The present report updates the main characteristics and outcomes of heart transplants in Spain to 2020.
MethodsWe describe the main features of recipients, donors, surgical procedure, and immunosuppression in 2020. We also analyze the temporal trends of these characteristics and outcomes (survival) for the period 2011 to 2019.
ResultsIn 2020, 278 heart transplants were performed (7.3% decrease vs 2019). The findings in 2020 confirmed previous observations of an increase in pretransplant sternotomy, a slight decrease in urgent transplants carried out with ventricular assist devices, a slight decrease in donor age, an increase in the use of allografts with previous arrest, and a decrease in ischemia time. Survival continued to improve in recent triennia, reaching 82.0% at 1 year in the period 2017 to 2019.
ConclusionsThe slight decrease in the number of heart transplants performed in 2020 in Spain, most likely due to the SARS-CoV-2 pandemic, did not change the main characteristics of the procedure. No change was observed in the tendency to improved survival.
Keywords
The Spanish Heart Transplant Registry (Registro Español de Trasplante Cardiaco) has published an annual report every year since 1991 on heart transplant activity and outcomes in Spain. This document includes all heart transplants performed in Spain since transplant activity began here in 1984. The report is hugely valuable for detecting problems and opportunities in transplant patient care and has established itself as a driver of clinical research.1–3
The present article provides an update on the data from previous years, including the procedures performed in 2020, paying particular attention to the results obtained in the last decade.
METHODSPatients and proceduresData related to the characteristics of recipients, donors, surgical procedures, immunosuppression, and outcomes of all procedures are collected in a pre-established, Excel-based electronic database that can be accessed online. Updating this registry at least once per year is mandatory for participating centers. The Spanish Heart Transplant Registry is anonymized for patients, has been approved by an ethics committee, and is registered by the Spanish Society of Cardiology with the Spanish Ministry of Health as outlined in the Organic Law on Data Protection. The database is the property of the Spanish Society of Cardiology. Database maintenance, quality assurance, and statistical analysis are performed by an external contract research organization. The only significant change to the current database is related to the cutoff age for defining pediatric transplants, which is now 18 years, in line with the change made by the Spanish National Transplant Organization and is aimed at standardizing our data with those of international registries.
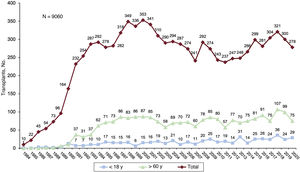
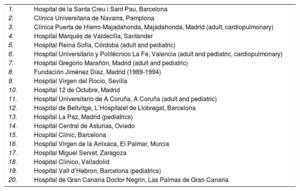
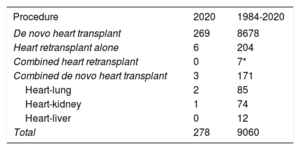
Currently, 19 centers have an active heart transplant program (table 1). Of these, 2 perform pediatric transplants alone (which is also performed in 4 other centers with an adult program) and 2 centers are equipped to perform cardiopulmonary transplants. The types of transplants performed in 2020 and in the entire series are summarized in table 2. With 278 transplants performed in 2020 (10.4% in recipients younger than 18 years and 26.9% in those older than 60 years), the Spanish Heart Transplant Registry includes 9060 procedures (figure 1). The outcomes from 2020 are compared with those from the previous decade segmented into 3-year periods (2011-2013, 2014-2016, and 2017-2019). The changes over time in the percentages of urgent transplants, the type of pretransplant circulatory support, and donor age were analyzed by year.
Centers participating in the Spanish Heart Transplant Registry from 1984 to 2020 (by order of first transplant performed)
| 1. | Hospital de la Santa Creu i Sant Pau, Barcelona |
| 2. | Clínica Universitaria de Navarra, Pamplona |
| 3. | Clínica Puerta de Hierro-Majadahonda, Majadahonda, Madrid (adult, cardiopulmonary) |
| 4. | Hospital Marqués de Valdecilla, Santander |
| 5. | Hospital Reina Sofía, Córdoba (adult and pediatric) |
| 6. | Hospital Universitario y Politécnico La Fe, Valencia (adult and pediatric, cardiopulmonary) |
| 7. | Hospital Gregorio Marañón, Madrid (adult and pediatric) |
| 8. | Fundación Jiménez Díaz, Madrid (1989-1994) |
| 9. | Hospital Virgen del Rocío, Sevilla |
| 10. | Hospital 12 de Octubre, Madrid |
| 11. | Hospital Universitario de A Coruña, A Coruña (adult and pediatric) |
| 12. | Hospital de Bellvitge, L’Hospitalet de Llobregat, Barcelona |
| 13. | Hospital La Paz, Madrid (pediatrics) |
| 14. | Hospital Central de Asturias, Oviedo |
| 15. | Hospital Clínic, Barcelona |
| 16. | Hospital Virgen de la Arrixaca, El Palmar, Murcia |
| 17. | Hospital Miguel Servet, Zaragoza |
| 18. | Hospital Clínico, Valladolid |
| 19. | Hospital Vall d’Hebron, Barcelona (pediatrics) |
| 20. | Hospital de Gran Canaria Doctor Negrín, Las Palmas de Gran Canaria |
Spanish Heart Transplant Registry (1984-2020). Type of procedure
| Procedure | 2020 | 1984-2020 |
|---|---|---|
| De novo heart transplant | 269 | 8678 |
| Heart retransplant alone | 6 | 204 |
| Combined heart retransplant | 0 | 7* |
| Combined de novo heart transplant | 3 | 171 |
| Heart-lung | 2 | 85 |
| Heart-kidney | 1 | 74 |
| Heart-liver | 0 | 12 |
| Total | 278 | 9060 |
Continuous variables are expressed as mean±standard deviation, whereas categorical variables are expressed as percentages. Differences among time periods were analyzed using a nonparametric test for temporal trends (Kendall τ) for categorical variables and ANOVA (analysis of variance) with polynomial fit for continuous variables. Survival curves were calculated using the Kaplan-Meier test and were compared using a log-rank test. P <.05 was considered statistically significant.
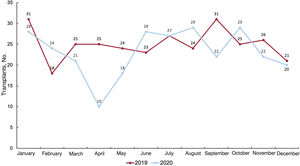
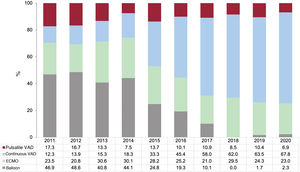
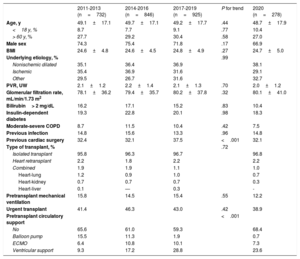
RESULTSRecipient characteristicsIn total, 278 transplants were performed in 2020, 7.3% less than in the previous year. The fall in the number of transplants was largely due to a decrease in April (figure 2). Recipient characteristics in 2020 and in the previous decade are summarized in table 3. At the time of transplantation, 10.2% of recipients were younger than 18 years and 26.9% were older than 60 years. The overall mean age was 48.7 years, similar to that of the previous decade; 33.1% were women. Almost one-third of the procedures were performed for heart diseases with etiologies other than ischemic or nonischemic dilated cardiomyopathy and in patients with previous cardiac surgery. In total, 39% of procedures were urgent (table 3); these procedures were largely performed with circulatory support via ventricular assist devices (figure 3). The percentage of urgent transplants has returned to the levels recorded at the start of the decade (about 38%), after a period (2013 and 2018) when it almost reached 50% (figure 4). In the last decade, there were no significant changes in the main characteristics of recipients, except an increase in the percentage of patients with previous cardiac surgery and a change in the type of pretransplant circulatory support, with the almost complete disappearance of the balloon pump and an increase in ventricular assist devices, mainly continuous flow (figure 3).
Recipient characteristics in the Spanish Heart Transplant Registry (2011-2020)
| 2011-2013 (n=732) | 2014-2016 (n=846) | 2017-2019 (n=925) | P for trend | 2020 (n=278) | |
|---|---|---|---|---|---|
| Age, y | 49.1±17.1 | 49.7±17.1 | 49.2±17.7 | .44 | 48.7±17.9 |
| <18 y, % | 8.7 | 7.7 | 9.1 | .77 | 10.4 |
| > 60 y, % | 27.7 | 29.2 | 30.4 | .58 | 27.0 |
| Male sex | 74.3 | 75.4 | 71.8 | .17 | 66.9 |
| BMI | 24.6±4.8 | 24.6±4.5 | 24.8±4.9 | .27 | 24.7±5.0 |
| Underlying etiology, % | .99 | ||||
| Nonischemic dilated | 35.1 | 36.4 | 36.9 | 38.1 | |
| Ischemic | 35.4 | 36.9 | 31.6 | 29.1 | |
| Other | 29.5 | 26.7 | 31.6 | 32.7 | |
| PVR, UW | 2.1±1.2 | 2.2±1.4 | 2.1±1.3 | .70 | 2.0±1.2 |
| Glomerular filtration rate, mL/min/1.73 m2 | 78.1±36.2 | 79.4±35.7 | 80.2±37.8 | .32 | 80.1±41.0 |
| Bilirubin> 2 mg/dL | 16.2 | 17.1 | 15.2 | .83 | 10.4 |
| Insulin-dependent diabetes | 19.3 | 22.8 | 20.1 | .98 | 18.3 |
| Moderate-severe COPD | 8.7 | 11.5 | 10.4 | .42 | 7.5 |
| Previous infection | 14.8 | 15.6 | 13.3 | .96 | 14.8 |
| Previous cardiac surgery | 32.4 | 32.1 | 37.5 | <.001 | 32.1 |
| Type of transplant, % | .72 | ||||
| Isolated transplant | 95.8 | 96.3 | 96.7 | 96.8 | |
| Heart retransplant | 2.2 | 1.8 | 2.2 | 2.2 | |
| Combined | 1.9 | 1.9 | 1.1 | 1.0 | |
| Heart-lung | 1.2 | 0.9 | 1.0 | 0.7 | |
| Heart-kidney | 0.7 | 0.7 | 0.7 | 0.3 | |
| Heart-liver | 0.1 | — | 0.3 | - | |
| Pretransplant mechanical ventilation | 15.8 | 14.5 | 15.4 | .55 | 12.2 |
| Urgent transplant | 41.4 | 46.3 | 43.0 | .42 | 38.9 |
| Pretransplant circulatory support | <.001 | ||||
| No | 65.6 | 61.0 | 59.3 | 68.4 | |
| Balloon pump | 15.5 | 11.3 | 1.9 | 0.7 | |
| ECMO | 6.4 | 10.8 | 10.1 | 7.3 | |
| Ventricular support | 9.3 | 17.2 | 28.8 | 23.6 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ECMO, extracorporeal membrane oxygenation; PVR, pulmonary vascular resistance.
Values are expressed as percentage or mean ± standard deviation.
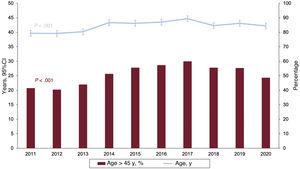
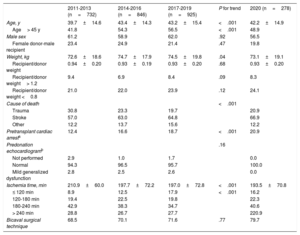
The characteristics of the donors and surgical procedures are summarized in table 4. Once again, a high percentage of transplants involved donors older than 45 years, which represented almost half of the patients. Nonetheless, after a peak in 2017, the subsequent years showed a slight decreasing tendency in the percentage of older donors (figure 5). As in previous years, the trends show a high percentage of transplants involving donors who had a preprocedural cardiac arrest or who died of stroke.
Donor characteristics and procedure times in the Spanish Heart Transplant Registry (2011-2020)
| 2011-2013 (n=732) | 2014-2016 (n=846) | 2017-2019 (n=925) | P for trend | 2020 (n=278) | |
|---|---|---|---|---|---|
| Age, y | 39.7±14.6 | 43.4±14.3 | 43.2±15.4 | <.001 | 42.2±14.9 |
| Age> 45 y | 41.8 | 54.3 | 56.5 | <.001 | 48.9 |
| Male sex | 61.2 | 58.9 | 62.0 | .92 | 56.5 |
| Female donor-male recipient | 23.4 | 24.9 | 21.4 | .47 | 19.8 |
| Weight, kg | 72.6±18.6 | 74.7±17.9 | 74.5±19.8 | .04 | 73.1±19.1 |
| Recipient/donor weight | 0.94±0.20 | 0.93±0.19 | 0.93±0.20 | .68 | 0.93±0.20 |
| Recipient/donor weight> 1.2 | 9.4 | 6.9 | 8.4 | .09 | 8.3 |
| Recipient/donor weight <0.8 | 21.0 | 22.0 | 23.9 | .12 | 24.1 |
| Cause of death | <.001 | ||||
| Trauma | 30.8 | 23.3 | 19.7 | 20.9 | |
| Stroke | 57.0 | 63.0 | 64.8 | 66.9 | |
| Other | 12.2 | 13.7 | 15.6 | 12.2 | |
| Pretransplant cardiac arresta | 12.4 | 16.6 | 18.7 | <.001 | 20.9 |
| Predonation echocardiogramb | .16 | ||||
| Not performed | 2.9 | 1.0 | 1.7 | 0.0 | |
| Normal | 94.3 | 96.5 | 95.7 | 100.0 | |
| Mild generalized dysfunction | 2.8 | 2.5 | 2.6 | 0.0 | |
| Ischemia time, min | 210.9±60.0 | 197.7±72.2 | 197.0±72.8 | <.001 | 193.5±70.8 |
| ≤ 120 min | 8.9 | 12.5 | 17.9 | <.001 | 16.2 |
| 120-180 min | 19.4 | 22.5 | 19.8 | 22.3 | |
| 180-240 min | 42.9 | 38.3 | 34.7 | 40.6 | |
| > 240 min | 28.8 | 26.7 | 27.7 | 220.9 | |
| Bicaval surgical technique | 68.5 | 70.1 | 71.6 | .77 | 79.7 |
Values are expressed as percentage or mean ± standard deviation.
The mean ischemia time has tended to fall in the last decade due to an increase in procedures with short ischemia times (≤ 120minutes) and a decrease in interventions with moderately long times (180-240minutes). In 2020, 4 of every 5 transplants were performed with a bicaval technique.
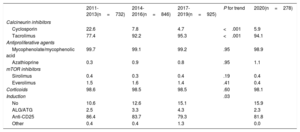
ImmunosuppressionInduction immunosuppression in 2020 was in line with that observed in the previous 3-year period (2017-2019; table 5). The use of cyclosporin was very low (about 5%) and almost entirely limited to patients with adverse reactions to tacrolimus. Likewise, the use of azathioprine was barely recorded in the last decade. More than 80% of patients received antibody-based pretransplant induction therapy, mainly basiliximab.
Induction immunosuppressive in the Spanish Heart Transplant Registry (2011-2020)
| 2011-2013(n=732) | 2014-2016(n=846) | 2017-2019(n=925) | P for trend | 2020(n=278) | |
|---|---|---|---|---|---|
| Calcineurin inhibitors | |||||
| Cyclosporin | 22.6 | 7.8 | 4.7 | <.001 | 5.9 |
| Tacrolimus | 77.4 | 92.2 | 95.3 | <.001 | 94.1 |
| Antiproliferative agents | |||||
| Mycophenolate/mycophenolic acid | 99.7 | 99.1 | 99.2 | .95 | 98.9 |
| Azathioprine | 0.3 | 0.9 | 0.8 | .95 | 1.1 |
| mTOR inhibitors | |||||
| Sirolimus | 0.4 | 0.3 | 0.4 | .19 | 0.4 |
| Everolimus | 1.5 | 1.6 | 1.4 | .41 | 0.4 |
| Corticoids | 98.6 | 98.5 | 98.5 | .60 | 98.1 |
| Induction | .03 | ||||
| No | 10.6 | 12.6 | 15.1 | 15.9 | |
| ALG/ATG | 2.5 | 3.3 | 4.3 | 2.3 | |
| Anti-CD25 | 86.4 | 83.7 | 79.3 | 81.8 | |
| Other | 0.4 | 0.4 | 1.3 | 0.0 | |
ALG, antilymphocyte globulin; anti-CD25, basiliximab, daclizumab; ATG, antithymocyte globulin.
Values are expressed as percentages.
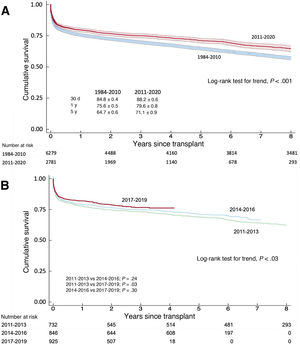
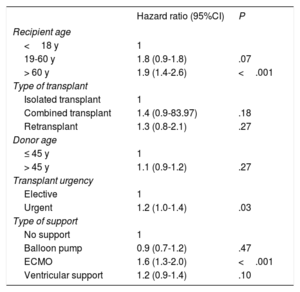
In the last decade, survival was about 80% in the first posttransplant year and was more than 70% at 5 years, which was significantly higher than that recorded in the entire previous series (figure 6A). From the last decade, the most recent 3-year period (2017-2019) showed significantly higher survival vs the 2011 to 2013 period and nonsignificantly higher survival vs the 2014 to 2016 period (figure 6B). The 1-year survival rates in the 2011 to 2013, 2014 to 2016, and 2017 to 2019 periods were 77.7%, 78.9%, and 82.0%, respectively. As in previous years, the main univariable predictors of mortality were recipient age and urgent transplant, largely due to the higher mortality of recipients who received circulatory support with extracorporeal membrane oxygenation (table 6).
Univariate analysis of survival by the baseline characteristics of the recipient, donor, and procedure (2011-2020)
| Hazard ratio (95%CI) | P | |
|---|---|---|
| Recipient age | ||
| <18 y | 1 | |
| 19-60 y | 1.8 (0.9-1.8) | .07 |
| > 60 y | 1.9 (1.4-2.6) | <.001 |
| Type of transplant | ||
| Isolated transplant | 1 | |
| Combined transplant | 1.4 (0.9-83.97) | .18 |
| Retransplant | 1.3 (0.8-2.1) | .27 |
| Donor age | ||
| ≤ 45 y | 1 | |
| > 45 y | 1.1 (0.9-1.2) | .27 |
| Transplant urgency | ||
| Elective | 1 | |
| Urgent | 1.2 (1.0-1.4) | .03 |
| Type of support | ||
| No support | 1 | |
| Balloon pump | 0.9 (0.7-1.2) | .47 |
| ECMO | 1.6 (1.3-2.0) | <.001 |
| Ventricular support | 1.2 (0.9-1.4) | .10 |
95%CI, 95% confidence interval; ECMO, extracorporeal membrane oxygenation.
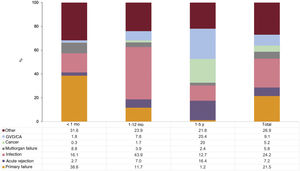
In the first 5 posttransplant years, almost half of deaths were due to primary graft failure or infection (figure 7), with primary graft failure concentrated in the first posttransplant month and infection in the remainder of the first year. Acute graft rejection was a major cause of death between the first and fifth post-transplant year (16.4%), only surpassed by combined sudden cardiac death/graft vascular disease (25.4%) and cancer (20.0%). These trends are similar to those recorded in the most recent registry analyses.
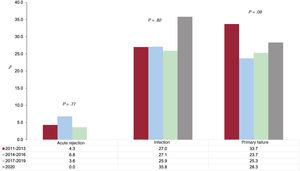
The trends in the posttransplant causes of death were analyzed only for those occurring in the first year, because complete information was available from this period for all patients (figure 8). The last decade showed a nonsignificant tendency for a decrease in primary graft failure as the cause of death, particularly since 2013, with infection and rejection maintained. Death due to rejection fell by almost half in the 2017 to 2019 period vs the previous 3-year period, although the difference was not significant due to the small number of events.
DISCUSSIONIn all settings and particularly in the health care field, 2020 has been heavily affected by the impact of the SARS-CoV-2 pandemic. Heart transplant activity has been no exception, with the number of procedures falling in 2020 vs 2019. Nonetheless, it must be highlighted that this decrease can be considered slight and, furthermore, generally limited to April and May (the latter month with less intensity), given that the activity recovered in the following months. We believe these data to be highly valuable, particularly given that transplant activity greatly depends on the activity of intensive care units, and to undoubtedly reflect the efficacy of a mature system with a very strong involvement of all of its participants.
The clinically most relevant trends in the last 10 years regarding recipient characteristics, which seem to be confirmed by the data from 2020, are related to the increased percentage of patients with previous sternotomy, a factor with prognostic implications,4 and the increased percentage of transplants performed with ventricular assist devices, which specifically require sternotomy. The latter has been accompanied by the almost complete disappearance of the balloon pump as a pretransplant circulatory support device. In addition, the percentage of transplants performed under urgent conditions has shown a biphasic behavior in the last decade, with a growing tendency until 2016 and a decrease since then, particularly since 2018. Undoubtedly, these trends have been influenced by the modification of the inclusion criteria for the urgent transplant list from the middle of 2017. A similar biphasic behavior with a less obvious explanation was observed for donor age, with a peak in 2017 and a slow progressive decrease until 2020. This finding may have a positive impact on the prognosis of our patients, particularly in the mid- and long-term.2 A variable related to donor age is cause of death, with stroke being the leading cause of death. However, this variable has exhibited a tendency for stabilization in the last two 3-year periods, which is clearly related to the variations in donor age. Finally, the last decade has shown an increase in the number of procedures performed with very short ischemia times (≤ 120minutes), due to decreases in those with moderately long times (180-240minutes), which can at least partly explain the improved survival outcomes found in our analysis.1
As in previous reports,5,6 we once again observed a significant trend for improved survival, which, in the last 3-year period analyzed, exceeded 80% in the first year. This improvement must be attributed to the slow progressive change in donor, recipient, and surgical procedure characteristics, as well as, highly probably, the familiarization of transplant teams with the increasingly complex clinical environment of contemporary heart transplantation. Nonetheless, a deeper investigation of this topic is impeded by the nature of the present report. Finally, in future reports, it will be possible to evaluate the possible impact of the SARS-CoV-2 pandemic on our results.
CONCLUSIONSHeart transplant activity fell slightly in 2020 due to the SARS-CoV-2 pandemic. Nonetheless, the clinical results continue to show a tendency for progressive improvement.
FUNDINGThe present article did not receive funding.
AUTHORS’ CONTRIBUTIONSAll authors have contributed to the data collection, have critically revised the manuscript, and have approved its publication in the current form. F. González-Vílchez was responsible for the preparation of the manuscript.
CONFLICTS OF INTERESTNone.
| Center | Collaborators |
|---|---|
| Hospital Universitario Marqués de Valdecilla, Santander | Manuel Cobo-Belaustegui, Miguel Llano-Cardenal, José Antonio Vázquez de Prada, Francisco Nistal-Herrera |
| Hospital Universitario Central de Asturias, Oviedo | José Luis Lambert-Rodríguez, Beatriz Díaz-Molina, Cristina Fidalgo-Muñiz |
| Hospital Universitario Virgen del Rocío, Sevilla | Diego Rangel-Sousa, Antonio Grande-Trillo |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Vicens Brossa-Loidi, Sonia Mirabet-Pérez, Laura López, Isabel Zegrí, Marta de Antonio |
| Hospital Clínic Universitari, Barcelona | María Ángeles Castel, Marta Farrero |
| Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat, Barcelona | Nicolás Manito, Carles Díez, Elena García-Romero, Josep Roca |
| Hospital General Universitario Gregorio Marañón, Madrid (adults) | Javier Castrodeza, Iago Sousa, Zorba Blázquez, Eduardo Zataraín, Jorge García-Carreño, Paula Navas, Miriam Juárez, Carlos Ortiz, Manuel Martínez-Sellés |
| Hospital Univesitari i Politècnic La Fe, Valencia | Mónica Cebrián, Raquel López-Viella, Ignacio Sánchez-Lázaro, Sol Martínez, Víctor Donoso, Luis Martínez |
| Hospital Universitario Reina Sofía, Córdoba | Amador López-Granados |
| Hospital Universitario Puerta de Hierro-Majadahonda, Majadahonda, Madrid | Javier Segovia-Cubero, Francisco Hernández-Pérez, Cristina Mitroi, Mercedes Rivas-Lasarte |
| Hospital Universitario 12 de Octubre, Madrid | María Dolores García-Cosío, Laura Morán-Fernández, Pedro Caravaca, Juan Carlos López-Azor |
| Complejo Hospitalario Universitario de A Coruña, A Coruña | María Jesús Paniagua-Martín, Eduardo Barge-Caballero, Gonzalo Barge-Caballero, David Couto-Mallón, José Cuenca-Castillo, José María Herrera-Noreña |
| Hospital Universitario La Paz, Madrid | Luis García-Guereta Silva, Óscar González-Fernández, Inés Ponz de Antonio, Carlos Labrandero de Lera, Álvarez González-Rocafort, Luz Polo-López |
| Hospital General Universitario Gregorio Marañón, Madrid (pediatric) | Manuela Camino-López, Nuria Gil-Villanueva |
| Hospital Clínico Universitario, Valladolid | Luis de la Fuente-Galán, Javier Tobar-Ruiz |
| Hospital Universitario Virgen de la Arrixaca, El Palmar, Murcia | Iris P. Garrido-Bravo, Domingo A. Pascual-Figal, Francisco J. Pastor-Pérez |
| Hospital Universitario Miguel Servet, Zaragoza | Teresa Blasco-Peiró, Ana Pórtoles-Ocampo, María Lasala-Alastuey |
| Clínica Universitaria, Pamplona | Gregorio Rábago-Juan-Aracil, Rebeca Manrique-Antón, Leticia Jimeno-San Martín |
| Hospital Universitario Doctor Negrín, Las Palmas de Gran Canaria | Antonio García-Quintana, María del Val Groba-Marco, Mario Galván-Ruiz |
| Hospital Universitari Vall d’Hebron, Barcelona | Ferrán Gran-Ipiña, Paola Dolader |