). Success was achieved in 276 procedures (79%), with 12 complications (3.4%): 7 cases of tamponade, 3 vascular complications, 1 atrioventricular block, and 1 myocardial infarction in the setting of a circumflex coronary artery dissection that required stenting.
The type of VT treated was reported in 303 procedures: 201 occurred in the right ventricular outflow tract and 62 in the left ventricular outflow tract; 40 were fascicular, and 46 were reported as “other location”. The success rates for these procedures were 79.1%, 83%, 85%, and 76%, respectively. The focal origin of the VT was the aortic root in 16 patients, pulmonary artery in 9, and in the interior of a coronary vein in 1. A 4-mm-tip ablation catheter was used 46.5% of patients, irrigated-tip catheter in 51.5%, and 8-mm-tip catheter in the remaining 2%.
Ventricular Tachycardia Associated With Postinfarction ScarringA total of 53 (71.6%) centers performed 323 VT-AMI ablation procedures (6 [range, 1-27] ablations per center). The complications reported (n=23; 7.1%) were vascular access (5); cardiac tamponade in 8 patients, stroke in 2, heart failure in 2, and complete atrioventricular block in 4. Two patients (0.6%) died due to electrical storm, shock, and electromechanical dissociation.
The type of ablation performed was reported in 98.4% of procedures: 75 used a “conventional” approach and 243 used a substrate approach. Irrigated-tip ablation catheters were used for these types of ablation in most procedures. Steerable sheaths were used in 61 procedures. The success rate was 82% with the conventional approach and 85.1% with the substrate approach. Compared with 2011, there was a significant increase in the number of epicardial procedures: 13.6% (44 procedures in 16 centers).
Ventricular Tachycardia not Associated With Postinfarction ScarringA total of 168 ablation procedures were performed for this substrate in 37 laboratories (50%).
The types of VT were arrhythmogenic cardiomyopathy in 38 patients, branch-branch in 11, nonischemic dilated cardiomyopathy in 61, nonsustained VT in 25, and “other” in 31. The success rates were 86.8%, 100%, 68.8%, 94.2%, and 67.7%, respectively. Four procedures were epicardial; 2 of these with acute success.
Complications occurred in 4 patients, all of which were related to vascular access.
Irrigated-tip ablation catheters were used in 97% of the procedures and 4-mm-tip catheters in the remainder.
DISCUSSIONData from the 2012 catheter ablation registry show a continued increase in the number of participating centers, and thus the registry is increasingly representative of the situation in Spain. In total, 74 centers participated, surpassing the 66 centers that participated in 2011, thus setting a new record. The mean number of ablations per center increased slightly, and the total number of procedures easily surpassed the number performed in 2011.
Healthcare staff levels remained the same this year. There was a slight increase in the number of physicians working in electrophysiology laboratories, although there was slight reduction in the number of full-time physicians. The number of fellowship students, registered nurses, and technical assistant radiologists remained stable compared with the data for 2011. Exclusive dedication of the electrophysiology laboratory occurred principally in public-sector centers.
The percentage of laboratories provided with a nonfluoroscopic navigation system remained steady at the 2009 level of around 80%. The number of centers with magnetic navigation increased to 4 and those with robot navigation to 2.
Despite the overall increase in the number of ablation procedures, the relative percentage of these procedures for each substrate remained stable compared with 2011. The number of AF ablation procedures significantly increased compared with the previous registry and for the first time steerable sheaths were included. There was a significant increase in the use of cryoenergy balloon procedures, which was probably related to the increase in the reported rate of phrenic nerve palsy. In contrast to 2011, there was an increase in the number of centers performing more than 50 AF procedures per year. The complications rate related to AF ablation increased slightly compared with 2011, due to a higher rate of vascular complications and phrenic nerve palsy.
The number of ventricular arrhythmias treated with ablation remained stable despite the decrease in VT-AMI ablation. This was due to the slight increase in ablation procedures for other VTs. In the case of VT-AMI, the substrate approach was 3 times more common than the conventional approach. The number of procedures using a steerable sheath were reported this year. In contrast to the previous registry, there was an increase in the number of ablation procedures for IVT. For the first time, the registry reported the number of procedures addressing extramyocardial structures (great vessels and coronary veins).
Thus, as in 2011, there appears to have been a steady increase in AF ablation procedures. However, VT ablation continued to be stable and there was a slight decrease in VT-AMI ablation. The use of irrigated-tip catheters continued to increase. These were the most frequently used catheters in the treatment of AF, MAT, VT-AMI, and VT-NAMI substrates. Attention is drawn to the significant increase in the use the cryoenergy balloon in AF ablation.
CONCLUSIONSAs in previous years, the Spanish Catheter Ablation Registry contains one of the largest samples of ablation procedures reported in international publications, surpassing the 9662 ablation procedures performed in 2011. Ever more complex substrates were treated, while maintaining a very high success rate with low rates of major complications and mortality.
Once again, the increase in the number and complexity of the ablations performed was not matched by an increased number of healthcare staff dedicated to this technique.
CONFLICTS OF INTERESTNone declared.
The coordinators of the registry would like to express their thanks to all participants in the 2012 Spanish Catheter Ablation Registry who voluntarily and disinterestedly submitted the data on the procedures they performed. They also wish to extend special thanks to Cristina Plaza for her excellent and untiring administrative work.
Julio Martí Almor, Miguel Ángel Arias, Josep Brugada, Mar González Vasserot, Andrés Bodegas, Oscar Alcalde, Ernesto Díaz Infante, Federico Segura Villalobos, Manuel Doblado Calatrava, José Luis Ibañez Criado, Alberto Barrera, María del Carmen Expósito Pineda, Vicente Bertomeu González, Rafael Romero Garrido, José Luis Moríñigo, Javier Pindado, Ángel Arenal, Jerónimo Rubio, José Manuel Rubio Campal, Juan Carlos Rodríguez Pérez, Adolfo Fontenla, Roberto Matía, Pablo Moriña, Nicasio Pérez Castellano, Alfonso Macías, Nuria Rivas Gándara, Ángel Moya i Mitjans, Naiara Calvo, Antonio Asso, Miguel Álvarez López, José Manuel Rubín, Aníbal Rodríguez, Ignacio Gil Ortega, Bieito Campos, Pablo Moriña, María Luisa Hidalgo, Gonzalo Rodrigo Trallero, Nelson Alvarenga, Jordi Pérez Rodón, Agustín Pastor, Joaquín Osca, Alonso Pedrote, Víctor Castro Urda, Rafael Peinado, Javier Fosch, Eduardo Caballero, Lluis Mont, Enrique Rodríguez Font, Xavier Viñolas, Sonia Ibars, Amador Rubio, Francisco Mazuelos Bellido, Dolores García Medina, Ángel Martínez Brotons, Antonio Peláez, Miguel Álvarez, Concepción Alonso, Arcadio García Alberola, Eloy Domínguez, Luisa Pérez Álvarez, Alicia Ibáñez, Felipe Rodríguez Entem, José Luis Martínez Sande, M. Fe Arcocha, Manuel Frutos, Georgia Sarquella Brugada, Ángel Grande, J. García Fernández, Benito Herreros, Jesús Almendral, and Xavier Sabaté.
| Andalusia | |
| Córdoba | Hospital Reina Sofía (F. Mazuelos) |
| Granada | Hospital Virgen de las Nieves (M. Álvarez) |
| Huelva | Hospital Blanca Paloma (P. Moriña), Hospital Juan Ramón Jiménez (P. Moriña) |
| Jaén | Complejo Hospitalario de Jaén (M. Frutos) |
| Málaga | Hospital Clínico Universitario Virgen de la Victoria (A. Barrera), Hospital Quirón (M. Álvarez) |
| Seville | Hospital Nisa Aljarafe (E. Díaz Infante), Hospital Virgen Macarena (E. Díaz Infante), Hospital Virgen del Rocío (A. Pedrote), Hospital Nuestra Señora de Valme (D. García) |
| Aragon | |
| Zaragoza | Hospital Lozano Blesa (G. Rodrigo), Hospital Miguel Servet (A. Asso), Clínica Quirón (A. Asso) |
| Asturias | Hospital Central de Asturias (J.M. Rubín), Hospital de Cabueñes (M. González) |
| Balearic Islands | Clínica Rotger (X. Viñolas), Hospital Son Llàtzer (X. Fosch), Hospital Quirón Palma (N. Alvarenga), Hospital Son Espases (MV. Expósito) |
| Canary Islands | |
| Las Palmas | Hospital Dr. Negrín (E. Caballero), Hospital Universitario Insular (F. Segura), Clínica Santa Catalina (J.C. Rodríguez) |
| Tenerife | Hospital Nuestra Señora de la Candelaria (R. Romero), Hospital Universitario de Canarias (A. Rodríguez) |
| Cantabria | Hospital Marqués de Valdecilla (F. Rodríguez) |
| Castile-La-Mancha | |
| Toledo | Hospital Nuestra Señora del Prado (A. Macías), Hospital Virgen de la Salud (MA. Arias) |
| Castile and León | |
| Burgos | Hospital Universitario de Burgos (J. García) |
| Leon | Hospital de León (M.L. Fidalgo) |
| Salamanca | Hospital Clínico Universitario (J.L. Moríñigo) |
| Valladolid | Hospital Río Hortega (B. Herreros); Hospital Clínico Universitario (J. Rubio) |
| Catalonia | |
| Barcelona | Hospital de Bellvitge (X. Sabaté), Hospital Clínic (L. Mont), Hospital Germans Trias i Pujol (O. Alcalde), Hospital del Mar (J. Martí), Hospital de la Santa Creu y Sant Pau (C. Alonso), Hospital Sant Joan de Déu (G. Sarquella), Hospital Vall d’Hebron (N. Rivas), Hospital Mútua de Terrassa (S. Ibars), Clínica Pilar Sant Jordi (J. Brugada), Clínica Sagrada Família (A. Moya), Clínica Teknon (E. Rodríguez), Instituto Universitario Dexeus (J. Pérez) |
| Lleida | Hospital Universitario Arnau de Vilanova (B. Campos) |
| Valencian Community | |
| Alicante | Hospital General (J.L. Ibáñez), Hospital de San Juan (V. Bertomeu), Cardioritmo Levante (A. Ibáñez) |
| Castellón | Hospital General de Castellón (E. Domínguez) |
| Valencia | Hospital Clínico Universitario de Valencia (A. Martínez), Hospital Universitario La Fe (J. Osca), Hospital Dr. Peset (A. Peláez) |
| Extremadura | |
| Badajoz | Hospital Infanta Cristina (M. Doblado) |
| Galicia | |
| A Coruña | Hospital Universitario de A Coruña (L. Pérez), Hospital Clínico Universitario de Santiago (J.L. Martínez Sande) |
| Community of Madrid | Fundación Jiménez Díaz (J.M. Rubio), Hospital 12 de Octubre (A. Fontenla), Hospital Gregorio Marañón (A. Arenal), Hospital La Paz (R. Peinado), Hospital Puerta de Hierro (V. Castro), Hospital Ramón y Cajal (R. Matía), Hospital Clínico San Carlos (N. Pérez Castellano), Hospital de Getafe (A. Pastor), Grupo Hospitales de Madrid (J. Almendral), Fundación Hospital Alcorcón (A. Rubio), Hospital de Leganés (A. Grande) |
| Region of Murcia | Hospital Virgen de la Arrixaca (A. García Alberola), Complejo Universitario de Cartagena (I. Gil) |
| Chartered Community of Navarre | Clínica Universitaria de Navarra (N. Calvo), Complejo Hospitalario de Navarra (no disponible) |
| Basque Country | |
| Vizcaya | Hospital Universitario de Cruces (A. Bodegas), Hospital de Basurto (M.F. Arcocha) |
| Álava | Hospital Txagorritxu (J. Pindado) |
The complete list of collaborators is included in Appendix 1.