Keywords
INTRODUCTION
Implantable cardioverter-defibrillators (ICDs) have become a well-established therapeutic option for secondary prevention in patients with malignant ventricular arrhythmias. The number of indications in primary prevention in patients at risk of arrhythmias has also increased.1-10
Several scientific societies have published recommendations for the indications for these devices and the resources needed for this therapeutic option.11-14 However, little information is available on the actual use and indications of these devices either in Spain or internationally.15-23
Health registries are a valuable source of information for assessing the day-to-day reality of clinical practice and the actual outcomes of applying the findings of large multicenter studies and clinical guidelines.24,25 In 1996, the first National ICD Registry was set up in Spain, and the findings were published in 1997.15 In 2001, the Working Group on Implantable Cardioverter-Defibrillators (abbreviated to GT-DAI in Spanish) was set up within the Electrophysiology and Arrhythmias Working Group of the Spanish Society of Cardiology (SEC). One of the main aims was to set up the SEC's National ICD Registry. This publication of the GT-DAI presents the data of ICD implantations reported to the Registry in the 3 years spanning 2002 to 2004 and covers the majority of centers that implant ICDs in Spain.
MATERIALS AND METHOD
Data for the Registry were collected prospectively. A questionnaire was drawn up, and the final version was approved by the members of the Electrophysiology and Arrhythmias Working Group (Annex). The questionnaire, which is available on the web page of this Working Group (www.arritmias.org), was sent to arrhythmia units in Spain, the members of the Working Group, and the companies that market ICDs in Spain.
The questionnaire was filled in directly and voluntarily by each implant team during or after ICD implantation, and sent by fax or e-mail to the SEC.
The SEC collaborated in creating the database and in data entry. Data were checked for consistency by a SEC computer technician and a member of the GT-DAI. Previous and current board members of the GT-DAI were responsible for data analysis and publication of the findings.
Population data for calculation of rates per million inhabitants, for the all of Spain and for Spanish autonomous regions and provinces, were obtained from estimates made for the years 2002, 2003, and 2004 by the National Institute of Statistics (www.ine.es).
The GT-DAI board requested information on the total number of ICDs implanted in 2002, 2003, and 2004 from the companies that market ICDs in Spain in order to determine how many of the ICD implantations done in Spain were reported to the Registry and in turn to give an indication of how representative the Registry is. Thus, the total number of implants and the number of implants reported to the Registry allowed the calculation of a correction factor which was used to estimate the overall numbers of implants by autonomous region and province.
Statistical Analysis
Numerical results were expressed as means±standard deviation for variables with a normal distribution, and as medians and interquartile ranges for variables not normally distributed. Qualitative variables were compared with the χ2 test and quantitative variables by analysis of variance. The relationship between quantitative variables was analyzed with a linear regression model. Statistical significance was set at P<.05.
RESULTS
The proportion of the questionnaire fields were filled out was high, and this proportion remained stable throughout the 3 years, ranging from 83% to 97% for the main variables of the Registry.
Implant Centers
In 2002, 72 centers that performed ICD implantations reported data to the Registry, compared to 78 in 2003, and 80 in 2004 (Table 1). Most centers were in the public health sector (58 in 2002, 61 in 2003, and 68 in 2004). Table 2 shows the number of public hospitals per million inhabitants that performed ICD implantation in each autonomous region.
Total Number of Implantations
The total number of implantation procedures (initial implants and replacements) reported to the Registry increased progressively over the 3 years. Thus, ICDs were implanted in 925 patients in 2002, 1046 in 2003, and 1414 in 2004. Given that the estimated total number of implants in these years was 1477, 1778, and 2097, respectively, reports reaching the Registry represented 63%, 59%, and 67.5%, respectively, of the total number of ICDs implanted in Spain.
The total number of implantations per million inhabitants reported to the Registry was 22 in 2002, 24 in 2003, and 33 in 2004. The estimated total number of implants per million inhabitants was 35, 41, and 49, respectively (Tables 3 and 4). There was no significant correlation between the number of hospitals performing ICD implants and the number of ICDs implanted per million inhabitants (r2=0.21; P=.07).
Most implantations took place in public hospitals, which accounted for 894 procedures in 2002, 1009 in 2003, and 1386 in 2004, corresponding to 96%, 98%, and 98%, respectively, of the total number of procedures reported to the Registry.
Initial Implants Versus Replacements
The number of initial implants was 691 in 2002, 702 in 2003, and 945 in 2004, which represented 80%, 71%, and 70%, respectively, of all procedures reported to the Registry. The number of initial implants per million inhabitants reported to the Registry was 18 in 2002, 17 in 2003, and 23 in 2004, and the estimated number of initial implants in the same years was 28, 29, and 34, respectively. The number of replacements done was 174 in 2002 (20%), 284 in 2003 (29%), and 378 in 2004 (30%).
Age and Sex
The median age of patients receiving an ICD was 66 years (interquartile range, 54-72 years; range, 1-86 years) in 2002, 66 years (interquartile range, 54-73 years; range, 4-85 years) in 2003, and 65 years (interquartile range, 54-66 years; range, 10-85 years) in 2004. The sex of the recipient was predominantly male--87% in 2002, 85% in 2003, and 86% in 2004. Similar age and sex distributions were reported for initial implants.
Underlying Heart Disease, Left Ventricular Ejection Fraction, Functional Class, and Initial Rhythm
Figures 1 and 2 and Tables 5 and 6 show the patients heart disease by total number of ICDs implanted and initial implants. The most common underlying condition was ischemic heart disease. The percentages of different heart diseases were similar over the 3 years, and no statistically significant differences in the distribution were observed. Other common conditions were noncompactation cardiomyopathy, peripartum cardiomyopathy, Steinert disease, idiopathic sustained monomorphic ventricular tachycardia (SMVT), Prinzmetal angina, restrictive cardiomyopathy, etc.
Figure 1. Heart disease in the patients reported to the Registry (initial implants and replacements). RVAD indicates right ventricular arrhythmogenic dysplasia.
Figure 2. Heart disease in patients reported to the Registry (only initial implants). RVAD indicates right ventricular arrhythmogenic dysplasia.
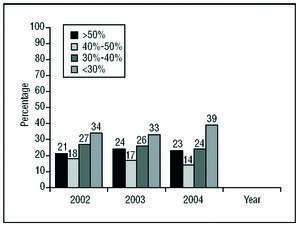
Most patients had a left ventricular ejection fraction (LVEF) of less than 30% or between 30% and 40% (Figure 3). The percentage of patients with LVEF above 50% was greater than that of patients with mild dysfunction (LVEF of 40%-49%). A greater percentage of patients with severe left ventricular dysfunction (LVEF<30%) was reported in 2004 compared to 2003 and 2002 (38.3% vs 33.6% and 34.2%, respectively; P<.01) whereas a smaller percentage had mild dysfunction (LEVF of 40%-50%) (14% in 2004 vs 17% and 18%, respectively; P<.01). On analysis of initial implants only, the percentages of patients in each LVEF range were similar to those for all types of ICD implantation.
Figure 3. Left ventricular ejection fraction of the patients
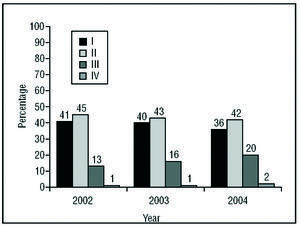
The majority of patients were in NYHA functional class II or I. The percentage of patients in functional class III was smaller, and rarely were patients in functional class IV (Figure 4). An increasing and statistically significant trend (P<.001) towards larger number of implants in patients in functional class III was observed at the expense of those in functional classes I and II, largely as a result of increased indication of ICD with cardiac resynchronization.
Figure 4. New York Heart Association Functional Class of the Patients in the Registry.
Most patients were in sinus rhythm--83% in 2002, 82% in 2003, and 81% in 2004. Atrial fibrillation was reported in 13% of the patients over the 3 years. Paced rhythm was reported in 3%, 4%, and 5% in 2002, 2003, and 2004, respectively.
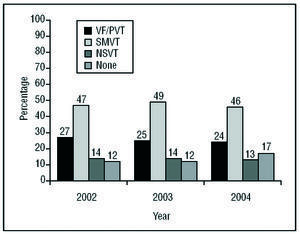
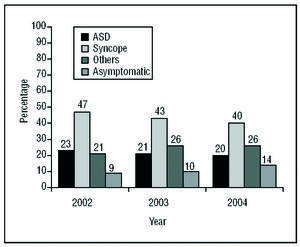
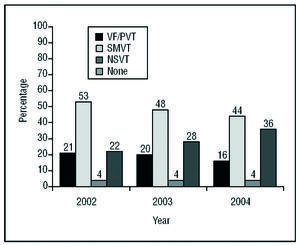
Clinical Arrhythmia Leading to Implantation, Form of Presentation, and Induced Arrhythmia in the Laboratory (Figures 5-7)
Figure 5. Clinical Arrhythmia of the Patients in the Registry. VF indicates ventricular fibrillation; SMVT, sustained monomorphic ventricular tachycardia; NSVT nonsustained ventricular tachycardia; PVT, polymorphic ventricular tachycardia.
Figure 6. Form of clinical presentation of the arrhythmia in patients in the Registry. ASD indicates aborted sudden death.
Figure 7. Arrhythmia indicated in the laboratory in patients who underwent electrophysiological study. VF indicates ventricular fibrillation; SMVT sustained monomorphic ventricular tachycardia; NSVT, nonsustained ventricular tachycardia; PVT, polymorphic ventricular tachycardia.
Implantation was indicated for SMVT in almost half of the cases. The second most common type of clinical arrhythmia was ventricular fibrillation or polymorphic ventricular tachycardia. The remaining devices were implanted as prophylaxis in patients with nonsustained ventricular tachycardia or with no documented clinical arrhythmia. The most common form of presentation was syncope, followed by "other symptoms," and cardiorespiratory arrest.
Indications (Tables 5 and 6)
The most common indication for ICD implantation was secondary prevention in patients with ischemic heart disease, mainly with SMVT and aborted sudden death. In 2003 and 2004, there was a statistically significant decrease in the number of implantations due to aborted sudden death in patients with this type of heart disease (19.5% in 2002 vs 13.4% and 13.2%, respectively; P<.01). There was also a decrease in the percentage of indications for SMVT with syncope (16.3% in 2004 vs 20.9% in 2003 and 25.9% in 2002) and an increase in the indications in patients with SMVT episodes without syncope from 19.5% in 2002 to 27.5% in 2004 (P=.001). Indications corresponding to those in the MADIT I or MUSST5,6 remained stable over the years. In contrast, other prophylactic indications increased progressively and statistically significantly between 2002 and 2004, representing just 10% in 2002 compared to 21.5% in 2004 (P<.001).
For patients with dilated cardiomyopathy, the most common indication was also SMVT, with fewer indications for SMVT with syncope in 2004 compared to previous years (7.7% in 2004, 27.3% in 2003, and 22.8% in 2002; P<.01). The next most common indication was aborted sudden death, which followed a progressive nonsignificant trend downwards over the 3 years. Prophylactic indications increased significantly in the last year (24.4% vs 14% and 16.5% in the previous years; P=.01).
Implantation Site and Specialist Who Did the Operation Implantation
An increasing number of implantations were done in the electrophysiology laboratory (48.6% of the procedures in 2002, 51% in 2003, and 58% in 2004; P<.001). In the remaining cases, implantation was done in the operating room.
Over the 3 study years, the number of implantations done by electrophysiologists increased (accounting for 48.3% of the procedures in 2002, 53% in 2003, and 59.4% in 2004; P<.001) at the expense of the proportion of implants done by heart surgeons (48.4%, 44%, and 35.6%, respectively). Implantation was done by other types of specialist in 3.3% of the cases in 2002, 3% of the cases in 2003, and 5% of the cases in 2004.
Generator Site
Subcutaneous pectoral implantation was the most common site for the generator, with the proportion of devices implanted in this site increasing over the 3 years (69% in 2002, 73% in 2003, and 81% in 2004; P<.001). The submuscular pectoral site was used in 29%, 25%, and 17% of the implanted patients in 2002, 2003, and 2004, respectively. In each study year, 2% of all implantation sites were abdominal, these procedures being replacements in all but one, corresponding to an implantation in a child.
Device Type
A single-chamber device accounted for 65% of implants in 2002, 69% in 2003, and 57% in 2004. Dual-chamber devices were implanted in 28%, 24%, and 29% of the recipients, respectively. Implantation of ICDs with cardiac resynchronization was done in 6%, 7%, and 14% of the cases in 2002, 2003, and 2004, respectively, with an increase in 2004 with respect to the previous years (P<.01).
Reasons for Device Replacement: Need for New Electrodes When Replacing the Generator and Use of Additional Electrodes
In 2002, 90% of the replacements reported were done because of battery failure and the remaining 10% because of complications, 88% of which occurred at least 6 months after implantation. In 2003, 88% were due to battery failure and 12% to complications (79% more than 6 months after implantation). In 2004, the percentage of replacements due to battery failure was 90%, and 61% of the complications documented were late complications. In 2002, 6% of electrodes were replaced because of malfunction, compared to 8% in 2003, and 9% in 2004. In 13%, 63%, and 87% of the cases, respectively, electrodes were removed because of malfunction. Additional defibrillation electrodes or sensing electrodes were only rarely used (9 times in 2002, 10 in 2003, and 8 in 2004).
Minimum Defibrillation Energy
In 2002, the mean±standard deviation minimum defibrillation energy was less than 16.9±4.9 J, compared to less than 17.6±4 J in 2003 and less than 17.8±4.2 J in 2004. The limits of minimum effective defibrillation energy over the 3 years ranged from 6 J to 36 J.
Programming the Implantable Cardioverter-Defibrillator
Antibradycardia pacing was used mainly in VVI mode (55% in 2002, 57% in 2003, and 51% in 2004). Overall, VVIR mode was used in 13% in 2002, 14% in 2003, and 13% in 2004, whereas DDD mode was programmed in 11%, 9%, and 12%, respectively, and DDDR mode in 11%, 9%, and 12%, respectively.
Antitachycardia pacing was programmed in 83%, 85%, and 86% in the respective study years for ventricular arrhythmias. Such pacing was programmed for both the ventricle and atrium in 3%, 1%, and 3%, respectively. In 14%, 14%, and 13% of the cases, respectively, no antitachycardia programming was done.
Complications
No deaths were associated with implantation procedures in 2002, whereas 1 death was reported in 2003 and 3 in 2004, corresponding to a mortality rate of 1.2 per thousand and 2.4 per thousand implants, respectively. No cases of tamponade were reported during the procedure in any of the 3 years. Pneumothorax was reported in 3 patients in 2002, 1 in 2003, and none in 2004. Minor unspecified complications were reported with 17 implantations in 2002, 9 in 2003, and a further 9 in 2004.
DISCUSSION
Usefulness of the Spanish Implantable Cardioverter-Defibrillator Registry
The Electrophysiology and Arrhythmias Working Group of the SEC publishes an annual report on the findings of the National Catheter Ablation Registry in the field of arrhythmias.26 For ICDs, the Working Group itself started the National ICD Registry in 1996, and the results were published in 1997.15 One of the main aims for 2001 of the recently established GT-DAI was to set up the Spanish ICD Registry. The results from the period 2002 to 2004 are published in this article.
This Registry serves as a good reference for arrhythmia units throughout Spain who wish to assess their own activity, given that registries are usually more representative of the day-to-day reality in a country than data from multicenter clinical trials. On the other hand, data obtained from a large number of procedures over a limited period provide a better indication of possible influences of different multicenter studies published in the literature and the effects of technological innovations on the indications of ICDs, the type of devices implanted, and their programming. In addition, the information of the ICD Registry highlights geographic differences in resources, indications, and number of ICD implants within Spain and should help health managers adapt health planning in this field.
Comparison With the 1996 Registry
In 1996, two thirds of the implantation procedures were reported to the Registry.15 Comparison of the present results with those from 1996 reveals a marked increase in the number of implantations and the number of centers performing implantations. The total number of implantations reported to the Registry in 1996 was 306, compared to 1414 in 2004. The number of implantations per million inhabitants, including both initial implants and replacements, was 9 in 1996 compared to 49 in 2004. Thirty-six centers performed implantations in 1996 compared to 80 in 2004. There was also a notable change in the type of indications. In the 1996 Registry, most implantations were done in patients who had been resuscitated after aborted sudden death or who had presented with SMVT, usually with syncope, whereas prophylactic implants were not reported. In contrast, the proportion of prophylactic implantations has increased significantly in recent years, as reflected by studies published in the literature.5-10 The site of ICD implantation has also changed substantially (subcutaneous pectoral implantation accounted for 19% of the procedures in 1996 compared to 80% at present). Important changes have also occurred in the place where the implantation is done (15% in the electrophysiology laboratory in 1996 vs 58% in 2004) and in the person who performs the procedure (17% done by the electrophysiologist in 1996 vs 59.4% in 2004).
Comparison With Registries Outside Spain
Information on ICD implants from other countries is limited.16-23 Few countries in the European Community (Denmark, Sweden, Italy, and the United Kingdom) run national registries, and most do not publish their results. The Danish ICD Registry collects information on all implantations done in Denmark since 198916 and publishes a report every year on the web site www.pacemaker.dk. In 2003, 350 initial devices and 153 replacements were implanted (68 initial implants per million inhabitants). The proportion of initial implants to replacements is similar to Spain. The most common cardiomyopathy was ischemia (52%), followed by dilated cardiomyopathy (21.4%). The arrhythmias that most often led to implantation were SMVT, reported in 53.4% of the cases, and ventricular fibrillation, reported in 33.1%. Dual-chamber ICDs were implanted in 36.3% of the cases and resynchronization devices with ICDs in 6%.
The German ICD Registry, EURID, is a project that was launched in 1998 by the Arrhythmias Working Group of the German Society of Cardiology.17 Participation was voluntary, and initially 62 centers took part, although this number had decreased to 34 by 2000. Between January 1998 and October 2000, information was collected on 3344 ICD implantations. The mean age of the implant recipient was 61 (12) years, and 80.2% were done in men. The most common heart disease, as in Spain, was ischemic heart disease, reported in 64% of the patients and dilated cardiomyopathy, reported in 18.9%. Overall, 54% of the patients were in functional class II and 47% had an ejection fraction of 20% to 50%. Most devices were implanted in patients who had suffered cardiac arrest (44%) or SMVT with syncope (24.7%). Dual-chamber ICDs were implanted in 21.6% of the patients.
The European Cardiac Pacing Registry also collects information on defibrillators implanted in Europe, and results are available at the web site www.heart.org. uk/ewgcp. The most recent data were published in 2001 and correspond to 1997, although these data were retrospective and not very representative of the actual numbers of ICDs implanted.19
At present, the United States has no national registry on defibrillators. However, the Bilitch Registry, which was created in 1974 to collect information on pacemaker implantation, later also gathered data on ICDs.18 The registry disappeared in 1993 due to lack of funding.20 The most recent data published in the literature on implantation in the United States date from 1997, and were collected by members of NASPE and ICD manufacturers. In total, 35 630 ICD devices were implanted in 817 hospitals (107 initial implants per million inhabitants).
Overall Number of Implantations, Indications, and Trend
The number of procedures reported to the Registry and the total estimated number have increased each year. This increase is due, above all, to an increased number of indications, particularly of the prophylactic type, probably because a number of studies have demonstrated the usefulness of ICDs in primary prevention.7-10 The increased number of centers that carry out implantations and perhaps a better management of patients with malignant ventricular arrhythmias may also have contributed to the increased number of implants.
Ischemic heart disease is the most common underlying condition leading to ICD implantation. Among patients with this underlying condition, those with SMVT and aborted sudden death occurred most frequently. The number of prophylactic implantations has increased significantly in recent years, probably because of the publication of the findings of the MADIT II study and the presentation of the SCD-HeF study.7,10 The proportion of patients with implantations due to aborted sudden death has decreased in the last year. The number of implantations for SMVT has remained relatively stable, although in the last 2 years, the proportion of implantations for SMVT without syncope was greater than that of patients with syncope during tachycardia, reversing the trend of the first year. This is partly due to the greater number of prophylactic implantations and a trend towards implanting ICDs in patients with severe ventricular dysfunction, even though they tolerate tachycardia.
Prophylactic indications have also increased in cases of dilated cardiomyopathy, probably in association with the publication of the results of the COMPANION and SCD-HeF studies, and to a lesser extent, those of the DEFI-NITE study.8-10 The number of resynchronization ICDs has increased significantly in such patients and also in those with ischemic heart disease.
Geographic Distribution: Regional Differences
The estimates of implants per million inhabitants based on the Registry showed marked variations from one Spanish autonomous region to another and within provinces of the same autonomous region. While considering the limitation that only two thirds of the implants are reported to the Registry, these variations implantation rates among and within autonomous regions cannot be readily explained by differences in the incidence of heart disease in Spain and so must be attributed to other reasons. One possibility is that, in some autonomous regions, hospitals performing implantations tend to concentrate in the capitals of those regions. Another possible explanation is that some hospitals have a weaker "arrhythmia culture" or, in contrast, ICD implantation is done by some services that do not have other therapeutic options available. In particular, catheter ablation might sometimes be preferable to ICD implantation. On the other hand, variations in the availability of centers performing implantations among autonomous regions is probably not a decisive factor, as there is no clear correlation between the number of centers performing implantations and the number of implantations per million inhabitants.
Complications
The incidence of complications associated with implantations is very low, although it should be remembered that the data collected by the Registry refer exclusively to complications during the implantation procedure itself.
Limitations
The main limitation of the Registry is that participation ranged from 59% to 67.5%, and so cannot be truly representative. Nevertheless, the level of participation is acceptable considering that this is a prospective registry that included a large number of ICD implantations. Moreover, the increase in the number of implants reported to the Registry in 2004 highlights the commitment of the professionals who participate in ICD implantation procedures to consolidate it.
National registries of different hospital care activities are descriptive and the consistency of information may vary widely according to autonomous region and hospital. This limitation should be remembered when assessing the reliability of subpopulation data from different autonomous regions and provinces.25
Future Prospects
The usefulness of the Spanish ICD Registry is beyond doubt and all professionals involved in the treatment of arrhythmias should be congratulated for contributing to one of the few national ICD registries kept anywhere in the world. These benefits should act as encouragement to ensure the continuity of the project and to improve quality of the data, especially by increasing the number of implantations that are reported to the Registry and extending the patient data collected and improving the control and verification procedures. Some fields are to be changed and some new fields will appear in the questionnaire in order to bring it into line with the recommendations of the CARDS project.27
Legislation SCO/3603/2003, dated December 18, published in the Official Gazette of the Spanish State, no. 309, dated December 26, 2003, provided for the creation of several national implantation registries, among them, 1 for cardiac implantations, run by the Spanish Medicines and Healthcare Products Agency. In accordance with this piece of legislation, a collaboration agreement was signed by the SEC and the Agency which should increase the importance of the National ICD Registry.
Aside from these legal aspects, our main motivation should be to obtain real data from Spain to help improve health care, establish epidemiological or clinical lines of investigation that draw on information from the Registry, and ensure that technical and human resources are more efficiently managed by the pertinent bodies.
CONCLUSIONS
The Spanish ICD Registry for 2002 to 2004 is one of the largest samples of ICD implantation procedures published in the international literature and can be considered representative of this activity and the outcomes of the procedure in Spain. The number of implantations has grown in Spain, and was estimated to be 49 per million inhabitants in 2004 (34 per million inhabitants for initial implants). Large regional and provincial variations are observed in the number of ICD implants per million inhabitants. The most common underlying reasons for implantation were SMTV and aborted sudden death, particularly in patients with ischemic heart disease or dilated cardiomyopathy. An increasing number of implants are done in the electrophysiology laboratory and by electrophysiologists. The incidence of complications during implantations is very low.
ACKNOWLEDGEMENTS
To SEC for support in setting up and running the Registry, and particularly to Mr Gonzalo Justes, Ms Patricia Aragón, and Ms Eva Cardenal.
To representatives of ICD manufacturers (Medtronic, Guidant, St Jude Medical, Biotronik and Ela Medical) for collaborating in data collection and returning questionnaires on a large number of implants to the SEC.
ABBREVIATIONS
LVEF: left ventricular ejection fraction.
GT-DAI: Working Group on Implantable
Cardioverter-Defibrillators.
ICD: implantable cardioverter-defibrillator.
SEC: Spanish Society of Cardiology.
SMVT: sustained monomorphic ventricular
tachycardia.
Correspondence: Dr. R. Peinado.
Unidad de Arritmias. Servicio de Cardiología.
Hospital Universitario La Paz.
P.o de la Castellana, 261. 28046 Madrid. España.
E-mail: rpeinado@secardiologia.es