Keywords
INTRODUCTION
This article is the customary annual update analysis describing results of heart transplantations carried out in Spain between the first such procedure, performed in May 1984, and December 31, 2006.1-17
The registry includes all heart transplants performed by all teams at all centers in Spain and is therefore an accurate account of the status of heart transplantation in the country. The report's reliability is founded on the nationwide use of a similar database constructed on mutually agreed principles, which standardizes variables and unifies possible responses.
METHODS
Nineteen heart transplantation centers supplied data for the registry (Table 1) although only 18 actively perform transplants at present. The number of active centers in Spain had remained stable since 2001 but in 2006 one new center became operational.
In the 22 years that heart transplantation procedures have been being performed in Spain, the total number of operations has reached 5241. Figure 1 presents the distribution of the number of heart transplants per year. Of these, 94% were isolated orthotopic transplants. Table 2 shows the distribution of transplants by procedure type.
Figure 1. Number of heart transplants per year.
Survival data are analyzed in Kaplan-Meier curves and compared using the log rank test.
RESULTS
Heart Transplant Recipient Profile
In Spain, the profile of the average heart transplant recipient is that of a man aged 52 years diagnosed with ischemic heart disease or idiopathic dilated cardiomyopathy and with blood group A or O. Table 3 shows the clinical profile of isolated heart transplant recipients by age-group; retransplant recipients appear in a separate column.
Waiting List Mortality and Days-to-Transplant
In 2006, waiting list mortality was 7%. The percentage of patients excluded from transplant after placement on the waiting list was 18%. Figure 2 shows the annual percentages of waiting list patients who received a transplant, were removed from the list without receiving one, or died before receiving one.
Figure 2. Patient outcomes following inclusion in the heart transplantation waiting list.
In recent years, mean waiting list time for recipients prior to undergoing heart transplantation has been 125 days. Figure 3 shows how this has evolved over the last 14 years.
Figure 3. Year on year evolution of mean waiting list to heart transplantation days.
Cause of Death and Mean Age of Donors
Most heart transplant donors die of traumatic brain injury. In recent years, the mean age of donors has been 34 years (Figures 4 and 5).
Figure. 4. Year on year evolution of causes of heart transplant donor deaths. TBI indicates traumatic brain injury.
Figure 5. Year on year evolution of mean age of heart transplant donors.
Urgent Transplantation
In 2006, indications for urgent transplantation represented 27% of the total. This was similar to the figure for recent years (26%). Figure 6 shows the evolution of indications for urgent transplantation over the years.
Figure 6. Year on year evolution of urgent heart transplantations.
Survival
Early mortality (death at ≤30 days post-transplantation) was 14% in 2006 which represents a slight increase by comparison with recent years (12%) as Figure 7 shows.
Figure 7. Year on year percentage evolution of early deaths (at >30 days) among transplant recipients.
When survival rate data for 2006 were added to those of previous years, we obtained a 1-month actuarial survival rate of 84%, and 1-, 5-, 10-, and 15-year rates of 75%, 64%, 51%, and 35%, respectively. Average recipient survival for the entire series was 10.2 years (Figure 8). Survival by periods showed better results in the last stage with 1- and 5-year survival rates of 80%, and 75%, respectively, and with significant differences between periods (Figure 9).
Figure 8. Actuarial survival curve (Kaplan-Meier) for the entire series.
Figure 9. Survival curve by periods.
We made univariate comparisons of some variables and found significant differences between heart transplants depending on baseline etiology and degree of urgency (Figures 10 and 11). We found no differences for gender, body mass index, or age-group (Figures 12, 13, and 14).
Figure 10. Survival curves according to etiology indicating transplantation.
Figure 11. Survival curves by degree of urgency.
Figure 12. Survival curves by gender.
Figure 13. Survival curves by body mass index.
Figure 14. Survival curves by age of recipient.
Causes of Death
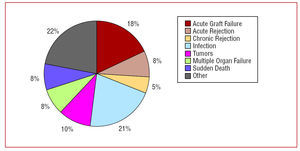
The most frequent cause of death in the entire series was infection (21%) followed by acute graft failure (18%), the combination of vascular graft disease and sudden death (13%), tumors (10%), and acute rejection (8%) (Figure 15).
Figure 15. Typical causes of mortality.
When causes of mortality are analyzed by periods, differences can be seen at ≤30 days (acute graft failure and infection), 1-12 months (infection), and >1 year (tumors and the combination of sudden death and chronic rejection). Figure 16 shows the distribution of causes of death by periods.
Figure 16. Causes of death by periods.
DISCUSSION
In Spain, with 22 years experience of heart transplantation and >5000 transplants performed, we can say that this procedure can be offered to the whole population with the certainty that levels of knowledge, control, and survival are similar to those found in other western Europe countries and around the world. Analysis of the Registry of the International Society for Heart and Lung Transplantation annual report demonstrates this clearly.18,19
An important advantage of our Registry is that it is compiled from a standardized database that only permits a previously agreed range of responses. All teams update results annually and submit figures to the Registry Coordinator who, using custom-built software, introduces the data into a common database for subsequent analysis of variables. We believe this method greatly enhances the reliability of our results and avoids errors of the kind so often found in non-standardized databases. Notwithstanding, we have obtained the support of the pharmaceutical industry to improve the database and modify its current format, increasing the number of variables (from 100 to 150), thru an audit (conducted by an independent company) of the clinical records of all the centers. Moreover, we have conducted our statistical analysis with improved professional support.
In 2006, the number of active transplantation centers in Spain increased, causing concern among most of the transplant teams because the number of optimal donors has practically remained constant (and is tending to fall) whereas the ratio of centers to transplants has increased. The fact that fewer transplant procedures are being performed leads to the under use of resources in hospitals equipped to undertake a great number of transplants and to a longer learning process needed to achieve adequate results. The only tangible benefit for patients is the convenience of being able to undergo transplantation without having to travel far from home.
In 2006, total transplants performed fell by 13 in comparison with 2005 (274 vs 287). This may be purely by chance but the evident trend towards the performance of fewer transplants is worrying. In fact, since 2000 when 353 transplants were performed, a gradual, though irregular, fall has been the trend. There is no single explanation for this reduction in the number of donors but it seems clear that incidence of death from traumatic brain injury has decreased while prolonged care of patients with multiple trauma in specialized units has improved. The scarcity of optimal donors has caused an increase in days waiting to obtain an optimal organ despite the use of older donors. However, death while on the waiting list has remained constant (7%), although here we should add in those patients removed from the list due to severe decompensations and not included again, who die having been removed from the list. According to Spain's national transplant organization this accounts for some 10% of deaths.20 Consequently, mortality among patients waiting for a heart is 17%.
The clinical profile of patients has not changed in recent years. We analyzed heart transplant recipients in 3 groups (pediatric, adult, and retransplantation) as each of these is indicated for transplant for very different reasons: pediatric patients are operated for congenital heart disease or idiopathic dilated cardiomyopathy; they have slightly higher pulmonary resistances and do not present cardiovascular risk factors. In contrast, patients undergoing retransplantation are usually indicated for vascular graft disease; they present greater organ deterioration and more risk factors. This may be a more accurate explanation for the bad prognosis of these patients than the fact that they undergo a second transplant.
Urgent heart transplantation is somewhat controversial as these operations have specific characteristics (recipients in worse clinical condition, less-than-ideal donors, longer periods of ischemia) that entail a worse prognosis than programmed transplants. In 2006, the percentage of urgent transplants increased (27% in 2006 vs 22% in 2005). This figure is slightly higher than the mean for the last 5 years (26%). The cause of these fluctuations in indication for urgent transplantation is not wholly clear, nor are the differences in geographical distribution. However, the low number of donors clearly increases the chances of urgent transplantation. Indication for urgent transplantation has been questioned given that it offers poorer results. However, the Transplant Teams are of the opinion that this option should continue to exist, in a controlled form, as it is the only therapeutic option available to the subgroup of patients with advanced heart failure and uncontrollable acute decompensation. In any event, we must remember, as European guidelines on acute heart failure recommend, that it is better to stabilize heart failure rather than indicate for urgent transplantation.21
Incidence of early mortality increased slightly in 2006 versus 2005 (14% vs 10%, respectively). This may be due to the worse profile of recipients as well as increased donor age and longer times of ischemia motivated by the increase in urgent transplants. The early period is probably the most important in improving survival, as the survival curve stabilizes after the first months post-transplantation.
Over the years, overall survival has shown a clear trend towards progressive improvement. However, logically, the number of patients added to the Registry each year represents a comparatively smaller percentage of the total. Thus, chances of finding substantial changes in 1 year are very remote and analysis of survival by periods is more illuminating.
The most frequent cause of death depends on time post-transplantation. Causes of death at ≥1 year are acute graft failure and infection and, later, tumors and chronic rejection and sudden death. It is important to note that infection seems to be gaining ground as a cause of death, whereas death due to acute rejection is less frequent. This imbalance could be due to an overuse of immunosuppressive drugs that prevent rejection but favor infection.
CONCLUSIONS
1. In recent years, the annual volume of heart transplantations has fallen and waiting list times have increased.
2. In general, (early and late) survival rate figures are similar to those published in international registry reports and have improved year on year, especially in the last 5 years.
3. We should continue to try to reduce the high incidence of acute graft failure. This would have a highly positive effect on the probability of immediate post-operative and overall survival.
4. Given that infection is a greater cause of morbidity and mortality than rejection, we should pay it more attention and make it one of the principle objectives of general studies and clinical trials of drugs.
Statistical analysis conducted with unconditional financial support from Novartis Trasplante.
Correspondence: Dr. L. Almenar-Bonet.
Avda. Primado Reig, 189-37. 46020 Valencia. España.
E-mail: lu.almenarb5@comv.es