This report describes the findings of the 2016 Spanish Catheter Ablation Registry.
MethodsData were retrospectively collected by means of a standardized questionnaire completed by each of the participating centers.
ResultsData were collected from 83 centers. A total of 13 482 ablation procedures were performed (the highest historically reported in this registry), with a mean of 162.4 ± 116 and a median of 136 procedures per center. The most frequently treated ablation targets were atrioventricular nodal re-entrant tachycardia (n = 3058; 22.7%), atrial fibrillation (n = 2953; 21.9%), and cavotricuspid isthmus (n = 2892; 21.4%). There was a peak in ablation procedures for atrial fibrillation, which, for the first time in this registry, became the second most treated substrate. After exclusion of atrial fibrillation and ventricular tachycardia with underlying heart disease, the overall success rate was 86%. The rate of major complications was 2.3%, and the mortality rate was 0.05%. In all, 2.7% of the ablations were performed in pediatric patients.
ConclusionsThe Spanish Catheter Ablation Registry systematically and uninterruptedly records the ablation procedures performed in Spain, showing a progressive rise in the number of ablations performed, with a high success rate and a low percentage of complications.
Keywords
The purpose of the present article is to report the findings of the Spanish Catheter Ablation Registry, the Official Report of the Working Group on Electrophysiology and Arrhythmias of the Spanish Society of Cardiology for 2016, which marks the 16th year of uninterrupted activity by this group.1–15 The registry is a voluntary nationwide record, published annually, that includes data from most of the arrhythmia units operating in Spain, making it one of the few large-scale, observational registries focusing on catheter ablation.
The main objectives of the registry are to observe and describe developments in the interventional treatment of cardiac arrhythmias in Spain and to provide reliable information on the type of activity carried out and the facilities available in Spanish arrhythmia units.
METHODSData were collected retrospectively using a standardized data collection form sent to all of the participating interventional electrophysiology laboratories in January 2017; the form was also available on the website of the Working Group on Electrophysiology and Arrhythmias.16 All of the compiled data remained anonymous, even to the registry coordinators, with the secretariat of the Spanish Society of Cardiology removing any identifying information from the data.
The information collected concerned the technical and human resources available in the arrhythmias units, the procedures performed, and their results and complications.
We analyzed the same 10 arrhythmias and arrhythmogenic substrates examined in previous registries: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways, atrioventricular node ablation, focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia associated with myocardial infarction (VT-AMI), and ventricular tachycardia not associated with myocardial infarction (VT-NAMI). The following variables common to these 10 conditions were analyzed: number of patients and procedures performed, success rate, type of ablation catheter used, and number and type of procedure-related complications, including periprocedural death. Also recorded for all ablation targets were the number of procedures performed with electroanatomic navigation, number of procedures performed without fluoroscopy, and number of procedures performed in pediatric patients (defined as those younger than 15 years). In addition, we analyzed a number of ablation target-specific variables, such as the anatomic location and type of accessory pathway conduction, location and mechanism of atrial tachycardias, type of AF ablation and approach, and ventricular tachycardia substrate.
As in previous years, the success rate refers only to the immediate postprocedural data (acute success rate). Several therapeutic approaches with different objectives can be used to treat AF, ventricular tachycardia associated with structural heart disease and the criteria for success/failure can differ according to the technique applied. Thus, AF, VT-AMI, and VT-NAMI were excluded from the analysis of the overall outcomes of ablation procedures. As for complications, only those occurring during the hospital stay after the procedure were reported.
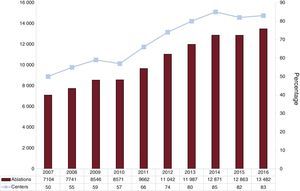
RESULTSEighty-three centers participated in the 2016 registry, the same number as in previous years (Appendix 1 and Appendix 2). However, the total number of procedures in 2016 was 13 482, the highest recorded in the history of the registry (Figure 1). The participating centers comprised 59 (71.1%) from the public health care system and 24 (28.9%) from the private sector.
The participating hospitals continued to be mainly tertiary (80.2%) and teaching (78.0%) centers. Patients were attended in cardiology departments in 81 of the 82 centers reporting this information (98.7%) and 71.1% had cardiac surgery units.
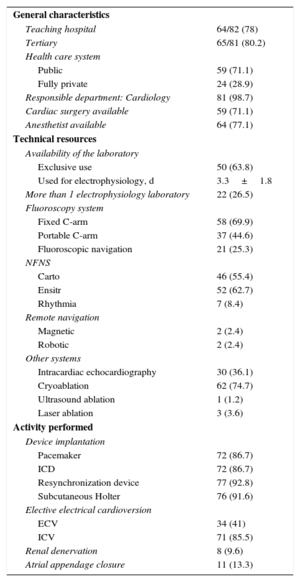
Infrastructure and ResourcesThe technical and human resources available in the laboratories participating in the registry and the activity carried out in them are presented in Table 1 and Table 2.
General Characteristics, Technical Resources, and Activity (in Addition to Catheter Ablation) of the 83 Electrophysiology Laboratories in the 2016 Registry
| General characteristics | |
| Teaching hospital | 64/82 (78) |
| Tertiary | 65/81 (80.2) |
| Health care system | |
| Public | 59 (71.1) |
| Fully private | 24 (28.9) |
| Responsible department: Cardiology | 81 (98.7) |
| Cardiac surgery available | 59 (71.1) |
| Anesthetist available | 64 (77.1) |
| Technical resources | |
| Availability of the laboratory | |
| Exclusive use | 50 (63.8) |
| Used for electrophysiology, d | 3.3±1.8 |
| More than 1 electrophysiology laboratory | 22 (26.5) |
| Fluoroscopy system | |
| Fixed C-arm | 58 (69.9) |
| Portable C-arm | 37 (44.6) |
| Fluoroscopic navigation | 21 (25.3) |
| NFNS | |
| Carto | 46 (55.4) |
| Ensitr | 52 (62.7) |
| Rhythmia | 7 (8.4) |
| Remote navigation | |
| Magnetic | 2 (2.4) |
| Robotic | 2 (2.4) |
| Other systems | |
| Intracardiac echocardiography | 30 (36.1) |
| Cryoablation | 62 (74.7) |
| Ultrasound ablation | 1 (1.2) |
| Laser ablation | 3 (3.6) |
| Activity performed | |
| Device implantation | |
| Pacemaker | 72 (86.7) |
| ICD | 72 (86.7) |
| Resynchronization device | 77 (92.8) |
| Subcutaneous Holter | 76 (91.6) |
| Elective electrical cardioversion | |
| ECV | 34 (41) |
| ICV | 71 (85.5) |
| Renal denervation | 8 (9.6) |
| Atrial appendage closure | 11 (13.3) |
ECV, external cardioversion; ICD, implantable cardioverter-defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
Data are expressed as no./No. (%) or mean±standard deviation.
Changes in the Human Resources in the Electrophysiology Laboratories of Public Hospitals Participating in the Registry Since 2007
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Staff physicians | 2.4 | 2.5 | 2.6 | 2.8 | 2.6 | 2.7 | 2.8 | 2.8 | 3.0 | 3.0 |
| Full-time physicians | 2.1 | 2.1 | 2.1 | 2.3 | 2.2 | 2.1 | 2.0 | 1.9 | 2.4 | 2.1 |
| Residents/y | 0.6 | 0.6 | 0.8 | 0.7 | 0.7 | 0.7 | 0.6 | 0.6 | 0.8 | 0.7 |
| RN | 2.0 | 2.2 | 2.2 | 2.4 | 2.3 | 2.3 | 2.2 | 2.3 | 2.7 | 2.7 |
| RT | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 | 0.3 |
RT, radiologic technologist; RN, registered nurse.
Fifty centers (63.8%) were equipped with at least 1 dedicated cardiac electrophysiology laboratory, 20 centers (24.1%) had 2 such laboratories, and 2 (2.4%) had 3. On average, the laboratory was available on 3.3±1.8 (median, 4) days a week.
Devices for the diagnosis and/or treatment of rhythm disturbances were implanted in 81 centers (97.6%): pacemakers in 72 centers (86.7%), defibrillators in 72 (86.7%), resynchronization devices in 77 (92.8%), and subcutaneous Holter monitors in 76 (91.6%).
At least 1 fixed C-arm fluoroscopy system was available in 58 centers (69.9%) and at least 1 portable fluoroscopy system was available in 37 (44.6%). Most centers (86.7%) had at least 1 nonfluoroscopic navigation system, 31.3% had 2 nonfluoroscopic navigation systems, and 8.4% had 3 such systems, figures slightly higher than in the previous registry. In addition, 25.3% of the centers had an X-ray system with integrated fluoroscopy (rotational angiography).
The use of remote navigation systems was limited to 4 centers (4.8%), 2 with magnetic navigation systems and 2 with robotic navigation systems. Thirty centers (36.1%) reported that they had intracardiac echocardiography. The most common nonradiofrequency ablation technique was cryoablation, whose use continues to increase (74.7% this year, 61% in 2015, and 56% in 2014). Other energy sources (laser, ultrasound) were rarely used.
Electrophysiology laboratories employed an average of 3 staff physicians (Table 2), although the full-time average was 2.1. The number of full-time physicians ranged from 0 to 5. A total of 73.5% of centers had at least 1 full-time physician and 62.6% had 2 or more. In addition, 79.5% of centers had at least 2 (range, 1-6) registered nurses. This year, 21 centers (25.3%) had between 1 and 6 resident physicians, usually 1 or 2.
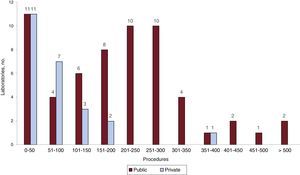
Overall ResultsThe number of centers participating in the registry this year (83 centers) was similar to that of the previous year (82); the changes in participation over time are shown in Figure 1. However, the number of ablations performed (13 482) is the highest reported to the registry and represents a 4.8% increase vs 2015. The mean number of procedures per center was 162.4±116 (157±119 in 2015) and the median was 136 (range, 3-530). More than 300 ablations were performed in 11 centers (10 of which were public), with 5 centers, all public, performing more than 400 ablations (Figure 2).
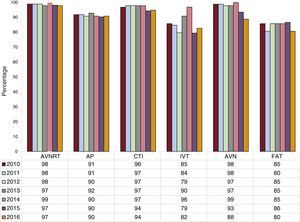
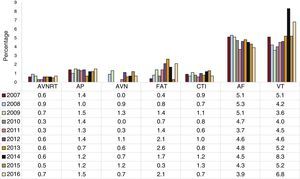
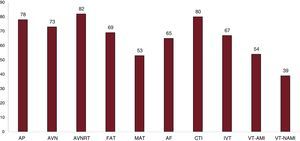
The overall success rate, excluding the treatment of AF, VT-AMI, and VT-NAMI, was 86%. Figure 3 shows the ablation procedure success rate since 2010, excluding, as in previous years, the treatment of AF, MAT, VT-AMI, and VT-NAMI. The success rates for the complex substrates were as follows: MAT, 72%; VT-AMI, 83%; and VT-NAMI, 64%. The number of complications reported for all ablation procedures was 307, which represents 2.3% and is similar to that reported in 2015 (2%). The distribution of the complications for the different ablation targets is shown in Figure 4. The most frequent complications were vascular (40.7%), followed by pericardial effusion/cardiac tamponade (29%). There were 13 cases of iatrogenic atrioventricular block (0.1% of all ablation procedures and 4.2% of all complications) requiring permanent pacemaker implantation: 4 during AVNRT ablation, 3 during accessory pathway ablation, 1 during FAT ablation, 1 during MAT ablation, and 4 during the ablation of the various types of VT. There were 7 periprocedural deaths (0.05%), 4 less than in the previous year; 6 deaths occurred during VT ablation in patients with structural heart disease (VT-AMI or VT-NAMI) and 1 occurred due to a vascular complication after CTI ablation.
Changes in catheter ablation success rates since 2010 by the arrhythmia or arrhythmogenic substrate treated. AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia.
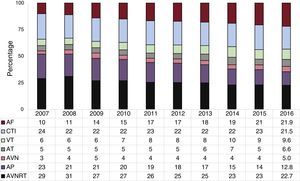
Changes in major complications related to catheter ablation since 2007 by the arrhythmia or arrhythmogenic substrate treated. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
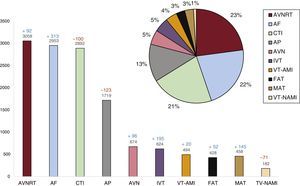
Regarding the frequency of the ablation targets treated and their changes over time, AVNRT was the most frequent ablation target (23%) and, for the first time in the 16 published registries, AF has become the second-most common ablation target; in 2016, CTI was the third most common target.
Compared with 2015, the number of ablations of all substrates increased, except CTI, accessory pathways, and VT-NAMI (Figure 5). The changes in the relative frequency of the different ablation targets since 2007 are shown in Figure 6. Notably, the trend continues for increased ablation of AF with respect to the other ablation targets and decreased ablation of accessory pathways; this trend has been observed since the registry was first published. VT ablation (of any cause, including ventricular extrasystole) was the highest reported thus far in previous registries (10% of substrates).
Relative frequency of arrhythmias and arrhythmogenic substrates treated by catheter ablation in Spain in 2016 (n=13 482). The change in the number of cases compared with the 2015 registry is shown for each ablation target. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with myocardial infarction; VT-NAMI, ventricular tachycardia associated with heart disease and not associated with myocardial infarction.
Changes in the relative frequency of different ablation targets treated since 2007. AF, atrial fibrillation; AP, accessory pathway; AT, atrial tachycardia (focal and atypical flutter); AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
Information on the number of laboratories treating each of the different arrhythmia targets is shown in Figure 7. Atrioventricular nodal reentrant tachycardia was the most frequently treated substrate in the participating centers (98.8%), followed by CTI (97.6%). The number of centers performing AF ablation continues to grow, increasing from 73.1% in 2015 to 78.3% in 2016.
Number of electrophysiology laboratories participating in the registry that treat each of the different ablation targets. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with myocardial infarction; VT-NAMI, ventricular tachycardia associated with heart disease and not associated with myocardial infarction.
The following sections summarize the data analysis for the different subgroups.
Atrioventricular Nodal Reentrant TachycardiaIn contrast to the 2015 registry, AVNRT was the most frequently treated substrate. A total of 3058 AVNRT ablation procedures were performed (22.7% of the total). The mean number of procedures per center was 36.8±26 (range, 2-119). The success rate was 97% and 64 centers (77%) reported a 100% success rate. There were 22 major complications (0.7%): 4 cases of atrioventricular block requiring a permanent pacemaker, 12 vascular access complications, 1 stroke, and 3 pericardial effusions (with or without tamponade). The most commonly used ablation catheter was the standard 4-mm tip radiofrequency catheter, used in 87% of procedures. Additionally, a cryoablation catheter was used in 75 cases (2.5%) and an irrigated-tip catheter in 1.7% (53 catheters, 2 of which were contact force-sensing catheters). A navigation system was used in 179 procedures (6%) and, of these, 150 (5% of the total) were entirely performed without fluoroscopy.
Cavotricuspid IsthmusFor the first time, CTI ablation, performed in 97.6% of centers, exceeded AF ablation.
A total of 2892 ablation procedures (21.4%) were performed, with a mean of 34.9±29.0 procedures per center (range, 1-156). Success was reported in 94% of the cases, with a 100% success rate in 46 centers (55%).
There were 21 major complications (0.7%), including 14 vascular complications (resulting in 1 death), 1 stroke, 1 myocardial infarction, 1 case of heart failure, and 1 pericardial effusion/tamponade. In addition, 1465 irrigated-tip catheters were used (50.6%) (168 with contact force-sensing technology) and 1166 8-mm catheters.
A navigation system was used in 539 procedures (18.6%), with 202 (7% of the total) entirely performed without fluoroscopy.
Accessory PathwaysAccessory pathways were again the fourth most targeted substrate, performed in 94% of centers. Nonetheless, as in recent years, the number of ablations decreased. There were 1712 procedures, yielding a mean of 22.0±16.7 per site (range, 18.2-25.8). Success was achieved in 1539 procedures (89.9%) and 22 centers reported a 100% success rate.
The data available on the direction of accessory pathway conduction confirm that most pathways exhibited bidirectional (41.1%) or exclusively retrograde (40.2%) conduction, whereas 18.7% showed exclusively anterograde conduction. Regarding their locations, left-sided accessory pathways continued to predominate (49.9%), followed by inferoseptal (26.2%). However, for the first time, para-Hisian pathways were more commonly treated than right ventricular free wall pathways (13.1% vs 10.8%).
Nonfluoroscopic 3-dimensional navigation systems were used in 284 procedures (16.6%); 44 of these were performed entirely without fluoroscopy. For the first time, data are available on the access approach used in the ablation of left-sided accessory pathways, predominantly retroaortic (75.8%); the remainder were transseptal (24.2%).
The highest accessory pathway success rates in the current registry were seen for inferoseptal pathways. According to the available data and the type of pathway treated at each of the locations, the success rate was 98.1% for inferoseptal pathways, 95.2% for left ventricular free wall, 93.7% for right ventricular free wall, and 88.4% for para-Hisian/anteroseptal.
There were 25 major complications (1.4%): 12 vascular complications (1 case of introducer entrapment in the femoral vein that required surgical removal), 7 pericardial effusions, 1 acute coronary event (secondary to coronary spasm in the right coronary artery, resolved with intravenous nitroglycerin), and 5 cases of atrioventricular block, 2 of which were transient and did not require permanent pacemaker placement. There was 1 death, described as sudden cardiac arrest 36hours after the procedure, with no further information.
The year 2016 saw another increase in the number of nonstandard ablation catheters from previous years: 414 irrigated-tip catheters (23 with contact force-sensing technology), 89 cryoablation catheters, and three 8-mm tip catheters. Fluoroscopy was not used in 2.6% of accessory pathway ablations.
Atrioventricular Node AblationIn all, 674 atrioventricular node ablation procedures were reported by 73 centers. Success was achieved in 88% of cases. There were 5 complications (0.7%), all vascular. Catheters other than the standard 4-mm tip catheter were used in 237 procedures (35.2%): 137 irrigated-tip catheters and 100 8-mm tip catheters.
Focal Atrial TachycardiaA total of 428 FAT ablation procedures (3.2%) were performed in 69 centers, with a success rate of 72%. The available data show that the FAT was in the right atrium in 297 cases (89.6% success rate) and in the left atrium in 131 (68.7% success rate). There was an increase vs the 2015 registry (1.6%), with 9 complications (2.1%) this year: 1 complete atrioventricular block requiring pacemaker implantation, 3 vascular complications (0.3%), 2 pericardial effusions, 2 myocardial infarctions, and 1 patient with symptoms of hemodynamic instability.
A total of 147 4-mm tip catheters were used and most catheters were conventional irrigated-tip catheters (used in 43.3% [181]), with a substantial number of contact force-sensing catheters (76); the remainder were rarely used: cryoablation in 9 procedures and 8-mm tip catheters in 5.
A navigation system was used in 247 procedures (57.7%) and, of these, 14 (3.3% of the total) were entirely performed without fluoroscopy.
Macroreentrant Atrial Tachycardia/Atypical Atrial FlutterThis ablation target was treated in 54 centers (65%), with 458 procedures (3.4%) in 404 patients (mean, 5.5±2.0 procedures per center; range, 0-47). There was a marked increase in the treatment of this ablation target—145 cases (31.6%)–vs the previous year. The procedure was successful in 328 cases (72%). In total, 187 MAT procedures were performed in the right atrium (successfully in 91%) and 254 in the left atrium (successfully in 81%). For the first time, information was available on the substrate underlying the MAT: 133 were secondary to AF ablation (36.0%), 69 to congenital heart disease (18.7%), 58 to arteriotomy (15.8%), and 61 to others (16.5%).
There were 14 nonfatal complications (3%): 7 femoral vascular complications, 6 pericardial effusions, and 1 atrioventricular block. Most catheters used were standard irrigated-tip catheters (48.3%) and irrigated-tip catheters with contact force-sensing technology (39.8%); the remainder were rarely used: 20 catheters with a 4-mm tip, 22 cryoablation, and 7 with an 8-mm tip. A navigation system was used in 280 procedures (61.1%) and, of these, 9 (2% of the total) were entirely performed without fluoroscopy.
Atrial FibrillationA total of 2953 AF ablation procedures were carried out in 2917 patients in 65 (78%) of the participating centers. These data repeat the tendency for a progressive increase in this substrate seen in previous registries and represent an increase of 313 ablations (10.5%) compared with the 2015 registry, which itself showed an increase of 5.7% compared with 2014. The mean number of procedures per center was 35.6±21.0 (range, 0-170), with an overall success rate of 91.5%.
Twenty-four centers (29%) carried out more than 50 procedures, with only 6 performing more than 100 procedures. Of the procedures reported, 1736 were for paroxysmal AF (58.8%), 770 for persistent AF (26%), and 107 for long-standing persistent AF (> 1 year) (3.6%).
The following procedural objectives were reported: general electrical isolation of the pulmonary veins in 2877 cases (97.4%), successful in 94%; reduction of the antral electrogram in 120 (4%), successful in 99.2%; placement of left atrial lines in 170 (5.7%), successful in 96.5%; complex fractionated electrogram ablation in 18 (0.7%), successful in 95.0%; superior vena cava isolation in 124 (4.2%), successful in 99.2%; and other objectives in 12 procedures (4 magnetic resonance-guided scar ablations and 8 atrial appendage isolations, 6 of which were performed with posterior box isolation).
The most frequently used catheter was an irrigated-tip ablation catheter with contact force-sensing in 1306 cases (43%) and in 43 centers (52% of the total); next most common was a cryoablation catheter, used in 917 cases (30%) in 30 centers (36%), and a conventional irrigated-tip catheter, used in 698 cases (23%) in 23 centers (28%).
Point-by-point radiofrequency ablation was still used for most procedures (66%), as in the previous year, while the use of cryoablation slightly increased (3%). Atrial fibrillation ablation with other single-shot techniques continued to be negligible: duty-cycled radiofrequency ablation (2.3%) was performed in only 2 centers and laser ablation (1.2%) in only 1. There was a marked increase in the use of steerable sheaths, with a total of 687 cases (23.3% of all procedures vs 11.6% in the previous registry). These sheaths were used in 27 centers (32%).
Intracardiac echocardiography is still used in few AF ablation procedures, just 112 (3.8%) in 2016. Three-dimensional navigation was used for this ablation target in 2019 procedures (68.4%); of these, no center reported that fluoroscopy was completely omitted, although some centers did perform the technique with “minimal fluoroscopy”.
There were 116 complications (3.9%, slightly less than in the previous registry [4.3%]), as follows: pericardial effusion/cardiac tamponade (36 [1.2%]), vascular access complications (40 [1.35%]), stroke (3 [0.1%]), phrenic nerve palsy (10 [0.3%]), infarction/angina (5 [0.16%]), heart failure (1 [0.3%]), and transient atrioventricular block not requiring pacemaker (1 [0.03%]). Additionally, there was 1 air embolism (with ST-segment elevation), 1 catheter entrapment in the mitral valve apparatus (which required surgery), 1 transient sinus node dysfunction with cryoablation, 1 interatrial septum dissection, 1 hemoptysis resolved with protamine, 1 transient gastroparesis, 2 severe postablation bronchospasms, and 1 esophageal ulcer with subsequent development of gastroduodenal reflux.
Idiopathic Ventricular TachycardiaIdiopathic ventricular tachycardia ablation was performed in 607 procedures in 67 centers (80.7%) (mean, 9.3±7.7 procedures per center). In all, 492 procedures were successful (81.1%), a slightly higher rate than that reported in the previous registry (78.8%). The type of ventricular tachycardia targeted was known in 521 procedures (85.8%): 333 of the right ventricular outflow tract, 86 of the left ventricular outflow tract, 49 originating from the aortic root/aortic cusps, 45 fascicular tachycardias, and 19 for ventricular tachycardias originating from the coronary/pericardial sinus. The most successfully ablated tachycardias were those originating from the left ventricular outflow tract, the right ventricular outflow tract, and fascicular ventricular tachycardia (90.7%, 89.4%, and 84.4%, respectively); the least successfully ablated tachycardias were those originating from the aortic root/coronary cusps and coronary/pericardial sinus (77.6% and 63.2%, respectively).
There were 27 complications (4.4%): 7 vascular complications (1.2%), 15 pericardial effusions/cardiac tamponades (2.5%), 1 stroke (0.2%), 2 acute coronary syndromes (0.3%), and 1 acute heart failure (0.2%).
A catheter other than the conventional 4-mm tip model was used in 85.7% of the cases. An irrigated-tip catheter without contact force-sensing was used in 321 cases (52.9%), an irrigated-tip with contact force-sensing in 190 (31.3%), an 8-mm tip catheter in 8 (1.3%), and cryoablation in 1 (0.2%). Fluoroscopy was not required for 9.1% of procedures.
Ventricular Tachycardia Associated With Myocardial InfarctionThe total number of VT-AMI ablation procedures has slightly increased, reaching 486 in the current registry (mean, 9.1±7.2 ablations per center).
The type of ablation performed was reported for 95.7%: 114 with a “standard” approach and 351 with a substrate approach, a similar ratio to the previous year. The overall success rate was 83.1% (higher than the results for 2015 and 2014, 80% and 81.2%, respectively).
There was a marked increase in the number of cases with an exclusively endocardial approach, 425 (87.5%) vs 335 (79.2%) in the previous year. Consequently, the number of procedures with an epicardial approach or combined approach (endocardial and epicardial) has decreased, with 24 procedures with an epicardial approach (4.9%) and 37 procedures with a combined approach (7.6%). This decrease in epicardial procedures is notable because this approach tended to be more popular in the last 3 years (3.7% in 2013, 5.4% in 2014, 8.7% in 2015, and 4.9% in the 2016 registry), and the same trend has been seen with the combined approach (12.1% in 2015 vs 7.6% in 2016).
For the endocardial approach, data were provided on the access route for 93.4% of cases. The retroaortic approach was used in 286 procedures (63%) and the transseptal approach in 168 (37%).
The following complications (47 [9.6%]) were reported: 22 vascular complications (4.5%), 13 pericardial effusions (2.7%), 7 heart failure events (1.4%), 2 embolic events (0.4%), 2 atrioventricular blocks (0.4%), and 1 phrenic nerve palsy (0.2%). There were 4 deaths (0.8%). The cause was specified in 3 cases. In 1 case, the procedure was begun with the patient in cardiogenic shock due to multiple implantable cardioverter-defibrillator discharges and the situation could not be reversed. In the second case, there was electromechanical dissociation secondary to intraprocedural cardiac rupture. Finally, the third case was reported as death 24hours after the procedure due to refractory cardiogenic shock after a new arrhythmic storm.
An irrigated-tip ablation catheter was used in most VT-AMI ablations (96.5%), of which 50.3% were contact force-sensing catheters. Steerable sheaths were used in 145 cases (29.8%).
Ventricular Tachycardia not Associated With Myocardial InfarctionA total of 182 VT-NAMI ablation procedures were performed in 39 laboratories (47%) (4.7±3.5 procedures per center). The type of ventricular tachycardia was specified in 165 cases: 91 cases of nonischemic dilated cardiomyopathy (70.3% success rate), 30 cases of arrhythmogenic cardiomyopathy (86.7% success rate), 22 cases of congenital heart disease (72.7% success rate), 10 cases of bundle branch reentrant ventricular tachycardia (100% success rate), and 11 reported as being of “another type” (54.5% success rate), which included 3 cases of Chagas disease, 2 of valvular heart disease, and 1 case of hypertensive heart disease.
Regarding the approach used for these ablation targets, there was greater use of the epicardial or combined (endocardial and epicardial) approach compared with VT-AMI procedures. Nineteen procedures were exclusively performed with an epicardial approach (10.4%) and 37 with a combined endocardial and epicardial approach (20.3%).
There were 17 complications (9.3%): 7 effusions/tamponades (3.9%), 4 vascular complications (2.2%), 1 heart failure event (0.5%), 1 atrioventricular block (0.5%), and 4 classified as “others” (2.2%; 2 cardiac perforations requiring cardiac surgery). There were 2 deaths, 1 occurring in a patient with dilated cardiomyopathy who had intraprocedural arrhythmic storm due to electromechanical dissociation.
The type of catheter used was reported in 158 procedures (86.8%). A catheter other than the 4-mm tip model was used in most cases (93.7%). The most commonly used catheter type was the irrigated-tip (144 cases [91.1%]), with contact force-sensing technology used in 81 (51.3%). An 8-mm tip catheter was used in only 4 cases.
Zero-fluoroscopy AblationNonfluoroscopic navigation was used in 4615 procedures (34%). Because of the tendency to perform zero-fluoroscopy procedures to protect patients and professionals from the risks associated with ionizing radiation, the registry has recorded for the first time data on procedures performed without fluoroscopy, which comprised 476 (3.5% of the total). The ablation target most frequently treated without fluoroscopy was the CTI (202 procedures, 7% of the total number of CTI ablations), although proportionally more IVT procedures were performed without fluoroscopy (57 procedures, 9.1% of the total number of IVT ablations).
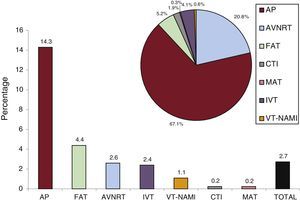
Ablations in Pediatric PatientsAblation procedures in pediatric patients have been identified in the registry for the first time, defined as those performed in individuals younger than 15 years (Figure 8). The registry recorded 369 ablation procedures (2.7% of the total number) in 35 centers (42.2%); the most frequent ablation target was the accessory pathways, with 246 procedures (67.1%), representing 14.3% of the total number of ablations performed of this target. The other procedures performed in pediatric patients by ablation target were as follows: 79 in AVNRT (20.8%), 19 in FAT (5.2%), 15 in IVT (4.1%), 7 in CTI (1.9%), 2 in VT-NAMI (0.6%), and 1 in MAT (0.3%).
Pediatric ablation procedures. The bar chart shows the proportion of pediatric procedures for each ablation target and the number of procedures in the registry while the pie chart shows the proportion of each substrate ablated with respect to the total number of pediatric procedures. AP, accessory pathway; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-NAMI, ventricular tachycardia associated with heart disease and not associated with myocardial infarction.
Catheter ablation treatment of cardiac arrhythmias has undergone an exponential growth in recent years. This rapid increase has necessitated a structural overhaul of the data collection approaches of our registry to enable it to continue to be a tool that accurately reflects the Spanish activity and contains information of practical interest for professionals involved in arrhythmia treatment. The most notable novelties this year include the incorporation of a single form and standardized data collection, updated information on the services portfolio and technical resources (eg, navigation systems, catheters) available in the laboratories, additional data collection related to the most complex ablation targets (AF, MAT, and ventricular tachycardias), information on the need for intraprocedural fluoroscopy, and identification of ablations performed in pediatric patients.
This year's registry amalgamates the experience of 83 centers reporting 13 482 procedures, which represents a record high both for the number of procedures and the mean number of ablations per center (162), as well as the number and percentage of AF ablations. The increased number of ablations this year can be explained by the opening of new electrophysiology laboratories in various centers, given that the number of centers with 2 or more rooms has increased from 10 in 2015 to 23 in 2016. However, there has been no growth in available human resources.
Regarding the proportional changes in the treatment of the various ablation targets, the tendency seen from the start of the registry has continued, namely, a progressive and continual increase in AF ablation and a corresponding decrease in accessory pathway ablation, which, for the first time, is the second-most frequently targeted substrate. Ablation of ventricular arrhythmias (including ventricular extrasystoles) is still in a plateau phase and represents 10% of the ablation procedures performed in Spain.
Despite the increased number of AF ablations, the mean number of procedures per center continues to be low, which is why this ablation target is still associated with the highest percentage of complications, although none were fatal. While the point-by-point radiofrequency technique is the most common method, there was another increase in cryoablation procedures. Notably, more than half of irrigated-tip catheters used had contact force-sensing information, which reflects the rapid uptake of this new technology in Spain.
There was a marked increase (of 45.5%) in the number of IVT ablations and a much less dramatic increase (of 4.2%) in VT-AMI. This latter ablation target is notable because the trend has changed, showing for the first time a fall in the number of epicardial ablations and an increase in endocardial approaches. As expected, almost all of the fatal complications were associated with VT ablation in patients with heart disease, most directly related to the poor preprocedural clinical situation of the patients.
For the first time, information is available on zero-fluoroscopy ablation, an approach that is currently rare (used in 3.9% of procedures), although it will be interesting to follow its changes in the coming years. Notably, zero-fluoroscopy ablation is being performed for some complex substrates (IVT, MAT) but not all. Various groups have reported the use of “minimal fluoroscopy” in AF ablation, although definition of and agreement on what constitutes “minimal fluoroscopy” are required for a systematic recording of these procedures.
Finally, effort has been made to identify pediatric procedures, whose absolute number and proportion for each ablation target were previously unknown. The results show a fragmentation in the number of centers performing pediatric ablations (more than 40%), which represent only 2.7% of the total number of ablations. The special characteristics of this population suggest that these procedures should be performed in fewer centers.
CONCLUSIONSThe Spanish Catheter Ablation Registry continues to systematically record the ablation procedures performed in Spain and its long track record and consistency make it the only such registry of its kind. The overall number of procedures and AF ablation procedures in particular reached a historical peak this year and still show very high success rates and low rates of complications. The high participation means that the registry continues to represent the current situation of this procedure in Spain.
CONFLICTS OF INTERESTNone declared.
Once again, the coordinators of the registry would like to thank all of the participants who voluntarily and selflessly submitted their data to the 2016 Spanish Catheter Ablation Registry. We extend special thanks to Cristina Plaza for her excellent and indispensable administrative work.
Miguel Álvarez-López, Jesús Almendral, Concepción Alonso, Luis Álvarez-Acosta, Ignasi Anguera, Eduardo Arana-Rueda, Ricardo Salgado-Aranda, María Fe Arcocha, Ángel Arenal, Miguel Ángel Arias, Antonio Asso, Alberto Barrera-Cordero, Gabriel Ballesteros, Andrés Bodegas-Cañas, Lucas Cano-Calabria, Eduardo Caballero-Dorta, Pilar Cabanas-Grandío, Bieito Campos, Víctor Castro, Ernesto Díaz-Infante, Javier Jiménez-Díaz, Manuel Doblado, María del Carmen Expósito-Pineda, Juan Manuel Fernández-Gómez, María Luisa Fidalgo, Dolores García-Medina, Arcadio García-Alberola, Ignacio Gil-Ortega, Carlos Gómez-Navarro, Mar González-Vasserot, Ángel Grande, José M. Guerra-Ramos, Julio Hernández-Afonso, Santiago Heras-Herreros, Sonia Ibars, Javier Jiménez-Candil, Francisco Mazuelos, Santiago Magnani, Javier Martínez-Basterra, Ángel Martínez-Brotons, José Luis Martínez-Sande, Roberto Matía-Francés, Pablo Moriña, Àngel Moya, Lluis Mont, José Moreno-Arribas, Javier Moreno-Planas, Marta Ortega-Molina, Joaquín Osca, Agustín Pastor, Rafael Peinado, Luisa Pérez-Álvarez, Nicasio Pérez-Castellano, Rosa Porro-Fernández, Jordi Punti-Sala, Aurelio Quesada, Nuria Rivas-Gándara, Gonzalo Rodrigo-Trallero, Felipe Rodríguez-Entem, Aníbal Rodríguez-González, Juan Carlos Rodríguez-Pérez, Enrique Rodríguez-Font, José Manuel Rubín, José Manuel Rubio, Amador Rubio-Caballero, Jerónimo Rubio-Sanz, Juan Miguel Sánchez-Gómez, Axel Sarrias, Georgia Sarquella-Brugada, and Emilce Trucco.
| Andalusia | |
| Almería | Hospital Mediterráneo (Carlos Gómez-Navarro) |
| Cádiz | Hospital Universitario Puerta del Mar (Lucas Cano-Calabria) |
| Granada | Complejo Hospitalario Universitario de Granada, Hospital Inmaculada (Miguel Álvarez-López) |
| Huelva | Hospital Juan Ramón Jiménez, Hospital Costa de la Luz (Pablo Moriña) |
| Córdoba | Hospital Reina Sofía (Francisco Mazuelos) |
| Málaga | Hospital Clínico Universitario Virgen de la Victoria, Hospital El Ángel, Vithas Parque San Antonio, Vithas Xanit Internacional, Hospital Quirón Salud Marbella (Alberto Barrera-Cordero); Hospital Quirón Salud Málaga (Miguel Álvarez-López) |
| Sevilla | Hospital Virgen Macarena, Hospital Nisa Aljarafe (Ernesto Díaz-Infante); Hospital Universitario Virgen del Rocío (Eduardo Arana-Rueda); Hospital Universitario Virgen de Valme (Dolores García-Medina); Hospital Quirón Infanta Luisa (Juan Manuel Fernández-Gómez) |
| Aragon | |
| Zaragoza | Hospital Universitario Miguel Servet, Hospital Quirón Salud Zaragoza (Antonio Asso); Hospital Clínico Universitario Lozano Blesa (Gonzalo Rodrigo-Trallero) |
| Principality of Asturias | Hospital de Cabueñes (Mar González-Vasserot); Hospital Central de Asturias (José Manuel Rubín) |
| Balearic Islands | Hospital Son Llàtzer (Santiago Magnani); Hospital Universitario Son Espases (María del Carmen Expósito-Pineda) |
| Canary Islands | |
| Las Palmas | Hospital Santa Catalina (Juan Carlos Rodríguez-Pérez); Hospital Universitario Dr. Negrín (Eduardo Caballero-Dorta) |
| Santa Cruz de Tenerife | Hospital Universitario Nuestra Señora de la Candelaria (Luis Álvarez Acosta); Hospital San Juan de Dios (Julio Hernández-Afonso); Hospital Universitario de Canarias (Aníbal Rodríguez-González) |
| Cantabria | Hospital Marqués de Valdecilla (Felipe Rodríguez-Entem) |
| Castile-La-Mancha | |
| Toledo | Hospital Virgen de la Salud (Miguel Ángel Arias) |
| Ciudad Real | Hospital General Universitario de Ciudad Real (Javier Jiménez-Díaz) |
| Castile and León | |
| Burgos | Hospital Universitario de Burgos (Ricardo Salgado-Aranda) |
| León | Hospital Universitario de León (María Luisa Fidalgo) |
| Salamanca | Hospital Universitario de Salamanca (Javier Jiménez-Candil) |
| Valladolid | Hospital Clínico Universitario Valladolid (Jerónimo Rubio-Sanz) |
| Catalonia | |
| Barcelona | Hospital Universitario de Bellvitge (Ignasi Anguera); Hospital Clínic (Lluis Mont); Clínica Teknon (Enrique Rodríguez-Font); Hospital Germans Trias i Pujol (Axel Sarrias); Hospital Vall d’Hebron (Nuria Rivas-Gándara); Clínica Corachán Barcelona (José M. Guerra-Ramos); Clínica Sagrada Família, Hospital Quirón Dexeus (Àngel Moya); Hospital Mútua de Terrassa (Sonia Ibars); Hospital Sant Joan de Déu (Georgia Sarquella-Brugada); Hospital Universitario de Sabadell (Jordi Punti-Sala); Hospital de la Santa Cruz y San Pablo (Concepción Alonso) |
| Lleida | Hospital Arnau de Vilanova (Bieito Campos) |
| Valencian Community | |
| Alicante | Hospital Universitario San Juan Alicante (José Moreno-Arribas); Hospital General Universitario de Alicante (José Luis Ibáñez-Criado) |
| Castellón | Hospital General Universitario de Castellón (Juan Miguel Sánchez-Gómez) |
| Valencia | Hospital La Fe (Joaquín Osca); Hospital General Universitario de Valencia (Aurelio Quesada); Hospital Clínico de Valencia (Ángel Martínez-Brotons); Hospital de Manises (Emilce Trucco); Hospital Universitario de la Ribera (Santiago Heras-Herreros) |
| Extremadura | |
| Badajoz | Hospital Infanta Cristina (Manuel Doblado) |
| Cáceres | Hospital San Pedro de Alcántara (Rosa Porro-Fernández) |
| Galicia | |
| A Coruña | Complejo Hospitalario Universitario de A Coruña (Luisa Pérez-Álvarez); Hospital Clínico Universitario Santiago de Compostela (José Luis Martínez-Sande) |
| Pontevedra | Hospital Álvaro Cunqueiro (Pilar Cabanas-Grandío) |
| Community of Madrid | Hospital Universitario Ramón y Cajal (Javier Moreno-Planas); Hospital Universitario 12 de Octubre (Adolfo Fontenla); Hospital Sanitas La Moraleja (Roberto Matía-Francés); Hospital Universitario de Getafe (Agustín Pastor); HM Hospitales (Jesús Almendral); Hospital Puerta de Hierro (Víctor Castro); Hospital La Paz (Rafael Peinado); Hospital Infantil La Paz (Marta Ortega-Molina); Hospital Clínico San Carlos (Nicasio Pérez-Castellano); Fundación Hospital Alcorcón (Amador Rubio-Caballero); Hospital Gregorio Marañón (Ángel Arenal); Fundación Jiménez Díaz (José Manuel Rubio); Hospital Severo Ochoa (Ángel Grande) |
| Region of Murcia | Hospital Virgen de la Arrixaca (Arcadio García-Alberola); Hospital Santa Lucía (Ignacio Gil-Ortega) |
| Chartered Community of Navarre | Complejo Hospitalario de Navarra (Javier Martínez-Basterra); Clínica Universidad Navarra (Gabriel Ballesteros) |
| Basque Country | |
| Vizcaya | Hospital de Cruces (Andrés Bodegas-Cañas); Hospital de Basurto (María Fe Arcocha) |
| La Rioja | Hospital Viamed Los Manzanos (F. Javier García-Fernández) |
The physician in charge of the registry in each center is indicated in parentheses.