We present the data corresponding to implantable cardioverter-defibrillator (ICD) implants in Spain in 2020.
MethodsThe data in this registry were drawn from implantation centers, which voluntarily completed a data collection sheet.
ResultsIn 2020, 7056 implant sheets were received compared with 7106 reported by Eucomed (European Confederation of Medical Suppliers Associations), indicating that data were collected from 99% of the devices implanted in Spain. Completion of the implant sheet ranged from 99.8% for the field “name of the implanting hospital” to 2.6% for the variable “referral hospital”. A total of 173 hospitals performed ICD implants and participated in the registry, which is a similar figure to that in 2019 (n=172). The total rate of registered implants was 149/million inhabitants (150 according to Eucomed), revealing a slight reduction in implants in Spain in 2020 as a result of the impact of the COVID-19 pandemic. This reduction was uneven among the autonomous communities.
ConclusionsThe Spanish Implantable Cardioverter Defibrillator Registry for 2020 shows an improvement in the rate of implants reported and a reduction in the number of ICD implants, which likely reflects the decrease in hospital activity not related to the treatment of COVID-19 infection. Similar to previous years, the total number of implants in Spain is still much lower than the average for the European Union, with an increase in the differences between Spanish autonomous communities.
Keywords
Implantable cardioverter-defibrillators (ICDs) have become the treatment of choice for preventing sudden cardiac death, and their implantation improves prognosis in patients with ventricular arrhythmias and structural heart disease or at high risk of developing these conditions.1,2 Their effectiveness is well-documented and their indications are included in clinical practice guidelines.1–3 ICDs are one of the main tools for possibly reducing sudden cardiac death. This event is one of the leading causes of death, with an incidence in Europe of 400 000 cases/y, 40% of which occur in people younger than 65 years.4
The Spanish Implantable Cardioverter-defibrillator Registry has been published annually since 2005.5–8 The current article presents data corresponding to ICD implantation in Spain in 2020, a peculiar year, in which health services have been embroiled in the fight against the COVID-19 pandemic.
METHODSThe registry is based on voluntarily submitted implantation forms. The information is entered in a database by a team comprising a technician, a Spanish Society of Cardiology (SEC) computer scientist, and a member of the Heart Rhythm Association of the SEC. Data cleaning was performed by the technician and the first author, and all authors of this article analyzed the data and are responsible for this publication. In addition, it has been possible since 2019 to submit the implantation data via a website designed by the SEC.9 In 2020, this route was used for 1714 implants, 24.3% of the total.
Population data were obtained from the Spanish National Institute of Statistics as of January 1, 2021.10 As in previous years, the data from the present registry were compared with those provided by the European Confederation of Medical Suppliers Associations (Eucomed).11
The percentages of each of the variables analyzed were calculated by taking into account the total number of implants with available information on the parameter. Only the most serious condition was included if various types of arrhythmias were recorded.
Statistical analysisResults are expressed as mean ± standard deviation or median [interquartile range], depending on the distribution of the variable. Continuous quantitative variables were analyzed using analysis of variance or the Kruskal-Wallis test, whereas qualitative variables were analyzed using the chi-square test. Linear models were used to analyze the number of implants and devices implanted per million population, the total number of implants, and the number of implants for primary prevention in each center.
RESULTSIn 2020, 7056 implantation forms were received, although 7106 procedures were reported by Eucomed (99.3% of devices implanted). This is the highest figure in the history of the registry. Completion ranged from 99.8% for the field name of implanting hospital to 2.6% for the variable referral hospital.
Implantation centersIn total, 173 hospitals participated in the registry. This number is similar to those of 2019 (n = 172) and 2018 (n = 173) but slightly lower than that of 2017 (n = 181, the highest number recorded since registry formation). Figure 1 shows the total number of implantation centers, the rate per million population, and the total number of implants per autonomous community according to the data submitted to the registry. In 2020, 22 centers implanted ≥ 100 devices, 75 between 11 and 99 devices, 49 ≤ 10, and 27 only 1.
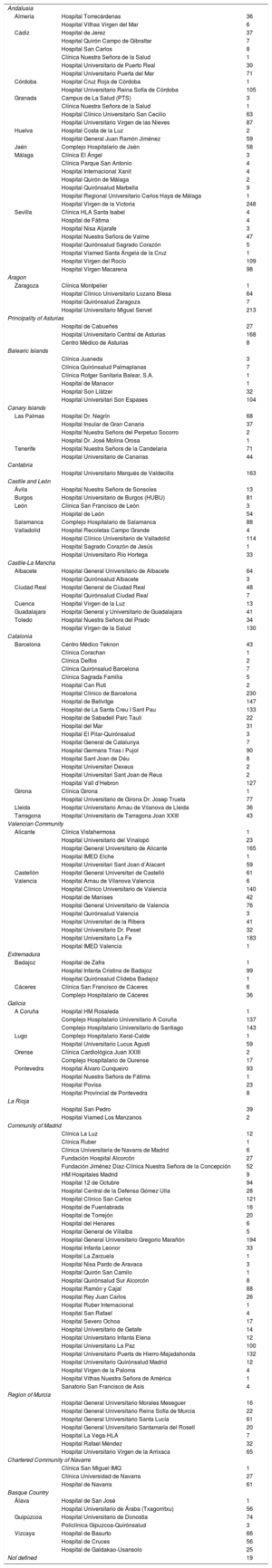
The name of the hospital performing the procedure was recorded in 99.8% of forms (table 1). Most procedures (6405, 91%) were performed in publicly-funded health centers.
Implantation by autonomous community, province, and hospital.
| Andalusia | ||
| Almería | Hospital Torrecárdenas | 36 |
| Hospital Vithas Virgen del Mar | 6 | |
| Cádiz | Hospital de Jerez | 37 |
| Hospital Quirón Campo de Gibraltar | 7 | |
| Hospital San Carlos | 8 | |
| Clínica Nuestra Señora de la Salud | 1 | |
| Hospital Universitario de Puerto Real | 30 | |
| Hospital Universitario Puerta del Mar | 71 | |
| Córdoba | Hospital Cruz Roja de Córdoba | 1 |
| Hospital Universitario Reina Sofía de Córdoba | 105 | |
| Granada | Campus de La Salud (PTS) | 3 |
| Clínica Nuestra Señora de la Salud | 1 | |
| Hospital Clínico Universitario San Cecilio | 63 | |
| Hospital Universitario Virgen de las Nieves | 87 | |
| Huelva | Hospital Costa de la Luz | 2 |
| Hospital General Juan Ramón Jiménez | 59 | |
| Jaén | Complejo Hospitalario de Jaén | 58 |
| Málaga | Clínica El Ángel | 3 |
| Clínica Parque San Antonio | 4 | |
| Hospital Internacional Xanit | 4 | |
| Hospital Quirón de Málaga | 2 | |
| Hospital Quirónsalud Marbella | 9 | |
| Hospital Regional Universitario Carlos Haya de Málaga | 1 | |
| Hospital Virgen de la Victoria | 248 | |
| Sevilla | Clínica HLA Santa Isabel | 4 |
| Hospital de Fátima | 4 | |
| Hospital Nisa Aljarafe | 3 | |
| Hospital Nuestra Señora de Valme | 47 | |
| Hospital Quirónsalud Sagrado Corazón | 5 | |
| Hospital Viamed Santa Ángela de la Cruz | 1 | |
| Hospital Virgen del Rocío | 109 | |
| Hospital Virgen Macarena | 98 | |
| Aragon | ||
| Zaragoza | Clínica Montpelier | 1 |
| Hospital Clínico Universitario Lozano Blesa | 64 | |
| Hospital Quirónsalud Zaragoza | 7 | |
| Hospital Universitario Miguel Servet | 213 | |
| Principality of Asturias | ||
| Hospital de Cabueñes | 27 | |
| Hospital Universitario Central de Asturias | 168 | |
| Centro Médico de Asturias | 8 | |
| Balearic Islands | ||
| Clínica Juaneda | 3 | |
| Clínica Quirónsalud Palmaplanas | 7 | |
| Clínica Rotger Sanitaria Balear, S.A. | 1 | |
| Hospital de Manacor | 1 | |
| Hospital Son Llàtzer | 32 | |
| Hospital Universitari Son Espases | 104 | |
| Canary Islands | ||
| Las Palmas | Hospital Dr. Negrín | 68 |
| Hospital Insular de Gran Canaria | 37 | |
| Hospital Nuestra Señora del Perpetuo Socorro | 2 | |
| Hospital Dr. José Molina Orosa | 1 | |
| Tenerife | Hospital Nuestra Señora de la Candelaria | 71 |
| Hospital Universitario de Canarias | 44 | |
| Cantabria | ||
| Hospital Universitario Marqués de Valdecilla | 163 | |
| Castile and León | ||
| Ávila | Hospital Nuestra Señora de Sonsoles | 13 |
| Burgos | Hospital Universitario de Burgos (HUBU) | 81 |
| León | Clínica San Francisco de León | 3 |
| Hospital de León | 54 | |
| Salamanca | Complejo Hospitalario de Salamanca | 88 |
| Valladolid | Hospital Recoletas Campo Grande | 4 |
| Hospital Clínico Universitario de Valladolid | 114 | |
| Hospital Sagrado Corazón de Jesús | 1 | |
| Hospital Universitario Río Hortega | 33 | |
| Castile-La Mancha | ||
| Albacete | Hospital General Universitario de Albacete | 64 |
| Hospital Quirónsalud Albacete | 3 | |
| Ciudad Real | Hospital General de Ciudad Real | 48 |
| Hospital Quirónsalud Ciudad Real | 7 | |
| Cuenca | Hospital Virgen de la Luz | 13 |
| Guadalajara | Hospital General y Universitario de Guadalajara | 41 |
| Toledo | Hospital Nuestra Señora del Prado | 34 |
| Hospital Virgen de la Salud | 130 | |
| Catalonia | ||
| Barcelona | Centro Médico Teknon | 43 |
| Clínica Corachan | 1 | |
| Clínica Delfos | 2 | |
| Clínica Quirónsalud Barcelona | 7 | |
| Clínica Sagrada Familia | 5 | |
| Hospital Can Ruti | 2 | |
| Hospital Clínico de Barcelona | 230 | |
| Hospital de Bellvitge | 147 | |
| Hospital de La Santa Creu I Sant Pau | 133 | |
| Hospital de Sabadell Parc Tauli | 22 | |
| Hospital del Mar | 31 | |
| Hospital El Pilar-Quirónsalud | 3 | |
| Hospital General de Catalunya | 7 | |
| Hospital Germans Trias i Pujol | 90 | |
| Hospital Sant Joan de Déu | 8 | |
| Hospital Universitari Dexeus | 2 | |
| Hospital Universitari Sant Joan de Reus | 2 | |
| Hospital Vall d‘Hebron | 127 | |
| Girona | Clínica Girona | 1 |
| Hospital Universitario de Girona Dr. Josep Trueta | 77 | |
| Lleida | Hospital Universitario Arnau de Vilanova de Lleida | 36 |
| Tarragona | Hospital Universitario de Tarragona Joan XXIII | 43 |
| Valencian Community | ||
| Alicante | Clínica Vistahermosa | 1 |
| Hospital Universitario del Vinalopó | 23 | |
| Hospital General Universitario de Alicante | 165 | |
| Hospital IMED Elche | 1 | |
| Hospital Universitari Sant Joan d’Alacant | 59 | |
| Castellón | Hospital General Universitari de Castelló | 61 |
| Valencia | Hospital Arnau de Vilanova Valencia | 6 |
| Hospital Clínico Universitario de Valencia | 140 | |
| Hospital de Manises | 42 | |
| Hospital General Universitario de Valencia | 76 | |
| Hospital Quirónsalud Valencia | 3 | |
| Hospital Universitari de la Ribera | 41 | |
| Hospital Universitario Dr. Peset | 32 | |
| Hospital Universitario La Fe | 183 | |
| Hospital IMED Valencia | 1 | |
| Extremadura | ||
| Badajoz | Hospital de Zafra | 1 |
| Hospital Infanta Cristina de Badajoz | 99 | |
| Hospital Quirónsalud Clideba Badajoz | 1 | |
| Cáceres | Clínica San Francisco de Cáceres | 6 |
| Complejo Hospitalario de Cáceres | 36 | |
| Galicia | ||
| A Coruña | Hospital HM Rosaleda | 1 |
| Complejo Hospitalario Universitario A Coruña | 137 | |
| Complejo Hospitalario Universitario de Santiago | 143 | |
| Lugo | Complejo Hospitalario Xeral-Calde | 1 |
| Hospital Universitario Lucus Agusti | 59 | |
| Orense | Clínica Cardiológica Juan XXIII | 2 |
| Complejo Hospitalario de Ourense | 17 | |
| Pontevedra | Hospital Álvaro Cunqueiro | 93 |
| Hospital Nuestra Señora de Fátima | 1 | |
| Hospital Povisa | 23 | |
| Hospital Provincial de Pontevedra | 8 | |
| La Rioja | ||
| Hospital San Pedro | 39 | |
| Hospital Viamed Los Manzanos | 2 | |
| Community of Madrid | ||
| Clínica La Luz | 12 | |
| Clínica Ruber | 1 | |
| Clínica Universitaria de Navarra de Madrid | 6 | |
| Fundación Hospital Alcorcón | 27 | |
| Fundación Jiménez Díaz-Clínica Nuestra Señora de la Concepción | 52 | |
| HM Hospitales Madrid | 9 | |
| Hospital 12 de Octubre | 94 | |
| Hospital Central de la Defensa Gómez Ulla | 28 | |
| Hospital Clínico San Carlos | 121 | |
| Hospital de Fuenlabrada | 16 | |
| Hospital de Torrejón | 20 | |
| Hospital del Henares | 6 | |
| Hospital General de Villalba | 5 | |
| Hospital General Universitario Gregorio Marañón | 194 | |
| Hospital Infanta Leonor | 33 | |
| Hospital La Zarzuela | 1 | |
| Hospital Nisa Pardo de Aravaca | 3 | |
| Hospital Quirón San Camilo | 1 | |
| Hospital Quirónsalud Sur Alcorcón | 8 | |
| Hospital Ramón y Cajal | 88 | |
| Hospital Rey Juan Carlos | 26 | |
| Hospital Ruber Internacional | 1 | |
| Hospital San Rafael | 4 | |
| Hospital Severo Ochoa | 17 | |
| Hospital Universitario de Getafe | 14 | |
| Hospital Universitario Infanta Elena | 12 | |
| Hospital Universitario La Paz | 100 | |
| Hospital Universitario Puerta de Hierro-Majadahonda | 132 | |
| Hospital Universitario Quirónsalud Madrid | 12 | |
| Hospital Virgen de la Paloma | 4 | |
| Hospital Vithas Nuestra Señora de América | 1 | |
| Sanatorio San Francisco de Asís | 4 | |
| Region of Murcia | ||
| Hospital General Universitario Morales Meseguer | 16 | |
| Hospital General Universitario Reina Sofía de Murcia | 22 | |
| Hospital General Universitario Santa Lucía | 61 | |
| Hospital General Universitario Santamaría del Rosell | 20 | |
| Hospital La Vega-HLA | 7 | |
| Hospital Rafael Méndez | 32 | |
| Hospital Universitario Virgen de la Arrixaca | 65 | |
| Chartered Community of Navarre | ||
| Clínica San Miguel IMQ | 1 | |
| Clínica Universidad de Navarra | 27 | |
| Hospital de Navarra | 61 | |
| Basque Country | ||
| Álava | Hospital de San José | 1 |
| Hospital Universitario de Áraba (Txagorritxu) | 56 | |
| Guipúzcoa | Hospital Universitario de Donostia | 74 |
| Policlínica Gipuzcoa-Quirónsalud | 3 | |
| Vizcaya | Hospital de Basurto | 66 |
| Hospital de Cruces | 56 | |
| Hospital de Galdakao-Usansolo | 25 | |
| Not defined | 19 | |
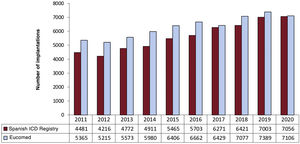
The total number of implants reported to the registry and those estimated by Eucomed in the last 10 years are shown in Figure 2. In 2020, the total number of implants (first and replacements) recorded was 7056, which suggests an increase vs 2019 (7003) and 2018 (6421). However, according to the data provided by Eucomed, the total for 2020 (7106) represents a fall in the number of ICD implants in Spain (7389 in 2019 and 7077 in 2018).
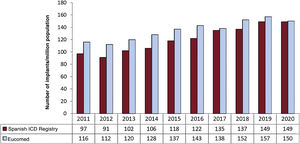
Changes in the implantation rate per million population in the last 10 years according to registry and Eucomed data are shown in Figure 3. According to Eucomed, the total implantation rate recorded was 150 implants/million population in 2020, 157 in 2019 and 152 in 2018. This figure represents a reduction vs the last 2 years and continues to be much lower than the average ICD implantation rate in Europe, which was 285/million population in 2020 (303/million in 2019).
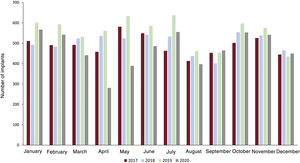
Figure 4, which shows the number of ICD implants by month between 2017 and 2020, reveals a fall in implantation in March (−17%) and particularly in April (−50%) and May (−39%) of 2020 vs the same months in the previous year. A recovery in ICD implantation activity can also be seen in the second half of 2020, although the total number of implants remained lower than that of 2019.
First implants vs replacementsThis information was available in 4405 forms (62.4% of those included in the registry). First implants comprised 3127, representing 71.0% of the total (74.3% in 2019, 71.5% in 2018, 71.4% in 2017, 66.8% in 2016, 71.8% in 2015, and 72.6% in 2014).
Age and sexThe mean age of all the patients included in the registry was 62.2 ± 13.4 (range, 5-95) years in 2020. This figure is similar to the average ages in 2019 and 2020 (62.1 ± 13.8 [4-97] years and 62.4 ± 13.5 [7-97] years, respectively). The age at first implantation was 61 ± 13.1 years (60.8 ± 13.8 in 2019). As in previous years, patients were overwhelming male: they represented 82.6% of all patients and 83.6% of first implants.
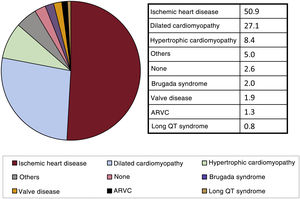
Underlying heart disease, left ventricular ejection fraction, functional class, and baseline rhythmThe most frequent underlying cardiac condition in first implant patients was ischemic (50.9%), followed by dilated cardiomyopathy (27.1%), hypertrophic cardiomyopathy (8.4%), primary conduction abnormalities (Brugada syndrome and long QT syndrome; 2.8%), valve diseases (1.9%), and arrhythmogenic right ventricular cardiomyopathy (1.3%) (Figure 5).
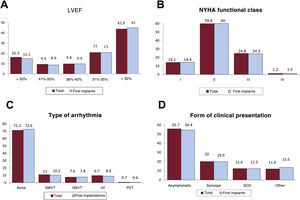
Left ventricular systolic function data were provided in 51.8% of forms. Left ventricular ejection fraction was > 50% in 16% of patients, from 41% to 50% in 9.4%, from 36% to 40% in 9.8%, from 31% to 35% in 21%, and ≤ 30% in 43.9% (Figure 6). The distribution was similar when it was grouped by first implants and replacements.
Clinical characteristics of the registry patients (total and first implants). A: left ventricular ejection fraction (LVEF). B: NYHA functional class. C: distribution of arrhythmias prompting implantation (first implants and total). D: clinical presentation of the arrhythmia in the registry patients (first implants and total). NSVT, nonsustained ventricular tachycardia; NYHA, New York Heart Association; PVT, polymorphic ventricular tachycardia; SCD, sudden cardiac death; SMVT, sustained monomorphic ventricular tachycardia; VF, ventricular fibrillation.
New York Heart Association (NYHA) functional class was recorded in 31.2% of forms. Most patients were in NYHA class II (59.8%), followed by NYHA III (24.8%), NYHA I (14.1%), and NYHA IV (1.2%). The distribution for this variable was also similar in the overall and first implantation groups (Figure 6).
With data from 52.9% of forms, the baseline cardiac rhythm was primarily sinus (78.9%), followed by atrial fibrillation (18.1%) and pacemaker rhythm (3.3%). The remaining patients had other rhythms (eg, atrial flutter and other arrhythmias).
Arrhythmias and implantationThe clinical arrhythm ia prompting device implantation was reported in 52.2% of forms. In the total group, patients with no documented clinical arrhythmia comprised 71.2%. For first implants, most patients had no documented clinical arrhythmias (72.6%), whereas 10.2% had sustained monomorphic ventricular tachycardia, 7.8% had nonsustained ventricular tachycardia, and 8.9% had ventricular fibrillation (Figure 6).
The most frequent presentation in both the total implantation group and in first implantation patients (39.3% of completed responses) was asymptomatic (in more than half of patients), followed by syncope, sudden cardiac death, and other symptoms (Figure 6).
Information on the electrophysiological studies performed before ICD implantation was provided in 40.7% of forms. These studies were performed in 379 patients (5.5%), mainly in those with ischemic heart disease or dilated cardiomyopathy and in 40.9% of patients with Brugada syndrome. Sustained monomorphic ventricular tachycardia was the most common induced arrhythmia (27.9%), followed by ventricular fibrillation (15.2%), nonsustained ventricular tachycardia (6.4%) and, to a lesser extent, other arrhythmias (4.2%). No arrhythmia was induced in 46.3% of the electrophysiological studies.
Clinical historyIn all forms submitted to the registry, 52.7% provided some data on the clinical history of the patient undergoing ICD implantation. Hypertension was present in 52.9% of patients, as well as hypercholesterolemia in 44.6%, smoking in 30.5%, diabetes mellitus in 28.1%, history of atrial fibrillation in 25.9%, renal failure in 11.3%, family history of sudden cardiac death in 8.9%, and history of stroke in 4.7%.
The QRS duration interval was reported in 40.6% of first implants (mean, 127.2ms). In 33.4% of the patients, the duration was > 140ms, and 83.0% of these patients had a resynchronization-defibrillator device (ICD-cardiac resynchronization therapy [CRT]).
IndicationsDevice indications over time are shown in table 2. These data were provided in 43.8% of forms in 2020. Ischemic heart disease was the most frequent reason for ICD implantation (50.9% of first implants in 2020). Among ischemic heart disease patients, the most common indication was primary prevention (56.1%). However, a considerable number of forms returned failed to note the reason or it was unclassifiable. The second most common reason for ICD implantation was dilated cardiomyopathy (27.1% of all first implants), and the absolute number of first implants increased in 2020 vs previous years, due to the increase in primary prevention indications. In the less common heart diseases, the most frequent indication was primary prevention.
Number of first implants according to the type of heart disease, type of clinical arrhythmia, and form of presentation from 2016 to 2020.
| 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|
| Ischemic heart disease | |||||
| Aborted SCD | 135 (10.4) | 101 (6.5%) | 165 (10.6) | 202 (11.2) | 183 (8.7) |
| SMVT with syncope | 142 (10.9) | 135 (8.7) | 92 (5.9) | 132 (7.3) | 105 (5.2) |
| SMVT without syncope | 226 (17.3) | 212 (13.7) | 231 (14.9) | 232 (12.9) | 204 (9.7) |
| Syncope without arrhythmia | 31 (2.4) | 61 (3.9) | 62 (3.9) | 62 (3.4) | 128 (6.1) |
| Prophylactic implantation | 650 (49.9) | 603 (39.0) | 793 (50.8) | 988 (54.9) | 1173 (56.1) |
| Missing/unclassifiable | 121 (9.3) | 434 (28.0) | 217 (13.9) | 181 (10.7) | 299 (14.3) |
| Subtotal | 1305 | 1546 | 1560 | 1797 | 2092 |
| Dilated cardiomyopathy | |||||
| Aborted SCD | 51 (5.9) | 61 (7.3) | 47 (5.6) | 42 (4.5) | 74 (5.9) |
| SMVT with syncope | 43 (5.0) | 65 (7.8) | 39 (4.8) | 45 (4.9) | 51 (4.1) |
| SMVT without syncope | 91 (10.5) | 100 (12.0) | 53 (6.6) | 121 (13.0) | 88 (7.1) |
| Syncope without arrhythmia | 59 (6.8) | 30 (3.6) | 26 (3.3) | 34 (3.7) | 59 (4.7) |
| Prophylactic implantation | 550 (63.5) | 341 (41.0) | 355 (44.2) | 547 (59.1) | 766 (61.7) |
| Missing/unclassifiable | 72 (8.3) | 233 (28.7) | 283 (35.2) | 136 (14.7) | 204 (16.4) |
| Subtotal | 866 | 830 | 803 | 925 | 1242 |
| Valve disease | |||||
| Aborted SCD | 12 (10.5) | 5 (5.3) | 9 (9.8) | 12 (12.4) | 12 (10.8) |
| SMVT | 28 (24.5) | 22 (23.2) | 24 (26.1) | 28 (28.7) | 21 (18.9) |
| Syncope without arrhythmia | 9 (7.9) | 5 (5.3) | 5 (5.4) | 2 (2.1) | 7 (6.3) |
| Prophylactic implantation | 52 (45.6) | 46 (48.4) | 37 (40.2) | 45 (46.4) | 52 (46.8) |
| Missing/unclassifiable | 13 (11.4) | 17 (17.9) | 17 (18.5) | 10 (10.3) | 18 (17.1) |
| Subtotal | 114 | 95 | 92 | 97 | 110 |
| Hypertrophic cardiomyopathy | |||||
| Secondary prevention | 49 (20.3) | 49 (21.5) | 48 (19.2) | 45 (14.2) | 80 (20.4) |
| Prophylactic implantation | 176 (70.3) | 166 (72.8) | 198 (79.2) | 207 (65.3) | 288 (73.5) |
| Missing/unclassifiable | 16 (6.6) | 13 (5.7) | 4 (1.6) | 65 (20.5) | 24 (6.1) |
| Subtotal | 241 | 228 | 250 | 317 | 392 |
| Brugada syndrome | |||||
| Aborted SCD | 16 (24.2) | 11 (15.5) | 14 (18.9) | 10 (12.0) | 10 (9.5) |
| Prophylactic implantation in syncope | 10 (15.2) | 16 (22.5) | 14 (18.9) | 23 (27.7) | 18 (17.1) |
| Prophylactic implantation without syncope | 35 (53.0) | 38 (53.5) | 14 (18.9) | 40 (48.2) | 56 (53.3) |
| Missing/unclassifiable | 5 (7.6) | 6 (8.4) | 17 (23.0) | 10 (12.0) | 21 (20.0) |
| Subtotal | 66 | 71 | 74 | 83 | 105 |
| ARVC | |||||
| Aborted SCD | 2 (4.3) | 3 (12.5) | 4 (10.3) | 4 (8.2) | 5 (8.9) |
| SMVT | 25 (54.3) | 7 (29.1) | 16 (41.0) | 14 (28.6) | 6 (10.7) |
| Prophylactic implantation | 18 (39.1) | 10 (41.6) | 14 (35.9) | 22 (44.9) | 29 (51.8) |
| Missing/unclassifiable | 1 (2.2) | 4 (16.6) | 5 (12.8) | 9 (18.4) | 16 (28.5) |
| Subtotal | 46 | 24 | 39 | 49 | 56 |
| Congenital heart disease | |||||
| Aborted SCD | 4 (12.1) | 6 (12.0) | 7 (15.2) | 6 (14.6) | 3 (7.0) |
| SMVT | 10 (30.3) | 10 (20.0) | 14 (30.4) | 11 (26.8) | 6 (13.9) |
| Prophylactic implantation | 12 (36.4) | 29 (58.0) | 21 (45.6) | 20 (48.8) | 27 (62.8) |
| Missing/unclassifiable | 7 (21.2) | 5 (10.0) | 4 (8.7) | 4 (9.7) | 7 (16.3) |
| Subtotal | 33 | 50 | 46 | 41 | 43 |
| Long QT syndrome | |||||
| Aborted SCD | 10 (30.3) | 15 (48.4) | 9 (24.3) | 15 (40.5) | 9 (21) |
| Prophylactic implantation | 15 (45.5) | 12 (38.7) | 18 (48.6) | 15 (40.5) | 23 (53.6) |
| Missing/unclassifiable | 8 (24.2) | 4 (12.9) | 10 (27.3) | 7 (18.9) | 11 (25.6) |
| Subtotal | 33 | 31 | 37 | 37 | 43 |
ARVC, arrhythmogenic right ventricular cardiomyopathy; SCD, sudden cardiac death; SMVT, sustained monomorphic ventricular tachycardia.
Data are expressed as No. (%).
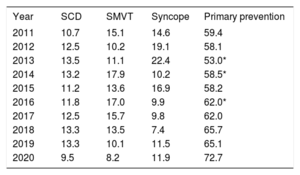
The implantation indication was identified in 62.2% of forms, and primary prevention was the main indication in first implants (72.7%). This figure is the highest in registry history (table 3).
Changes in the main indications for implantable cardioverter-defibrillators (first implants, 2011-2020).
| Year | SCD | SMVT | Syncope | Primary prevention |
|---|---|---|---|---|
| 2011 | 10.7 | 15.1 | 14.6 | 59.4 |
| 2012 | 12.5 | 10.2 | 19.1 | 58.1 |
| 2013 | 13.5 | 11.1 | 22.4 | 53.0* |
| 2014 | 13.2 | 17.9 | 10.2 | 58.5* |
| 2015 | 11.2 | 13.6 | 16.9 | 58.2 |
| 2016 | 11.8 | 17.0 | 9.9 | 62.0* |
| 2017 | 12.5 | 15.7 | 9.8 | 62.0 |
| 2018 | 13.3 | 13.5 | 7.4 | 65.7 |
| 2019 | 13.3 | 10.1 | 11.5 | 65.1 |
| 2020 | 9.5 | 8.2 | 11.9 | 72.7 |
SCD, sudden cardiac death; SMVT, sustained monomorphic ventricular tachycardia.
The implantation setting and specialist performing the procedure were recorded in 60.5% of forms; 85.6% of procedures were performed in electrophysiology laboratories and 13.3% in operating rooms. Cardiac electrophysiologists performed 82.4% of implants, surgeons performed 7.9%, and both together performed 5.5%. Other specialists and intensivists were involved in 1.5% and 2.7%, respectively.
Generator placement siteTransvenous ICD generator placement represented 65.5% of first implants, with a subcutaneous location in 95.6% of cases and subpectoral in the remaining 4.4%. These figures were 95.5% and 4.5%, respectively, for all devices implanted.
Device typeThe types of devices implanted are shown in table 4. This information was provided in 78.3% of forms submitted to the registry. In 2020, first implants of subcutaneous defibrillators became established, with a market penetration of 8.1%.
Percent distribution of implanted devices by type.
| Total | First implants | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2016 | 2017 | 2018 | 2019 | 2020 | |
| Subcutaneous | 3.6 | 3.8 | 4.4 | 6.2 | 5.7 | 6.4 | 5.3 | 6.0 | 8.3 | 8.1 | |||
| Single-chamber | 48.2 | 48.8 | 48.6 | 45.4 | 45.7 | 46.6 | 45.6 | 45.1 | 48.4 | 49.4 | 50.1 | 47.7 | 50.2 |
| Dual-chamber | 18.9 | 17.4 | 14.5 | 13.7 | 15.0 | 15.0 | 13.8 | 14.1 | 13.0 | 14.1 | 13.4 | 12.6 | 12.4 |
| Resynchronization device | 32.9 | 33.7 | 35.7 | 37.3 | 35.7 | 34.0 | 34.4 | 34.7 | 32.1 | 31.5 | 30.6 | 31.4 | 29.3 |
The most frequent reason for ICD generator replacement was battery depletion (84.3%); complications prompted 8.7% of replacements and a change in indication prompted 7.0%.
Of the 627 replacements providing this information, 1.7% were performed before 6 months. In addition, 30.2% of forms provided information on the status of leads, which were malfunctioning in 33 patients.
ComplicationsComplication data were recorded in 44.7% of forms. In total, 30 patients with complications were reported: 4 pneumothoraces, 3 coronary sinus dissections, 2 tamponades, 2 deaths, and 24 unspecified. The mortality rate was 0.06%, which fortunately was very low, as in previous years.
DISCUSSIONThis year, the Spanish Implantable Cardioverter-defibrillator Registry has managed to reflect almost all of the implants performed in Spain, with a data inclusion rate of 99.3% vs Eucomed data. This was possible due to the collaboration of the implantation centers and the tireless work performed by the SEC. The figures are similar to those of previous years, with major differences in implantation rates among the different autonomous communities and a mean implantation rate much lower than the European average. Finally, the 2020 registry shows a notable reduction in the number of ICD implants vs the last 2 years, a reflection of the impact of the COVID-19 pandemic on ICD implantation activity in Spain.
The SEC has published the Spanish Implantable Cardioverter-defibrillator Registry annually since 2005.5 This consistency allows us to identify trends in ICD implantation, the types of devices used, and the characteristics of patients undergoing ICD implantation in Spain in recent years.
Over time, there has been an increase in the number of ICD implants, with isolated reductions in the 2011 to 2012 period and in 2017 vs previous years. The years showing the highest ICD implantation activity were 2018 and 2019. However, 2020 exhibited a slight reduction, about 4%, in the number of ICD implants. The COVID-19 pandemic has had a dramatic impact on hospital activity, and numerous studies have found a reduction in hospitalizations for acute coronary syndrome and in cardiac catheterizations in both Europe, including Spain, and the United States in the initial months of the pandemic.12–14 A registry including 66 German hospitals revealed a 27% reduction in hospital admissions for cardiac arrhythmias and in interventional activity for cardiac arrhythmias between March and April 2020.15 Specifically, implantation of cardiac devices (pacemakers and ICDs) fell by 24%. In the region of Veneto, Italy, the number of urgent pacemaker implantation decreased by 29% after the detection of the first COVID-19 cases vs the previous weeks or the same period in 2019.16 Spain also showed a significant reduction in urgent pacemaker implantation, which reached 35% between March 15 and May 15, 2020, vs the same period of the previous year.17
ICD implantation activity has also been affected by the pandemic. In a registry recording the activity of 9 hospitals in Catalonia, ICD implantation fell by 66.7% between March 15 and April 30, 2020, vs the same period before COVID-19.18 The data from the present registry showed a highly pronounced decrease in the number of ICD implants between March and June 2020, particularly in April (with a 50% reduction vs April 2019). Worldwide, only a 4% reduction in ICD implantation activity was detected in 2020 vs 2019 due to the recovery in activity in the second half of the year after the initial impact of COVID-19. These results break with the trends observed in previous years for an increase in the number of ICD devices implanted and the reduction in the difference in the implantation rate between Spain and the other European countries. Finally, it is important to stress that this reduction in activity could have negative consequences for patients, including an increase in cardiovascular morbidity and mortality.
The Spanish implantation rate is one of the lowest in Europe. In the last 2 years, the implantation number slightly increased in Spain and slightly decreased in Europe,11 which would have partly reduced the difference. In 2010, the rate of implantation per million population in Spain was less than half that of Europe (116 vs 248). In 2020, the difference was slightly reduced, with 150 implants per million in Spain (vs 157, 152, and 138 in 2019, 2018, and 2017, respectively), whereas the figures for Europe fell from 303 in 2019 to 285 in 2020. In other words, during the toughest year of the pandemic, the implantation rate in Spain fell by 4.4%, whereas the decrease in Europe was 5.9%.
The decrease seen in the ICD implantation rate in 2020 worsened the situation in Spain, which has an implantation rate below that which would be expected according to the recommendations of clinical practice guidelines.1–3 This is something that is not exclusive to Spain; in a Swedish study, just 10% of patients with a primary prevention indication for an ICD between 2000 and 2016 ultimately received an ICD.19 Implantation improved survival outcomes, with mortality reductions of 27% in the first year of follow-up and of 12% at 5 years. Another recent European registry also showed through diverse analyses the benefit of ICDs in the primary prevention of sudden cardiac death in ischemic and nonischemic patients, with a 27% reduced risk of death during a mean follow-up of 2.5 years.20 Our registry results indicate a clear underuse of ICD therapy in Spain that has been worsened by the COVID-19 pandemic and highlight the importance of adopting measures to implement the therapy in patients who may benefit from it.
This latest Spanish Implantable Cardioverter-defibrillator Registry confirms the increase in primary prevention indications detected in recent years, with a 72.7% rate of prophylactic implantation (table 3). In the last 10 years, prophylactic indications have increased by 27%. Our rate is close to that of Europe, where primary prevention is the leading indication for ICD implantation, with rates of about 80%.21,22
Regarding the type of device implanted in Spain, the data showed a slight decrease in the percentage of first ICD-CRT implants (29.3% in 2020 vs 31.4% in 2019, 30.6% in 2018, 31.5% in 2017, and 32.1% in 2016) (table 4). The percentage of first implants of dual-chamber ICDs also decreased. Subcutaneous ICDs fell slightly to 8.1%. In 2020, the results were published of 2 studies supporting the effectiveness and safety of subcutaneous ICDs. The PRAETORIAN trial compared transvenous and subcutaneous ICDs in 849 patients with a class I indication for ICD implantation in both primary and secondary prevention.23 The results showed that subcutaneous ICD was not inferior to transvenous ICD in the composite endpoint of ICD-related complications and/or inappropriate shocks and had similar effectiveness. The UNTOUCHED study assessed the safety of subcutaneous ICD in a series of patients in primary prevention and identified an inappropriate shock-free survival of 95.9%.24 We will have to wait until next year to know the impact of these new data on the market.
The most frequent indication in 2020 continued to be ischemic heart disease (50.9%), followed by dilated cardiomyopathy (27.1%). These data show a stabilization in the percentage of patients with dilated cardiomyopathy vs a reduction in previous years. This reduction has followed the publication of the DANISH trial,25 which led to a fall in the primary prevention indications for this heart disease. This phenomenon was also seen to a greater or lesser extent in other European countries.26 The recovery in the indication for ICDs in patients with dilated cardiomyopathy is in line with the increase in the prophylactic indication observed in 2020.
The epidemiological characteristics of the patients are unchanged vs previous years. Patients with severe ventricular dysfunction and in NYHA II and III continue to predominate. No changes were seen either in the specialist performing the implantation and most procedures were once again performed in the electrophysiology laboratory.
Differences among autonomous communitiesThe 2020 registry confirms the major differences in implantation rates per million population among Spanish autonomous communities. Several communities showed higher than average rates: Cantabria, Aragon, the Principality of Asturias, Galicia, Valencian Community, Castile-La Mancha, Castile and León, and the Community of Madrid. Below the average were Region of Murcia, the Chartered Community of Navarre, Extremadura, Catalonia, Andalusia, La Rioja, the Basque Country, the Balearic Islands, and the Canary Islands. The data from 2020 indicate an increase in the difference between the communities with the highest (Cantabria) and lowest (the Canary Islands) rates of implantation per million population. The gap has widened to 180 units/million population from 139/million in 2019. The disparity in the ICD implantation rate among the various autonomous communities, present in previous registries and magnified in the current registry, is hard to explain. It cannot be explained by the gross domestic product per capita in each autonomous community, by health expenditure or population density, or by a different incidence in the type of heart disease most prevalent in each community. The COVID-19 pandemic may have unequally affected the autonomous communities and could explain the aggravation in the pre-existing differences in Spain. This situation might call into question the equity of our health care system in an area as important as the prevention of sudden cardiac death.
Comparison with other countriesIn 2020, the implantation rate in the countries participating in the Eucomed was 285/million population, dropping below 300/million population for the first time in more than 5 years. The countries with the highest implant numbers were the Czech Republic and Germany (474 and 445/million population, respectively). One consistent result is that Spain (150 implants/million population in 2020 and 157/million in 2019) is the country with the lowest number of implants.
Other European countries also exhibit regional differences22 that cannot be easily explained. A possible reason is the number of arrhythmia units available, but countries with many units have low implantation rates. Regarding income, countries with lower incomes than Spain, such as Ireland, the Czech Republic, and Poland, have higher implantation rates. The prevalence of cardiovascular disease also fails to explain these differences. The low implantation rate reflects a low level of adherence to clinical practice guidelines, which has been linked to increased mortality. We need to be aware of this problem and do everything in our power to alleviate it.
LimitationsAs in previous years, completion of the different fields in the implantation form varied and was lower than desired. In addition, no follow-up data were collected from patients, which would permit more relevant clinical studies. Finally, the unequal completion of the data on ICD-associated complications and the absence of follow-up data probably underestimate the actual complication rate.
CONCLUSIONSThe 2020 Spanish Implantable Cardioverter-defibrillator Registry collected information on 99% of all implants performed in Spain, approximating the totality of the activity and current indications for this therapy in Spain. In 2020, the total number of implants per million population fell as a result of the impact of the COVID-19 pandemic. This reduction has been unequal and has increased the differences in ICD implantation rates among the autonomous communities. In addition, the difference in the implantation rate between Spain and the other European countries is still wide, which compels us to improve our ability to identify patients who may benefit from this therapy.
FUNDINGFor the maintenance and collection of the data included in the present registry, the SEC has benefited from a grant from the Spanish Agency of Medicines and Medical Devices (AEMPS), the proprietor of these data.
AUTHORS’ CONTRIBUTIONSAll of the authors of this article analyzed the data, wrote and revised the manuscript, and are responsible for this publication. The first author is additionally responsible for the entry and cleaning of the data, together with a technician and SEC computer scientist.
CONFLICTS OF INTERESTFernández Lozano has participated in clinical studies sponsored by Medtronic, Abbott, Biotronik, and Sorin and receives fellowship grants from the SEC and the Interhospital Foundation for Cardiovascular Research. J. Osca Asensi has participated in clinical studies sponsored by Abbott, Boston, and Biotronik. J. Alzueta Rodríguez has participated in presentations sponsored by Boston and receives fellowship grants from the FIMABIS Foundation.