The findings of the 2010 Spanish Catheter Ablation Registry are presented.
MethodsData were collected in two ways: retrospectively using a standardized questionnaire, and prospectively from a central database. Each participating center selected its own preferred method of data collection.
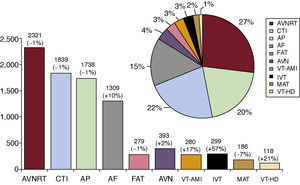
ResultsFifty-seven Spanish centers voluntarily contributed data to the survey. A total of 8762 ablation procedures was analyzed, averaging 154 (97) per center. The 3 main conditions treated were atrioventricular nodal reentrant tachycardia (n=2321; 27%), typical atrial flutter (n=1839; 22%), and accessory pathways (n=1738; 20%). Atrial fibrillation was the fourth most common condition treated (n=1309; 15%), and reflects mild growth. The overall success rate was 94%, major complications occurred in 1.7%, and the overall mortality rate was 0.06%.
ConclusionsData from the 2010 registry show that the number of ablations carried out continued to increase and exceeded 8700 ablations for the second time. In addition, they show, in general, a higher success rate and a lower number of complications. Again, cavotricuspid isthmus ablation for typical atrial flutter was the second most common condition treated. The number of catheter ablations carried out for ventricular arrhythmias in Spain is growing compared to the previous year.
Keywords
.
INTRODUCTIONThis is the Spanish Catheter Ablation Registry for 2010, published by Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias, which is completing its tenth year of uninterrupted activity.1, 2, 3, 4, 5, 6, 7, 8, 9 This is a voluntary Spanish registry, published annually, in which the majority of Spanish electrophysiology laboratories participate, making it one of the few large-scale observational catheter ablation registries.
The registry's objectives are to observe and report on the evolution of interventional treatment regarding cardiac arrhythmias in Spain, and to provide reliable information on the type of activity and facilities of our arrhythmia units.
METHODSAs in previous years, 2 different systems have been used for data collection: a prospective system and a retrospective system. The retrospective method was the most common, and involved the completion of a questionnaire that was sent to all interventional electrophysiology laboratories in January 2011. This questionnaire is available on the Electrophysiology and Arrhythmias Working Group website (www.arritmias.org). A standardized database, provided by the registry, was available for the prospective method and required that patients be added individually. The Spanish Society of Cardiology ensured that data collected by both systems was completely anonymous, even to the registry coordinators, so that the participating centers cannot be identified.
Information collected relates to the technical equipment and the personnel of the arrhythmia units, the procedures performed, and the demographic characteristics of patients. As on previous occasions, data on human resources only correspond to public centers, and epidemiological variables are only presented for patients belonging to those centers that chose the prospective data collection method.
We analyzed the same 10 arrhythmia substrates collected in previous registries: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways (AP), atrioventricular node (AVN) ablation, focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia associated with postinfarction scarring (VT-AMI) and ventricular tachycardia associated with nonischemic heart disease (VT-NAMI). We analyzed a series of variables common to all substrates, including the number of patients and procedures performed, the success rate, the type of ablation catheter used, and the number and type of complications suffered in connection with the procedure, including periprocedural death. We also collected a series of specific variables for particular substrates, such as the anatomical location of AP, the location and mechanism of atrial tachycardias, and the type of ventricular tachycardia.
As in previous years, the success rate only refers to the rate obtained at the end of the procedure (acute success rate). It was not possible to determine the number of recurrences because the subsequent follow-up was not analyzed. There are various therapeutic approaches with differing objectives for AF and VT-AMI substrates, and therefore the criteria for success or failure may differ depending on the technique used. For this reason, AF and VT-AMI substrates were excluded when analyzing overall success of the ablation procedure. Only those complications that occurred during the postprocedure hospital stay were reported, including those related to ablation of all substrates.
Statistical AnalysisQuantitative variables are expressed as means (standard deviation). Differences between quantitative variables were assessed using the Student t-test for dependent and independent samples, as appropriate. The chi-square test and the Fisher exact test were used to analyze the differences between categorical variables. Statistical significance was established at P<.05. Statistical analysis was performed using an SPSS 15.0 database.
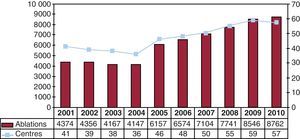
RESULTSIn contrast to previous registries, the number of participating centers did not exceed that of the previous year (Figure 1). Of the 57 participating centers this year (Appendix 1), 47 centers (82.5%) belonged to the public health system and 10 (17.5%) were private.
Figure 1. Change in the number of centers participating and procedures recorded in the Spanish Catheter Ablation Registry.
The retrospective data collection system was once again the preferred method. Only 7 centers (12%) collected data prospectively.
The characteristics of this year's participating hospital centers were similar to those of previous years. It should be noted that most are tertiary (89.5%) and university (82.5%) centers. The cardiology department reported the data in 98% of the cases, and 74% of the centers offered cardiac surgery (Table 1).
Table 1. Characteristics and Infrastructure of the 57 Electrophysiology Laboratories Participating in the 2010 Registry.
| no. (%) | |
| University hospitals | 47 (82.5) |
| Tertiary level | 51 (89.5) |
| Secondary level | 6 (10.5) |
| Health care system | |
| Public | 47 (82.5) |
| Fully private | 10 (17.5) |
| Department responsible | |
| Cardiology | 56 (98) |
| Intensive Care | 1 (2) |
| Cardiac surgery | 42 (74) |
| Availability of laboratory | |
| Exclusive dedication | 44 (77) |
| Days electrophysiology lab available (median) | 4 |
| Digital polygraphy | 57 (100) |
| Digital radiology | 41 (72) |
| NFNS (at least one) | 48 (84) |
| Magnetic navigation | 3 (5) |
| Robot navigation | 1 (2) |
| Cryoablation | 21 (37) |
| Intracardiac echocardiography | 21 (37) |
| Device implantation | |
| No | 15 (26) |
| ICD | 3 (5) |
| ICD and pacemaker | 39 (68) |
| Scheduled ECV | |
| No | 17 (30) |
| ECV | 31 (54) |
| ICV | 2 (4) |
| ECV and ICV | 7 (12) |
ECV, external cardioversion; ICD, implantable cardioverter defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
As in previous registries, epidemiological characteristics were only available for data collected prospectively. This year 7 centers used this method (1 fewer than in 2009), with a total of 1317 procedures.
Patient mean age was 41 (16) years. The youngest patients were those undergoing AP (34 [14] years), and the oldest were those who underwent AVN ablation (74 [8] years). With regard to distribution by sex, AVNRT ablation was predominantly performed on females (69%), and AF ablation (75%) and ventricular tachycardias (68%) (associated or not with structural heart disease) were performed predominantly on males. As the data shows, these data are very similar to those reported in previous registries.1, 2, 3, 4, 5, 6, 7, 8, 9.
Similarly, 30% of patients had a history of structural heart disease, and the presence of left ventricular dysfunction is generally limited to patients who underwent AVN ablation and ventricular tachycardia associated with heart disease. The same distribution was observed in implantable automatic defibrillator patients.
Infrastructure and ResourcesTable 1, Table 2 show the technical and human resources available in laboratories participating in the registry, as well as their activities. One of the centers treated pediatric patients exclusively.
Table 2. Change in Human Resources in Public Hospital Laboratories Participating in the Registry Since 2002.
| 2010 | 2009 | 2008 | 2007 | 2006 | 2005 | 2004 | 2003 | 2002 | |
| Staff physicians, no. | 2.8 | 2.6 | 2.5 | 2.4 | 2.3 | 2.2 | 2.2 | 2.2 | 2.2 |
| Fulltime physicians, no. | 2.3 | 2.1 | 2.1 | 2.1 | 1.8 | 1.7 | 1.6 | 1.4 | 1.6 |
| Fellowship students/y, no. | 0.7 | 0.8 | 0.6 | 0.6 | 1.3 | 0.6 | 0.7 | 0.6 | 1 |
| NGD, no. | 2.4 | 2.2 | 2.2 | 2 | 1.7 | 1.7 | 1.6 | 1.6 | 1.5 |
| TAR, no. | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 | 0.2 | 0.2 | 0.2 | 0.2 |
NGD, nurses with graduate degree; TAR, technical assistant in radiology.
A total of 44 centers (77%) had at least 1 laboratory exclusively dedicated to electrophysiology, and 7 centers (12%) had 2 laboratories. The mean number of days that the laboratory was available per week was 3.8 (1.4) days; median, 4.
Most laboratories also implanted devices, mainly defibrillators: 39 (68%) laboratories implanted defibrillators and pacemakers, and 3 (5%) laboratories implanted only defibrillators. External electric cardioversion was performed in 38 (67%) laboratories and internal cardioversion in 9 (16%) laboratories.
All centers had digital polygraphy, 72% had digital radiology, and 53% had portable fluoroscopy. A nonfluoroscopic navigation system (NFNS) was available in 84% of centers, with 20 centers having 2 NFNSs and 3 centers having 3 NFNSs. Some 91.5% of public centers had a NFNS while only 50% of private centers had one.
Since 2008, only 3 centers have had access to a magnetic navigation system and only 1 to a robot navigation system. Intracardiac echocardiography was available in 21 centers. Cryoablation was performed in 21 centers (37%) and, for the first time, 1 center had access to ultrasound ablation.
The number of healthcare staff in the electrophysiology laboratories remained largely unchanged. Although the percentage of centers that had more than 1 full-time physician (79%) remained stable, the number of centers with more than 2 physicians on staff increased to 45%. There were at least 2 full-time nursing graduates in 89% of laboratories. The number of centers staffed with electrophysiology fellowship students decreased from 30 centers in 2009 to 20 centers in 2010. Among the centers with fellowship students, the average was 1.75 students per center.
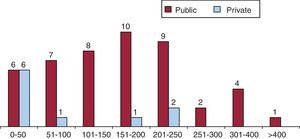
RESULTSAlthough 2 fewer centers participated this year than in the previous registry, the number of ablation procedures reported again increased, with a total of 8762 procedures reported by 57 participating centers (Figure 1, Figure 2). This represents a mean of 154 (97) ablations per center, with a median of 156 and a range of 5 to 462.
Figure 2. Number of electrophysiology laboratories in the Spanish Registry by number of ablation procedures performed during 2010.
Excluding AF and VT-AMI substrates, the overall success rate was 94% (6690/7173). A total of 145 complications (1.7%) was reported for all ablation procedures (including AF and VT-AMI). A total of 5 deaths (0.06%) was reported: 1 AF ablation (patient suffered a stroke 48h after the procedure), 1 AP ablation (patient had a pulmonary thromboembolism), 1 CTI ablation (patient suddenly died overnight, 36h after the procedure), 1 related to a VT-AMI ablation (due to cardiac tamponade and secondary ventricular fibrillation) and 1 related to VT-NAMI (due to cardiac tamponade). Two cases of pulmonary thromboembolism were reported, related to an AP ablation (which was the cause of death) and to an AVNRT. A total of 8 iatrogenic atrioventricular (AV) blocks (0.1%) occurred, requiring implantation of permanent pacemakers: 3 during AVNRT ablation, 2 for AP ablation, 2 during CTI ablation, and 1 during a VT-NAMI ablation.
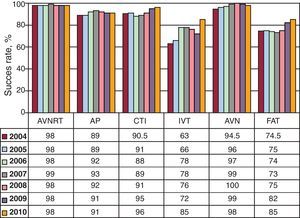
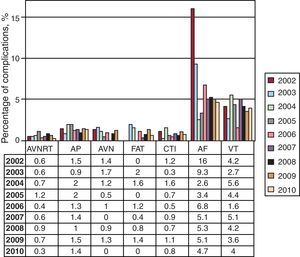
Figure 3, Figure 4 show the overall success and complication rates compared to those of previous years. In the last 6 years, the reported success rate for FAT and IVT ablation has increased by more than 10%, while remaining stable for the other substrates.
Figure 3. Change in catheter ablation success rates since 2004, by substrate treated. AP, accessory pathways; FAT, focal atrial tachycardia; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; IVT, idiopathic ventricular tachycardia.
Figure 4. Percentage of complications in catheter ablation since 2004, by substrate treated. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
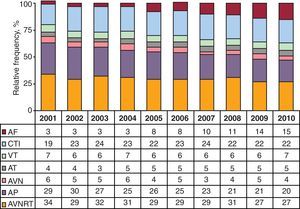
In terms of frequency of the substrates treated, AVNRT was still the most common procedure, with CTI ablation firmly established in second place (Figure 5). The least treated substrate was VT-NAMI. The number of ablation procedures performed remained stable for all substrates, except for AF and ventricular tachycardia, which increased. The number of AF ablation procedures increased by 10% compared to last year, representing 15.3% of all procedures performed. The evolution of the relative frequency of different substrates treated from 2001 is shown in Figure 6.
Figure 5. Relative frequency of different substrates treated by catheter ablation in Spain during 2010 (pie diagram). For each substrate, the total number of cases performed in 2010 is shown. In the upper part of the bars, the percentage change from the 2009 registry is shown. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia / atypical atrial flutter; VT-AMI, ventricular tachycardia with acute postinfarction scarring; VT-HD, ventricular tachycardia associated with heart disease.
Figure 6. Change in the relative frequency of different substrates treated since 2001. AF, atrial fibrillation; AP, accessory pathways; AT, atrial tachycardia; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
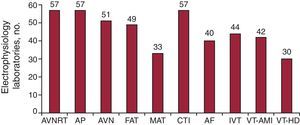
All hospital centers performed AVNRT, CTI, and AP ablations (Figure 7). The substrate treated in the lowest percentage of centers was VT-NAMI (51%). The number of centers performing AF ablation continues to increase progressively, and has reached 70% of all centers (n=40) and 74.5% of centers belonging to the public system.
Figure 7. Number of electrophysiology laboratories participating in the Spanish registry that treat each of the substrates. AF, atrial fibrillation; AP, accessory pathways; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia / atypical atrial flutter; VT-AMI, ventricular tachycardia with postinfarction scarring; VT-HD, ventricular tachycardia associated with heart disease.
The following section describes the data analyzed according to the specific arrhythmia substrates.
Atrioventricular Nodal Reentrant TachycardiaThis was the most commonly treated substrate and was performed in all centers. A total of 2321 ablation procedures were performed, 27% of all procedures. The mean number of AVNRT procedures per center was 41 (22), range, 1 to 115. The success rate for procedures was 98.4% (2283/2321), and 34 centers (60%) achieved 100% success. There were 8 complications (0.34%): 3 cases (0.13%) of AV block requiring permanent pacemakers, 3 cases of vascular access complication, 1 case of stroke, and 1 case of pulmonary thromboembolism.
The most commonly used ablation catheter was the conventional 4-mm tip radiofrequency catheter, although there was a slight increase in the use of other catheters. In particular, nonconventional ablation catheters were used in 176 cases (7.6%): 92 irrigated tip catheters, 62 cryoablation catheters, and 22 8-mm tip catheters.
Cavotricuspid IsthmusThe second most frequent procedure was CTI ablation. A total of 1839 ablation procedures was performed (mean 32 [23]), which were successful in 1774 cases (96.5%). All centers treated this substrate, and 26 centers reported 100% success. There were 15 major complications (0.8%): 9 vascular complications, 2 cases of AV block requiring implantation of permanent pacemakers, 3 episodes of heart failure, and 1 death. The death occurred suddenly during the night, 36h after the procedure.
The use of the 4-mm tip ablation catheter was rare (1%) in this substrate. The centers used 985 irrigated tip catheters, 821 8-mm tip catheters, and 12 cryoablation catheters.
Accessory PathwaysThis was the third most often treated substrate. A total of 1738 AP ablation procedures were performed, with a mean of 32 (19) per center (range, 1-77). There were 1589 successful procedures (91%) and only 8 of the 49 centers that performed more than 10 AP ablation procedures reported 100% success. A total of 24 (1.4%) major complications occurred: 12 vascular complications, 6 pericardial effusions, 2 strokes (1 of them hemorrhagic), 2 AV blocks requiring permanent pacemakers, 1 myocardial infarction, and 1 death. The cause of death was pulmonary thromboembolism.
Conventional ablation catheters were not used in 208 cases (12%). The centers used 127 irrigated tip catheters, 14 8-mm tip catheters, and 73 cryoablation catheters.
The location of the ablated AP was reported in 1626 cases (93.6%). As in previous registries, the most common locations were the left ventricular free wall (52%) and the inferior paraseptal pathways (24.4%). The least treated locations were still the peri-Hisian or superior paraseptal pathways (9%). The success of the procedures depended on the location of the AP: 94% (792/845) for ablations in the left free wall, 92% (219/239) for the right free wall, 88% (347/396) for the inferior paraseptal pathways, and 80% (117/146) in the peri-Hisian or superior paraseptal pathways.
Atrioventricular Node AblationThis substrate remains steady in fourth place in terms of procedures per year. The total number of procedures was 393 and was successful in 98.2% of cases. This year there were no complications reported during treatment of this substrate.
Conventional ablation catheters were not used in 52 cases: 28 8-mm tip catheters and 24 irrigated tip catheters were used instead. This year, the use of cryoablation catheters for this substrate was discontinued.
Focal Atrial TachycardiaIn total, 279 FAT ablation procedures were performed, with a success rate of 85% (237/279). The mean number of procedures per center was 5 (4). This substrate was treated in the right atrium in 45 centers, but only 32 centers treated it when located in the left atrium. The origin of the FAT was reported in 273 cases, and the success rate of the procedure was slightly higher for those originating in the right atrium: 86% for those in the right atrium (163/189) compared to 82% for those in the left atrium (69/84).
A total of 2 complications (0.7%) were recorded: 1 pericardial effusion and 1 stroke.
Special catheters were used in 77 cases: irrigated tip catheters (65), 8-mm tip catheters (5), and cryoablation catheters (7).
Macroreentrant Atrial Tachycardia / Atypical Atrial FlutterThis substrate was treated by 33 centers (58%), with a total of 186 procedures (mean, 5.6 [range, 1-19] procedures per center). The procedure was successful on 142 occasions (76%). There were 3 complications (1.6%): 2 strokes, 3 femoral vascular complications, and 1 cardiac tamponade.
The origin of the MAT was reported for 181 procedures: 86 right origin cases and 95 left cases, with a success rate of 85% and 68%, respectively. A catheter other than the conventional 4-mm tip was used in 90% of cases, mostly irrigated tips (95%).
Atrial FibrillationIn total, 1309 AF ablation procedures (range, 2-119) were performed among 40 of the participating centers (70%). This is a mean of 32 procedures per center, although 15 laboratories performed fewer than 15 procedures; 9 centers performed more than 50 and only 2 performed more than 100 procedures.
The technique used was indicated in 1206 procedures (92%). Ostial electrical disconnection was performed in 27% of cases, with circumferential isolation in 70% of cases, and circumferential isolation with discharge reduction in the remaining 3%. The superior vena cava was also electrically disconnected in 22 procedures.
Almost all groups used irrigated tip ablation catheters (96%). A total of 52 cryoenergy balloon ablation procedures were performed, along with 23 single-shot and 3 basket catheter ablations.
A total of 62 complications (4.7%) was recorded: significant pericardial effusion / cardiac tamponade (28), acute coronary syndrome (2), vascular access problems (15), stroke (7), phrenic nerve palsy (4), and pulmonary vein stenosis (6). There was 1 death 48h after surgery due to ischemic stroke.
Idiopathic Ventricular TachycardiaA total of 299 IVT ablation procedures was reported for 44 centers (mean, 7 [range, 1-25] ablations per center). Success was achieved in 255 procedures (85%) and there were only 3 complications (1%): 2 tamponades and 1 femoral pseudoaneurysm.
The type of ablated ventricular tachycardia was reported for 288 procedures: 176 occurred in the right ventricular outflow tract and 45 in the left ventricular outflow tract, 37 were fascicular, and 30 were reported as “other” location. The success rates for the above ablations were 89%, 75%, 86%, and 73%, respectively.
The irrigated tip ablation catheter was used in half of the cases, its use reaching 88% for left ventricular tachycardia.
Ventricular Tachycardia With Postinfarction ScarringA total of 42 (73%) centers performed 280 VT-AMI ablation procedures (6 [range, 1-27] ablations per center). The complications (n=19, 6.8%) were vascular access (5), cardiac tamponade (9), stroke (1), acute heart failure (2), and acute coronary syndrome (2). One patient died after suffering a cardiac tamponade (effective drainage) due to refractory ventricular fibrillation.
The type of ablation performed was reported in 265 cases: 68 used a “conventional” approach and 197 used a substrate approach. The irrigated tip ablation catheter was used for these types of ablations in almost all cases. Compared to 2009, there has been a marked increase in substrate ablations (77%) and a moderate decrease in ventricular tachycardia mapping ablations (26%).
The success rate reported for the conventional approach (noninducibility of clinical tachycardia after ablation) was 76.5%.
Ventricular Tachycardia Not Associated With Postinfarction ScarringA total of 118 ablation procedures was performed for this substrate in 29 laboratories (50%). There were 6 complications: 4 tamponades, 1 complete AV block, and 1 vascular fistula at the femoral level. One patient with incessant ventricular tachycardia died after suffering a cardiac tamponade.
The types of heart disease associated with the ablated ventricular tachycardias were arrhythmogenic right ventricular dysplasia (30), branch to branch (7), nonischemic dilated cardiomyopathy (37), and “other” (28). The success achieved was 73%, 85%, 59%, and 82%, respectively. One procedure was epicardial.
A nonstandard ablation catheter was used in 74% of the procedures: an 8-mm tip catheter was used in 3 cases and irrigated tip catheters were used in 84 cases.
DISCUSSIONAs in previous years, 2010 has seen a steady increase in activity in the arrhythmia units in Spain. The high participation in this registry (57 centers, 2 fewer than last year) and number of procedures (exceeding 8700 procedures for the first time) ensures the representative nature of the data recorded in this registry. More ablations have been reported from fewer centers, which means that the average number of procedures per center has increased.
This increased number of ablations carries with it a slight but hopeful numerical improvement in human resources, a distinguishing feature of this 2010 registry. It is surprising, however, that the number of centers with available fellowship students has clearly decreased, a fact that must be carefully assessed.
This year's distribution of substrates presents several noteworthy peculiarities. Firstly, stability has been achieved in the number of procedures for the so-called “conventional” substrates, with CTI once again being the second most commonly treated substrate in absolute numbers. The trend toward complex atrial procedures (ie, AF and MAT) has been disparate: AF ablation has increased by 10%, with an absolute number of procedures per center similar to last year, and this increase has been more moderate (10% vs 44% for 2009); MAT ablation has decreased by 7% (last year it increased by 40%). There may be various explanations for this trend, including its lower incidence and the complexity in performing the procedure. Additionally, the complication rate for AF ablation remains stable, with this substrate being one of the main substrates in a number of Spanish laboratories. Interestingly, in some laboratories it is the most treated substrate.
It is also of utmost importance to note that this year the greatest increase in ablation procedures took place in ventricular arrhythmias. This increase has been outstanding: some 20% of procedures on patients with heart disease and 57% in IVT. These results counter our pessimism from previous years with regard to these substrates.
Therefore, it seems that in coming years we will witness a slowdown in the number of procedures on “standard” substrates, with a variable but increasing number of AF and ventricular arrhythmia ablations.
CONCLUSIONSThe 2010 Spanish Catheter Ablation Registry, as in previous years, includes one of the largest samples published to date in the international literature on ablation procedures, and exceeds the 8500 ablations performed last year. The high participation, with the collaboration of 57 electrophysiology laboratories, makes the data recorded from this activity and the results of this procedure in Spain extremely reliable. The success rate of this procedure in Spain remains high (>90%), with a low rate for major complications (<2%) and mortality (0.06%). Ventricular arrhythmia ablation in patients with or without heart disease has experienced the greatest increase in number of procedures compared to previous years. CTI ablation as treatment for typical atrial flutter remains the second most frequently treated arrhythmic substrate.
CONFLICTS OF INTERESTNone declared.
Acknowledgements
The registry coordinators would once again like to express their appreciation to all those who participated in the 2010 Ablation Registry, and who voluntarily and selflessly sent data on their procedures. They also thank Cristina Plaza for her excellent and tireless administrative work.
Appendix 1. Electrophysiology Laboratories that Participated in the 2010 Spanish Catheter Ablation Registry by Autonomous Communities and Provinces (in parentheses, the doctor responsible for the registry)| Andalusia | |
| Cordoba | Hospital Reina Sofía (Dr. J. Segura) |
| Granada | Hospital Virgen de las Nieves (Dr. M. Álvarez) |
| Huelva | Hospital Juan Ramón Jiménez (Dr. P. Moriña) |
| Malaga | Hospital Clínico de Málaga (Dr. J. Alzueta), Hospital Quirón (Dr. M. Álvarez) |
| Seville | Hospital Virgen Macarena (Dr. E. Díaz Infante), Hospital Virgen del Rocío (Dr. A. Pedrote), Hospital Virgen de Valme (Dra. D. García Medina), Hospital Nisa Aljarafe (Dr. E. Díaz Infante) |
| Aragon | |
| Zaragoza | Hospital Lozano Blesa (Dr. G. Rodrigo), Hospital Miguel Servet (Dr. A. Asso), Clínica Quirón (Dr. A. Asso) |
| Principality of Asturias | Hospital Central de Asturias (Dr. J.M. Rubín) |
| Balearic Islands | |
| Mallorca | Hospital Son Llàtzer (Dr. X. Fosch), Clínica Rotger (Dr. X. Viñolas) |
| Canary Islands | Hospital Nuestra Señora de la Candelaria (Dr. R. Romero), Hospital Universitario de Canarias (Dr. A. Rodríguez), Hospital Insular (Dr. F. Segura) |
| Cantabria | Hospital Marqués de Valdecilla (Dr. F.J. Rodríguez) |
| Castile-La-Mancha | |
| Toledo | Hospital Virgen de la Salud (Dr. M.A. Arias) |
| Castile and León | |
| Burgos | Hospital General Yagüe (Dr. J. García) |
| Leon | Hospital de León (Dra. M.L. Fidalgo) |
| Salamanca | Hospital Clínico Universitario (Dr. J.L. Moríñigo) |
| Valladolid | Hospital Río Hortega (Dr. B. Herreros), Hospital Clínico Universitario (Dr. J. Rubio) |
| Catalonia | |
| Barcelona | Hospital de Bellvitge (Dr. X. Sabaté), Hospital del Mar (Dr. J. Martí), Hospital Clínic (Dr. L. Mont), Hospital Vall d’Hebron (Dra. N. Rivas), Hospital de la Santa Creu y Sant Pau (Dr. J. Guerra), Hospital Sant Joan de Déu (Dra. G. Sarquella), Hospital Mútua de Terrassa (Dra. S. Ibars), Clínica El Pilar (Dr. J. Brugada), Clínica Sagrada Família (Dr. A. Moya), Clínica Teknon (Dr. E. Rodríguez) |
| Lérida | Hospital Arnau de Vilanova (Dra. M. Matiello) |
| Valencian Community | |
| Alicante | Hospital Universitario de Alicante (Dr. J.G. Martínez) |
| Valencia | Hospital Clínico (Dr. A. Martínez) |
| Extremadura | |
| Badajoz | Hospital Infanta Cristina (Dr. M. Doblado) |
| Galicia | |
| A Coruña | Hospital Universitario de A Coruña (Dra. L. Pérez), Hospital Clínico Universitario de Santiago (Dr. J.L. Martínez Sande) |
| Community of Madrid | Hospital Ramón y Cajal (Dr. R. Matía); Hospital Puerta de Hierro (Dr. I. Fernández Lozano), Hospital 12 de Octubre (Dr. R. Salguero), Hospital Clínico San Carlos (Dr. N. Pérez Castellano), Hospital Gregorio Marañón (Dr. A. Arenal), Fundación Jiménez Díaz (Dr. J.M. Rubio), Hospital La Paz (Dr. R. Peinado), Grupo Hospitales de Madrid (Dr. J. Almendral), Fundación Hospital Alcorcón (Dr. Rubio) |
| Region of Murcia | Hospital Virgen de la Arrixaca (Dr. A. García Alberola), Hospital Santa María del Rosell (Dr. I. Gil) |
| Chartered Community of Navarre | Clínica Universitaria de Navarra (Dr. A. Macías), Hospital de Navarra (Dra. N. Basterra) |
| Basque Country | |
| Vizcaya | Hospital de Cruces (Dr. A. Bodegas), Hospital de Basurto (Dra. M.F. Arcocha) |
| Alava | Hospital de Txagorritxu (Dr. J. Pindado) |
Corresponding author: Irunlarrea 13, 8.°-D, 31008 Pamplona, Spain. igarciab@unav.es