This report presents the findings of the 2015 Spanish Catheter Ablation Registry.
MethodsFor data collection, each center was allowed to choose freely between 2 systems: retrospective, requiring the completion of a standardized questionnaire, and prospective, involving reporting to a central database.
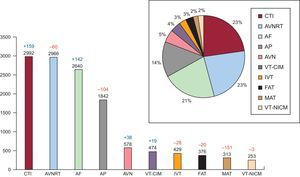
ResultsData were collected from 82 centers. A total of 12 863 ablation procedures were performed, for a mean of 157±119 and a median of 138 procedures per center. The ablation target most frequently treated was cavotricuspid isthmus (n=2992 [23.2%]), followed by atrioventricular nodal reentrant tachycardia (n=2966 [23%]) and atrial fibrillation (n=2640 [20.5%]). There were fewer ablation procedures for atrial tachycardia, idiopathic ventricular tachycardia and accessory pathways, while those for ventricular tachycardia in ischemic cardiomyopathy remained steady. The overall success rate, excluding atrial fibrillation and ventricular tachycardia in cardiomyopathy, was 87.5%, the rate of major complications was 2%, and the mortality rate was 0.08%.
ConclusionsThe 2015 registry is the first to show a slight reduction in the number of centers sending in their results and in the total number of ablation procedures performed. The most frequently treated substrate was the cavotricuspid isthmus. There was also a slight decrease in the success rate. The complications and mortality rates remained low.
Keywords
The purpose of the present article is to communicate the findings of the Spanish Catheter Ablation Registry, the Official Report of the Working Group on Electrophysiology and Arrhythmias of the Spanish Society of Cardiology for 2015, thus marking the 15th year of uninterrupted activity by this group1–14. The registry is a voluntary nationwide record, published annually, that includes data from most of the arrhythmia units operating in Spain, making it one of the few large-scale, observational registries focusing on catheter ablation.
The main objectives of the registry are to observe and describe developments in the interventional treatment of cardiac arrhythmias in Spain and to provide reliable information on the type of activity carried out and the facilities available in Spanish arrhythmia units.
METHODSAs in previous years, 2 different systems, 1 prospective and the other retrospective, were used for data collection. For the prospective method, the registry provided a standardized database that required the introduction of individual patient data. The retrospective approach involved completing a standardized questionnaire that was sent to all the participating interventional electrophysiology laboratories in January 2016; the questionnaire was also available on the website of the Working Group on Electrophysiology and Arrhythmias15. All the data compiled by both systems remained anonymous, even to the registry coordinators. The secretariat of the Spanish Society of Cardiology ensured that the participating centers could not be identified.
The information collected concerned the technical and human resources available in the arrhythmias units, the procedures performed, and the patients’ demographic data. As in previous years, the data on human resources included information only from centers in the publicly-funded health system, and the epidemiologic variables included only those from patients treated in centers using the prospective data collection method.
We analyzed the same 10 arrhythmias and arrhythmogenic substrates that were examined in previous registries: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathway, atrioventricular node (AVN), focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia in ischemic cardiomyopathy (VT-ICM), and ventricular tachycardia in nonischemic cardiomyopathy (VT-NICM). The following variables common to these 10 conditions were analyzed: number of patients and procedures performed, success rate, type of ablation catheter used, and number and type of procedure-related complications, including periprocedural death. In addition, we analyzed a number of substrate-specific variables, such as the anatomic location and type of accessory pathway conduction, the location and mechanism of atrial tachycardia, and the type of ventricular tachycardia.
As in previous years, the success rate refers only to the immediate postprocedural data (acute success rate). The number of recurrences could not be determined because there was no follow-up analysis. Several therapeutic approaches with different objectives can be used to treat AF and VT-ICM, and the criteria for success/failure may differ depending on the technique applied. Thus, AF, VT-ICM, and VT-NICM were excluded from the analysis of the overall outcome of ablation procedures. As for complications, only those occurring during the hospital stay following the procedure were reported.
Statistical AnalysisContinuous variables are expressed as the mean±standard deviation. Differences between continuous variables were evaluated using the Student t test for dependent or independent samples, as appropriate. Differences between categorical variables were assessed using the chi-square or Fisher exact test. Statistical significance was set at a P value of<.05. The statistical analysis was carried out using an SPSS (20.0) database.
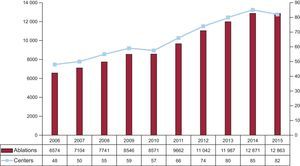
RESULTSIn contrast to the findings in previous registries, the number of participating centers did not increase this year. Eighty-two centers participated in the 2015 registry (Appendix 2) and, for the first time, the total number of procedures did not increase, but remained steady or decreased slightly compared with the previous year (Figure 1). The participating centers included 61 (74.4%) from the public health care system and 21 (25.6%) from the private sector.
As has been the case in previous years, the approach most widely used was retrospective data collection. Only 9 centers (11%) provided prospectively collected data.
The participating hospitals continued to be mainly tertiary (85.4%) and teaching (72%) centers. Patients were attended in cardiology departments in 81 centers (98.8%) and 63.8% had cardiac surgery units.
Epidemiological CharacteristicsThe epidemiological characteristics were analyzed using only the prospective data collected in 9 centers, with a total of 1959 ablation procedures.
The overall mean age of the patients was 58±31 years; the youngest were those with an accessory pathway (43±16 years) and the oldest, those who underwent AVN ablation (70±11 years). Regarding the sex distribution, women predominated in AVNRT ablation (72%), whereas men predominated in ablation for ventricular tachycardia (74%), with or without associated structural heart disease, MAT (70%), and AF (66%).
In all, 18.3% of the patients had a history of structural heart disease, and left ventricular dysfunction was generally limited to patients undergoing ablation of AVN, VT-ICM, or VT-NICM.
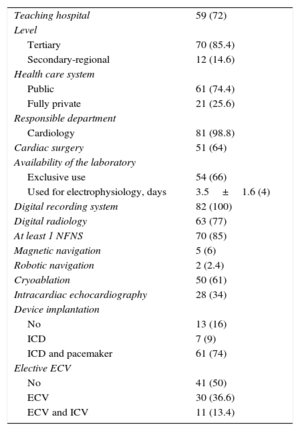
Infrastructure and ResourcesThe technical and human resources available in the participating laboratories and the activity carried out are presented in Table 1 and Table 2.
Characteristics and Infrastructure of the 82 Electrophysiology Laboratories Participating in the 2015 Registry
| Teaching hospital | 59 (72) |
| Level | |
| Tertiary | 70 (85.4) |
| Secondary-regional | 12 (14.6) |
| Health care system | |
| Public | 61 (74.4) |
| Fully private | 21 (25.6) |
| Responsible department | |
| Cardiology | 81 (98.8) |
| Cardiac surgery | 51 (64) |
| Availability of the laboratory | |
| Exclusive use | 54 (66) |
| Used for electrophysiology, days | 3.5±1.6 (4) |
| Digital recording system | 82 (100) |
| Digital radiology | 63 (77) |
| At least 1 NFNS | 70 (85) |
| Magnetic navigation | 5 (6) |
| Robotic navigation | 2 (2.4) |
| Cryoablation | 50 (61) |
| Intracardiac echocardiography | 28 (34) |
| Device implantation | |
| No | 13 (16) |
| ICD | 7 (9) |
| ICD and pacemaker | 61 (74) |
| Elective ECV | |
| No | 41 (50) |
| ECV | 30 (36.6) |
| ECV and ICV | 11 (13.4) |
ECV, external cardioversion; ICD, implantable cardioverter-defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
Data are expressed as No. (%) or mean±standard deviation (median).
Changes in the Human Resources in the Electrophysiology Laboratories of Public Hospitals Participating in the Registry Since 2006 (Mean No. per Hospital)
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Staff physicians | 2.3 | 2.4 | 2.5 | 2.6 | 2.8 | 2.6 | 2.7 | 2.8 | 2.8 | 3.0 |
| Full-time physicians | 1.8 | 2.1 | 2.1 | 2.1 | 2.3 | 2.2 | 2.1 | 2.0 | 1.9 | 2.4 |
| Residents/y | 1.3 | 0.6 | 0.6 | 0.8 | 0.7 | 0.7 | 0.7 | 0.6 | 0.6 | 0.8 |
| RN | 1.7 | 2.0 | 2.2 | 2.2 | 2.4 | 2.3 | 2.3 | 2.2 | 2.3 | 2.7 |
| RT | 0.3 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 |
RN, registered nurse; RT, radiologic technologist.
Fifty-four centers (66%) were equipped with at least 1 dedicated cardiac electrophysiology laboratory, 9 centers (11%) had 2 such laboratories, and 1 center had 3. Similar to previous years, on average, the laboratory was available on 3.5±1.6 (median, 4) days a week. Only 4 of the 21 private centers had a laboratory devoted exclusively to cardiac electrophysiology.
Half of the laboratories (n=41) did not perform external electric cardioversion, and internal cardioversion was done in 11 centers. Implantation of cardiac pacing devices was carried out in 69 centers (84%): implantation of both defibrillators and pacemakers was performed in 74% of the laboratories and defibrillator implantation alone in 9%. None of the centers implanted pacemakers only.
All of the participating centers were equipped with a digital recording system and 77% with digital radiography. A single nonfluoroscopic navigation system was available in 85% of the centers; 29% had 2 such systems and 2.4% had 3, without substantial differences with respect to the 2014 registry. Of note, nonfluoroscopic navigation systems were more widely available in public health care centers than in private centers (93% vs 52%, respectively).
Five centers had a magnetic navigation system and 2 had a robotic navigation system. The number of sites performing intracardiac echocardiography increased (n=28; 34% vs 21% in the 2014 registry). In 2015, ultrasound ablation was available at 2 sites, the number of centers offering cryoablation continued to grow, from 56% in 2014 to 61% in 2015.
Table 2 shows the main findings regarding human resources. Although 80% of the centers had more than 1 full-time physician and 41% more than 2, 15 centers (18%) had no full-time physicians. The staffs of 85% of the laboratories included at least 2 full-time registered nurses. In 2015, 25 centers had resident physicians, usually 1 or 2.
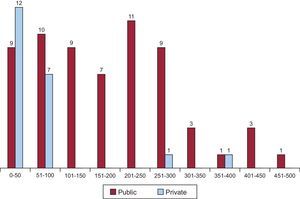
Overall ResultsIn this registry, the number of participating centers decreased for the first time, from 85 in 2014 to 82 (Figure 1) A total of 12 863 procedures were reported, a number that is also lower than that of the previous registry. This yields a mean of 157±119 procedures and a median of 138 per site, higher than that of the 2014 registry (149.5±103 per center; median, 124). The range of ablations was nearly identical to that of 2014 (Figure 2). Of the publicly-funded health centers, 8 carried out more than 300 ablations and 4 of them, more than 400. Only 9 private centers performed more than 50 ablation procedures in 2015, but 2 of them exceeded 250.
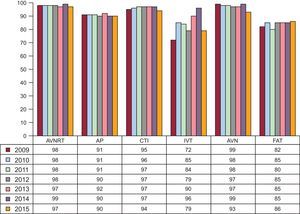
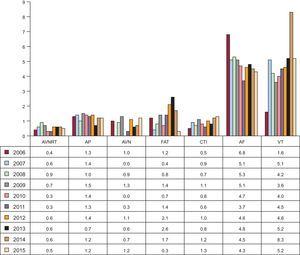
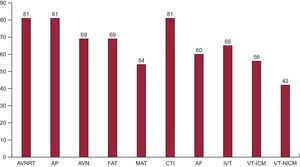
Figure 3 and Figure 4 show the overall results in terms of both successful outcomes and complications, and they are compared with those of previous registries. The overall success rate, excluding the treatment of AF, VT-ICM, and VT-NICM, was 87.5%. The percentages of success in the different ablation targets demonstrate that the rates in the most common arrhythmias and arrhythmogenic substrates and in VT-ICM remained steady and that there was a substantial decrease, between 2014 and 2015, in the success rate for MAT (from 87.7% to 74.4%) and IVT (from 96% to 79%). The number of complications notified in all of the ablation procedures (including AF, VT-ICM, and VT-NICM) was 269 (2%), higher than those reported in 2013 and 2014. The most common complications were vascular (33%), followed by pericardial effusion/cardiac tamponade (30%). There were 13 cases of iatrogenic atrioventricular block (0.1% of all the ablation procedures) requiring permanent pacemaker implantation: 8 during AVNRT ablation, 3 during accessory pathway ablation, 3 during VT-ICM ablation, and another during MAT ablation. Eleven periprocedural deaths were recorded (0.08%), 3 more than the year before. As in the 2014 registry, 3 of the deaths occurred in procedures involving low-risk ablation targets: 1 in AVNRT and 2 in accessory pathways. The other 8 deaths involved high-risk targets: VT-ICM in 6, VT-NICM in 1, and AF in 1.
Changes in catheter ablation success rates since 2009 by the arrhythmia or arrhythmogenic substrate treated. AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia.
Percentage of major complications related to catheter ablation since 2006 by the arrhythmia or arrhythmogenic substrate treated. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
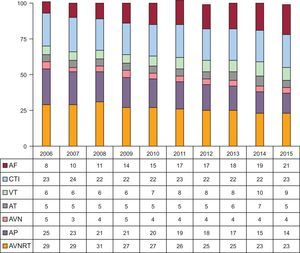
Regarding the frequency of treatment in each arrhythmia or arrhythmogenic substrate, CTI was the most prevalent (23.2%), followed by AVNRT (23%). Ablation of AF was the third most frequently performed intervention (20.5%). Ablation for VT-NICM continued to be the least common procedure (2%). Compared with the 2014 registry, there were increases in the number of ablations of AF, CTI, VT-ICM, and AVN and decreases in those involving accessory pathways and MAT (Figure 5). The changes in the relative frequency of the different ablation targets since 2006 are shown in Figure 6. Since the registry was first published, there have been increases in the ablation of AF and ventricular tachycardia and a gradual, progressive decrease in accessory pathway ablation.
Relative frequency of arrhythmias and arrhythmogenic substrates treated by catheter ablation in Spain in 2015 (n=12 863). The change in the number of cases compared with the 2014 registry is shown for each ablation target. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-ICM, ventricular tachycardia in ischemic cardiomyopathy; VT-NICM, ventricular tachycardia in nonischemic cardiomyopathy.
Changes in the relative frequency of different ablation targets treated since 2006. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; AT, atrial tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
In 2015, AVNRT, CTI, and accessory pathway ablation were performed in 81 of the 82 centers (Figure 7). The number of sites carrying out AF ablation increased from 50 in 2012 to 60 in 2015, representing 73% of all the centers. The ablation target treated in the fewest centers continued to be VT-NICM (42 of the 82).
Number of electrophysiology laboratories participating in the registry that treat each of the different ablation targets. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-ICM, ventricular tachycardia in ischemic cardiomyopathy; VT-NICM, ventricular tachycardia in nonischemic cardiomyopathy.
The following sections summarize the results of the data analysis for each specific arrhythmia or arrhythmogenic substrate.
Atrioventricular Nodal Reentrant TachycardiaIn 2015, AVNRT was the second most frequently targeted condition, and its ablation was performed in 98.8% of the centers. A total of 2966 ablations of AVNRT were carried out (23% of all the ablation procedures), with a mean number per site of 35.6±25.6 (range, 2-115). The success rate was 97.4%, and 53 centers (65%) reported a rate of 100%. Fifteen major complications were notified (0.5%): 8 cases of atrioventricular block requiring a permanent pacemaker, 5 vascular access complications, 1 stroke, and 1 case of pericardial effusion or tamponade. One death was reported in a 15-year-old patient; the cause remains unclear. The most commonly used ablation catheter was a standard 4-mm tip radiofrequency catheter. In addition, an irrigated tip catheter was used in 52 cases (1.7%), and a cryoablation catheter in 91 (3%).
Cavotricuspid IsthmusIn 2015, ablation of the CTI was the procedure most frequently performed in our laboratories and was carried out in 98.8% of the centers. In all, there were 2992 CTI ablation procedures (23.2%), with a mean of 36.9±28 (range, 1-106) procedures per center. Success was reported in 93.6% of the cases, with a 100% success rate in 47 centers (57%). There were 39 major complications (1.3%), including 15 vascular complications, 2 episodes of stroke, 2 cases of heart failure, and 1 case of pericardial effusion/tamponade. The data available in the registry specify that 1666 irrigated tip catheters (55.7%), 1062 8-mm tip catheters (35.5%), 63 10-mm tip catheters (2.1%), and 23 cryoablation catheters (0.8%) were employed.
Accessory PathwaysOnce again, accessory pathway ablation was the fourth most frequently performed procedure; it was carried out in 98.8% of the centers and, again, there was a decrease in the number of interventions compared respect to 2014. There were 1842 procedures, yielding a mean of 22.7±16 per site (range, 2-77). A successful outcome was reported in 1649 (89.5%) procedures, and a success rate of 100% was achieved in 21 centers. However, if we analyze only the 58 performing more than 10 accessory pathway ablation procedures annually, this figure is reduced to 13 sites. Although many centers still do not provide information on the direction of accessory pathway conduction, the available data indicate that 47.2% of the pathways exhibited bidirectional conduction; conduction was exclusively anterograde in 8.8% and retrograde in 44%. With respect to their locations, there were no marked changes in the distribution. Left-sided accessory pathways continued to be those most frequently found (56.7%), followed by inferoseptal (26.1%), and right-sided (13.5%). Parahisian pathways were the least common (10.3%). Procedural success by location was as follows: left ventricular free wall, 95.4%; right ventricular free wall, 92.1%; inferoparaseptal, 90.2%; and parahisian/anteroseptal, 81.2%. There were 22 major complications (1.2%), including 11 vascular complications, 5 cases of pericardial effusion, 2 acute coronary events (in 1 of them, the records specify that it was secondary to coronary spasm 3hours after ablation and was resolved with intravenous nitroglycerin), and 4 cases of atrioventricular block, 3 of which required a permanent pacemaker. Two deaths were reported as complications of accessory pathway ablation. No information was provided on 1 of these deaths; the other was secondary to cardiac tamponade, and the autopsy revealed a multivalvular malformation with leaflet dysplasia. The use of unconventional ablation catheters increased compared with 2014: irrigated tip catheters were used in 333 cases (18%), cryoablation catheters in 112 (6%), and 8-mm tip catheters in 2 (0.1%).
Atrioventricular Node AblationIn all, 578 atrioventricular node ablation procedures were reported by 69 centers. Success was achieved in 92.7% of the cases. There were 7 complications (1.2%): 6 vascular complications and 1 case of heart failure. Ablation catheters other than the standard 4-mm tip catheters were used in 186 cases (32.2%): 79 irrigated tip catheters (13.7%) and 111 8-mm tip catheters (19.2).
Focal Atrial TachycardiaIn all, 376 FAT ablation procedures were performed in 69 centers, with an overall success rate of 85.9%. The available data show that the intervention was performed for FAT localized in right atrium in 274 cases (88.7% of which were successful) and in left atrium in 73 (83.5% successful). One vascular complication (0.3%) was reported. In all, 191 (50.8%) catheters other than the 4-mm tip catheter were used, mainly irrigated tip catheters (n=179; 47.6%), the remainder being cryoablation (n=8; 2.1%) and 8-mm tip (n=4; 1.06%) catheters.
Macroreentrant Atrial Tachycardia/Atypical Atrial FlutterThis ablation target was treated in 54 centers (65.9%) in a total of 313 procedures (mean, 5.61 procedures per center; range, 1-18), 151 fewer than in 2014. The procedure was successful in 74.4% of the cases (n=233). Six complications were reported (1.9%): 3 femoral vascular complications, 1 case of pericardial effusion, 1 atrioventricular block, and 1 stroke.
The origin of the tachycardia was notified in 293 procedures: right atrium was identified in 127 cases and left atrium in 166, with success rates of 84.3% and 74.7%, respectively. In 85% of the cases, devices other than the 4-mm tip catheter were used. Irrigated tip catheters were used in 251 cases (80.2%) and 8-mm tip catheters in 15 (5.8%).
Atrial FibrillationA total of 2640 AF ablation procedures were carried out in 2378 patients in 60 (73%) of the participating centers (range, 1-170 per site). This activity represented an increase of 142 ablations (5.7%) compared with the 2014 registry (which, in turn, had shown a 13.5% increase with respect to 2013), with a mean of 44 procedures per center. Nine laboratories performed less than 10 procedures, and 23 less than 25. Twenty-two centers carried out more than 50 procedures and, in this group, only 6 performed more than 100 procedures. A total of 65.3% were for paroxysmal AF and 34.7% were for persistent AF. Of the ablation procedures for persistent AF, 116 were for long-standing AF.
The treatment approach used was reported in 2498 (94.6%) of the procedures: electrical disconnection at the pulmonary vein ostium in 11.4% of the cases, circumferential isolation with the aim of disconnection in 86.7%, and circumferential isolation to reduce electrical connections in the remaining 1.9%. The right atrium was treated in 58 (2.3%) of the procedures.
Most of the teams (69.8%) used irrigated-tip catheters. The proportion of procedures performed with cryoballoon (n=674; 25.9%) remained steady with respect to the 2014 registry (27%). Ablation of AF using other single-shot systems continued to be negligible: laser (1.3%), PVAC (pulmonary vein ablation catheter, 1.6%), and nMARQ (0.6%). Again, there was a slight decrease in the use of steerable sheaths, used in a total of 306 cases (11.6% of all the procedures vs 14.3% in the 2014 registry). These sheaths were used in 15 centers (25%).
A total of 114 complications (4.3%), similar to the percentage in 2014, were recorded as follows: pericardial effusion/cardiac tamponade (n=44; 1.7%), vascular access (n=43; 1.7%), stroke (n=3; 0.1%), phrenic nerve palsy (n=7; 0.3%), myocardial infarction/angina (n=5; 0.2%), pulmonary vein stenosis (n=1; 0.04%), and heart failure (n=1; 0.04%). There were 6 cases of air embolism (all resolved during the procedure, with coronary angiography in 1 case), 1 case of coronary spasm (cryoablation in left superior pulmonary vein), 2 cases of catheter entrapment in the mitral valve apparatus, which did not require surgery but resulted in mild and moderate mitral regurgitation, respectively, and hemoperitoneum in 1 of the cases. There was 1 death (0.03%), in a patient with pericardial effusion/tamponade (although the cause of death was not specified).
Idiopathic Ventricular TachycardiaAblation of IVT was carried out in 429 procedures in 65 centers (79%) (mean, 6.6 procedures per center; range, 1-19). In all, 338 procedures were successful (78.8%), a much lower proportion than that reported in the 2014 registry (95.8%). There were 14 complications (3.3%): 4 vascular complications (0.9%), 7 cases of pericardial effusion/cardiac tamponade (1.6%), 2 strokes (0.5%), and 1 case of non—ST-segment elevation acute coronary syndrome (0.2%).
The type of ventricular tachycardia treated was specified in 410 procedures (95%): right ventricular outflow tract in 228; left ventricular outflow tract in 95; fascicular tachycardia in 43, and ventricular tachycardia other than the above (reported as “other locations”) in 44 procedures. Ablation was successful in 82.9%, 67.4%, 86%, and 72.7% of these procedures, respectively. The site of origin of the ventricular tachycardia was aortic root in 25 cases, pulmonary artery in 23, and the interior of a coronary vein in 8.
Catheters other than the 4-mm tip device were used in 74.1% of the cases. An irrigated tip catheter was used in 316 cases (73.7%), an 8-mm tip catheter in 2 (0.5%), and a cryoablation catheter in 1 (0.2%).
Ventricular Tachycardia in Ischemic CardiomyopathyIn all, VT-ICM was treated in 56 centers (68.3%) performing 474 ablation procedures (8.6 per center; range, 1-40).
The type of ablation performed was specified in 95.6% of the cases: a “standard” approach was used in 103 cases and a substrate approach in 350. The overall success rate was 80% (similar to the rate of 81.2% reported in 2014). The success rate was 74.8% with the standard approach and 90.3% with the substrate approach. The access route was reported in 89.2% of the cases: 335 endocardial, 37 epicardial, and 51 endocardial and epicardial, indicating a further increase in the percentage involving epicardial access over that recorded in previous years (26.3% vs 15.7% in 2014 and 11.8% in 2013). The complications (n=36; 7.6%) involved vascular access (n=10; 2.1%), pericardial effusion/cardiac tamponade (n=18; 3.8%), ischemia/myocardial infarction (n=1; 0.2%), heart failure (n=6; 1.3%), and atrioventricular block (n=1; 0.2%). Six patients (1.3%) died after the procedure and the cause was specified in 3: electromechanical dissociation that did not respond to resuscitation maneuvers, cardiogenic shock, and perforation of an aortic cusp requiring emergency sternotomy.
An irrigated-tip ablation catheter was used in most of the cases of VT-ICM ablation (95.6%). Steerable sheaths were used in 175 cases (36.7%).
Ventricular Tachycardia in Nonischemic CardiomyopathyA total of 253 VT-NICM ablation procedures were performed in 42 laboratories (51.2%) (6.2 procedures per center; range 1-25). The type of ventricular tachycardia was specified in 231 cases. There were 34 interventions for arrhythmogenic cardiomyopathy (success rate, 73.5%), 12 for bundle branch reentrant ventricular tachycardia (success rate, 91.7%), 108 for nonischemic dilated cardiomyopathy (success rate, 69.4%), 50 for nonsustained ventricular tachycardia (success rate, 78%), and 31 for conditions reported as being of “another type” (success rate, 61.3%).
There were 12 complications (4.7%): 2 episodes of heart failure (0.8%), 2 vascular complications (0.8%), 7 cases of pericardial effusion/cardiac tamponade (2.8%), and 1 case of arrhythmic storm (0.4%), leading to death due to electromechanical dissociation in a patient with dilated cardiomyopathy.
A catheter other than the 4-mm tip model was used in 89.3% of the cases. An irrigated-tip catheter was used in 220 (87%), an 8-mm tip catheter in 5 (2%), and a cryoablation catheter in 1 (0.4%).
DISCUSSIONAlthough the present registry shows a slight decrease in the number of participating centers compared with 2014, the difference is minor (from 85 to 82). Thus, it may still be representative of the reality of the situation of this procedure in Spain. While it is difficult to establish the reasons, it could be due to a decrease in voluntary data reporting rather than to an actual decline in the number of Spanish centers performing ablations. The total number of ablations was nearly the same as in 2014, and the number of ablations per center increased slightly, exceeding the mark of 155 for the mean and 138 for the median. This datum is probably skewed due to the low productivity of some private centers; thus, the activity in the public centers may actually be higher.
The data reported for human and material resources confirm a sustained or even somewhat higher investment compared with previous registries, possibly related to growing health care needs. In this respect, it is clear that very few centers are not equipped with a nonfluoroscopic navigation system and that the number of laboratories equipped with digital radiography, intracardiac echocardiography, and cryoablation is increasing. The use of magnetic and robotic navigation systems has remained unchanged over the past few years, with an almost negligible presence, confirming the low penetration of these systems in Spain.
The percentages of ablations involving the different targets were along the lines of previous years, with some noteworthy exceptions. For the first time, the treatment of CTI surpassed–although by a small number of procedures–that of AVNRT, becoming the most frequently performed ablation procedure. Compared with 2014, there were considerable decreasesin the treatment of IVT and atrial tachycardia in general, and the decline in MAT was notable. We are aware of the slight but progressive decrease in ablation of accessory pathways since the registry was introduced in 2002. In contrast, the number of AF ablation procedures continued to grow, and AF became the third leading ablation target. Although it was carried out in 3 out of 4 electrophysiology laboratories, the mean number of procedures continued to be low, and less than half of the centers performing AF ablation carried out more than 50 procedures in 2015. Two thirds of the procedures were carried out to treat paroxysmal AF. The complications rate was similar to that reported in previous registries and there was 1 death. Radiofrequency ablation and irrigated ablation continued to predominate over cryoablation in the same proportion as in previous years, and the use of other single-shot devices was practically negligible. The success rate in FAT remained steady, and that of MAT decreased, with results more in accordance with the difficulty of this type of procedure.
Nearly 1 of 10 ablation procedures performed in Spain was carried out to treat ventricular tachycardia. The total number was very similar to that of 2014, so it remained steady. However, in the treatment of IVT, both the number of ablation procedures and the success achieved declined. This decrease in IVT ablation was offset by the treatment of VT-ICM, which rose by 4% compared with 2014, whereas ablation of VT-NICM remained the same (2%). Three of every 4 procedures to treat VT-ICM involved substrate ablation. There was also a considerable increase in the use of the epicardial approach.
Eleven periprocedural deaths (0.08%) were recorded, 3 more than in 2014. Although 8 of them occurred in patients who underwent high-risk substrate ablation, that was not the case in 3 patients. As in 2014, there was another deathof a patient with AVNRT, as well as the deaths of 2 patients who underwent accessory pathway ablation. The analysis of the causes is highly complex and goes beyond the scope of this article, but these deaths should alert us to the risk of mortality in any ablation procedure.
CONCLUSIONSYear after year, the Spanish Catheter Ablation Registry provides one of the largest samples of ablation procedures in the international literature. For the first time, there was no increase in the number of procedures reported. There was the same proportion of complex arrhythmias and arrhythmogenic substrates and the success rates remained high and the percentages of major complications and deaths were low. There were no noteworthy changes in the human and technical resources compared with previous years.
CONFLICTS OF INTERESTNone declared.
Once again, the coordinators of the registry would like to thank all the participants who voluntarily and disinterestedly submitted their data to the 2015 Spanish Catheter Ablation Registry. We extend special thanks to Cristina Plaza for her excellent and untiring administrative work.
| Miguel Ángel Arias-Palomares, Julio Martí-Almor, Manuel Doblado-Calatrava, Javier Jiménez-Díaz, José Manuel Rubio-Campal, Alberto Barrera-Cordero, Pilar Cabanas-Grandío, Xavier Sabaté-de la Cruz, Jordi Punti-Sala, Juan Carlos Rodríguez-Pérez, Rafael Romero-Garrido, José Luis Martínez-Sande, Eduardo Caballero-Dorta, Arcadio García-Alberola, Ignacio Gil- Ortega, Axel Sarrias-Mercé, Roberto Matía-Francés, Javier Moreno-Planas, Eduardo Arana-Rueda, Javier Jiménez-Candil, Adolfo Fontenla-Cerezuela, Concepción Alonso-Martín, Sonia Ibars-Campaña, Enrique Rodríguez-Font, Joaquín Osca-Asensi, Antonio Asso-Abadía, Miguel Álvarez-López, José Luis Ibáñez-Criado, Alicia Ibáñez-Criado, María Carmen Expósito-Pineda, Bieito Campos-García, Juan Miguel Sánchez-Gómez, Ricardo Salgado-Aranda, Andrés Bodegas-Cañas, Gonzalo Rodrigo-Trallero, María Luisa Fidalgo-Andrés, Luis Mainar-Latorre, Lucas Cano-Calabria, Marta Ortega-Molina, Rosa Porro-Fernández, Rafael Peinado-Peinado, Juan Manuel Fernández-Gómez, Ángel Moya-i-Mitjans, Mar González-Vasserot, Pablo Moriña, Agustín Pastor-Fuentes, Nicasio Pérez-Castellano, José María Guerra-Ramos, Carlos Gómez-Navarro, Jerónimo Rubio- Sanz, Jordi Pérez-Rodón, Antonio Peláez-González, Santiago Magnani, José Moreno-Arribas, Alfonso Macías-Gallego, Antonio Linde-Estrella, Elena Esteban-Paul, Ernesto Díaz-Infante, Víctor Castro-Urda, Felipe Rodríguez-Entem, Dolores García-Medina, Ignacio García-Bolao, José Manuel Rubín-López, Ángel Grande-Ruiz, Ivo Roca-Luque, Luis Borrego-Bernabé, Eduard Guasch-i-Casany, Rocío Cózar-León, Rafael Romero-Garrido, Georgia Sarquella-Brugada, María Fe Arcocha-Torres, Ángel Martínez-Brotons, Benito Herreros-Guilarte, Ángel Arenal-Maíz, Nuria Rivas-Gándara, Javier Pindado-Rodríguez, Javier Martínez-Basterra and Jesús Almendral-Garrote. |
| Andalusia | |
| Almería | Hospital Mediterráneo (C. Gómez Navarro) |
| Cádiz | Hospital Puerta del Mar (L. Cano Calabria) |
| Granada | Hospital Inmaculada, Complejo Hospitalario Universitario de Granada (M. Álvarez López) |
| Huelva | Hospital Juan Ramón Jiménez, Hospital Costa de la Luz (P. Moriña) |
| Jaén | Complejo Hospitalario de Jaén (A. Linde Estrella) |
| Málaga | Hospital Quirón Málaga (M. Álvarez López); Hospital Virgen de la Victoria (A. Barrera) |
| Sevilla | Hospital Nisa Aljarafe (E. Díaz Infante); Hospital Virgen Macarena (R. Cózar); Hospital Infanta Luisa Sevilla (J.M. Fernández Gómez); Hospital Virgen del Rocío (E. Arana Rueda); Hospital de Valme (D. García Medina) |
| Aragon | |
| Zaragoza | Hospital Miguel Servet; Hospital Quirón Zaragoza (A. Asso); Hospital Lozano Blesa (G. Rodrigo Trallero) |
| Principality of Asturias | Hospital Central de Asturias (J.M. Rubín López); Hospital de Cabueñes (M. González Vasserot) |
| Balearic Islands | Hospital Son Llàtzer (S. Magnani); Hospital Son Espases (M.C. Expósito Pineda); Red Asistencial Juaneda (I. Roca Luque) |
| Canary Islands | |
| Las Palmas | Hospital Universitario de Gran Canaria Dr. Negrín (E. Caballero Dorta); Hospital Santa Catalina (J.C. Rodríguez Pérez) |
| Santa Cruz de Tenerife | Hospital San Juan de Dios (R. Romero); Hospital Nuestra Señora de la Candelaria (R. Romero) |
| Cantabria | Hospital Marqués de Valdecilla (F. Rodríguez Entem) |
| Castile-La Mancha | |
| Toledo | Hospital Virgen de La Salud (M.A. Arias Palomares); Hospital Nuestra Señora del Prado (A. Macías) |
| Ciudad Real | Hospital General Universitario de Ciudad Real (J. Jiménez Díaz) |
| Castile and León | |
| Burgos | Hospital Universitario de Burgos (R. Salgado) |
| León | Hospital de León (M.L. Fidalgo) |
| Salamanca | Hospital Universitario de Salamanca (J. Jiménez Candil) |
| Valladolid | Hospital Clínico de Valladolid (J. Rubio Sanz); Hospital Río Hortega (B. Herreros) |
| Catalonia | |
| Barcelona | Hospital del Mar (J. Martí Almor); Hospital Vall d’Hebron (Nuria Rivas); Hospital Sant Joan de Déu (G. Sarquella); Hospital Clínic de Barcelona (E. Guasch); Hospital Quirón Dexeus (J. Pérez Rodón); Clínica Corachán, Barcelona (J.M. Guerra Ramos); Clínica Sagrada Familia (A. Moya); Clínica Teknon (E. Rodríguez Font); Hospital Mútua de Terrassa (S. Ibars Campaña); Hospital de la Santa Creu i Sant Pau (C. Alonso Martín); Hospital Germans Trias i Pujol (A. Sarrias); Corporació Sanitaria Parc Taulí (J. Punti); Hospital Universitario de Bellvitge (X. Sabaté) |
| Lleida | Hospital Arnau de Vilanova (B. Campos) |
| Valencian Community | |
| Alicante | Hospital de San Juan de Alicante (J. Moreno Arribas); Hospital General Universitario de Alicante (J.L. Ibáñez Criado); CardioRitmo Levante (A. Ibáñez Criado) |
| Castellón | Hospital General Universitario de Castellón (J.M. Sánchez) |
| Valencia | Hospital Clínico de Valencia (A. Martínez Brotons); Hospital La Fe (J. Osca); Hospital Dr. Peset (A. Peláez González); Hospital de Manises (L. Mainar Latorre) |
| Extremadura | |
| Badajoz | Hospital Infanta Cristina (M. Doblado Calatrava) |
| Cáceres | Hospital San Pedro de Alcántara (R. Porro) |
| Galicia | |
| A Coruña | Hospital Clínico Universitario de Santiago (J.L. Martínez Sande) |
| Vigo | Complejo Hospitalario Universitario de Vigo (P. Cabanas Grandío) |
| Community of Madrid | Grupo HM Hospitales-Hospital de Madrid (J. Almendral); Hospital Gregorio Marañón (A. Arenal); Hospital Puerta de Hierro (V. Castro Urda); Fundación Hospital Alcorcón (E. Esteban Paul); Hospital Severo Ochoa (A. Grande); Hospital de Getafe (A. Pastor); Hospital Clínico San Carlos (N. Pérez Castellano); Hospital La Paz (R. Peinado); Hospital Infantil La Paz (M. Ortega Molina); Fundación Jiménez Díaz (J.M. Rubio); Hospital 12 de Octubre (A. Fontenla); Hospital Ramón y Cajal (J. Moreno); Sanitas La Moraleja (R. Matía); Hospital de Torrejón (L. Borrego Bernabé) |
| Region of Murcia | Hospital Virgen de la Arrixaca (A. García Alberola); Hospital Universitario Santa Lucía (I. Gil Ortega) |
| Chartered Community of Navarre | Hospital de Navarra (J. Martínez Basterra); Clínica Universidad de Navarra (I. García Bolao) |
| Basque Country | |
| Álava | Hospital Txagorritxu (J. Pindado) |
| Vizcaya | Hospital de Basurto (M.F. Arcocha); Hospital de Cruces (A. Bodegas) |