This report describes the results of analysis of implanted pacemakers reported to the Spanish Pacemaker Registry.
MethodsThe analysis was based on information provided by the European Pacemaker Identification Card.
ResultsInformation was received from 115 hospitals, with a total of 12 697 cards, representing 32.3% of the estimated activity. Use of conventional and resynchronization pacemakers was 818 and 79 units per million inhabitants, respectively. A total of 200 leadless pacemakers were implanted. The mean age of the patients receiving an implant was 77.8 years, and 52% of devices were implanted in persons older than 80 years. In all, 74.9% were first implants and 23.4% corresponded to generator exchange. Endocardial leads were bipolar, 82.9% with active fixation, and 16.1% had magnetic resonance imaging protection. Most patients received bicameral sequential pacing, although single chamber pacing VVI(R) was used in 26.7% of the patients with sick sinus syndrome and in 23.8% of those with atrioventricular block, despite sinus rhythm.
ConclusionsTotal use of pacemaker generators in Spain has increased by 1.6% compared with 2015. Most implanted leads have active fixation and less than 20% have magnetic resonance imaging protection. Age and sex directly influenced pacing mode selection, which could be improved in around 32% of patients.
Keywords
The official report of the Spanish Pacemaker Registry has been published annually since 1997,1–15 and describes cardiac pacing procedures performed in Spain in the previous year. This report describes real-world clinical practice, the extent to which these procedures are in line with current clinical guidelines, evolving trends in recent years, and compares these pacing procedures with those conducted in other European countries.16 The current report provides information on pacemakers implanted in 2016.
METHODSThe Spanish Pacemaker Registry uses 3 information sources to prepare the annual report: the Spanish National Institute of Statistics (Instituto Nacional de Estadísticas [INE]),17 the European Patient Pacemaker Identification Card (EPPIC), and companies that supply the devices.
European Pacemaker Patient Identification CardEach year, the participating hospitals submit information on pacemaker implantation to the Spanish Pacemaker Registry. This information is based on the data contained in the EPPIC. Some hospitals send electronic data from their own databases. The implementation of the online application developed in agreement with the Spanish Agency of Medicines and Medical Devices remains pending. This application will allow greater involvement of the implanting hospitals, improved quality of data collection, and a more reliable and representative analysis of cardiac pacing activity in Spain.
Device SuppliersCurrent legislation on monitoring possible alerts (Royal Decree 1616/2009, dated 26 October, which regulates all active implantable healthcare devices), requires all implanting hospitals to complete the EPPIC. However, less than 100% of the cards are completed and some hospitals fail to send the EPPIC to the Spanish Pacemaker Registry. Therefore, data on all devices (pacemaker generators and cardiac resynchronization therapy [CRT] devices: high-energy [CRT-D] and low-energy [CRT-P]) implanted in Spain and their distribution by autonomous community is provided by the suppliers each year. The information provided by the suppliers to the Spanish Pacemaker Registry is compared with that reported by the European Confederation of Medical Suppliers Associations (Eucomed).18
Spanish National Institute of StatisticsThe population figures used to calculate the national and autonomous community implant rates were obtained from the INE updated report dated July 1, 2016.17
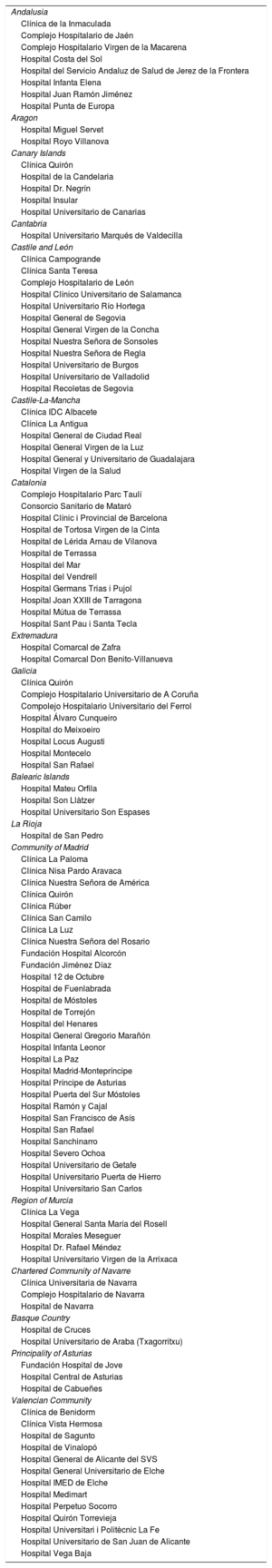
Sample AnalyzedA total of 115 centers (Table) provided 12 697 cards reporting 12 654 implants, which represents 32.3% of the generators used according to the information provided by the suppliers. This sample is considered representative of cardiac pacing activity in Spain in 2016.
Public and Private Hospitals Submitting Data to the Spanish Pacemaker Registry in 2016, Grouped by Autonomous Community
| Andalusia |
| Clínica de la Inmaculada |
| Complejo Hospitalario de Jaén |
| Complejo Hospitalario Virgen de la Macarena |
| Hospital Costa del Sol |
| Hospital del Servicio Andaluz de Salud de Jerez de la Frontera |
| Hospital Infanta Elena |
| Hospital Juan Ramón Jiménez |
| Hospital Punta de Europa |
| Aragon |
| Hospital Miguel Servet |
| Hospital Royo Villanova |
| Canary Islands |
| Clínica Quirón |
| Hospital de la Candelaria |
| Hospital Dr. Negrín |
| Hospital Insular |
| Hospital Universitario de Canarias |
| Cantabria |
| Hospital Universitario Marqués de Valdecilla |
| Castile and León |
| Clínica Campogrande |
| Clínica Santa Teresa |
| Complejo Hospitalario de León |
| Hospital Clínico Universitario de Salamanca |
| Hospital Universitario Río Hortega |
| Hospital General de Segovia |
| Hospital General Virgen de la Concha |
| Hospital Nuestra Señora de Sonsoles |
| Hospital Nuestra Señora de Regla |
| Hospital Universitario de Burgos |
| Hospital Universitario de Valladolid |
| Hospital Recoletas de Segovia |
| Castile-La-Mancha |
| Clínica IDC Albacete |
| Clínica La Antigua |
| Hospital General de Ciudad Real |
| Hospital General Virgen de la Luz |
| Hospital General y Universitario de Guadalajara |
| Hospital Virgen de la Salud |
| Catalonia |
| Complejo Hospitalario Parc Taulí |
| Consorcio Sanitario de Mataró |
| Hospital Clínic i Provincial de Barcelona |
| Hospital de Tortosa Virgen de la Cinta |
| Hospital de Lérida Arnau de Vilanova |
| Hospital de Terrassa |
| Hospital del Mar |
| Hospital del Vendrell |
| Hospital Germans Trias i Pujol |
| Hospital Joan XXIII de Tarragona |
| Hospital Mútua de Terrassa |
| Hospital Sant Pau i Santa Tecla |
| Extremadura |
| Hospital Comarcal de Zafra |
| Hospital Comarcal Don Benito-Villanueva |
| Galicia |
| Clínica Quirón |
| Complejo Hospitalario Universitario de A Coruña |
| Compolejo Hospitalario Universitario del Ferrol |
| Hospital Álvaro Cunqueiro |
| Hospital do Meixoeiro |
| Hospital Locus Augusti |
| Hospital Montecelo |
| Hospital San Rafael |
| Balearic Islands |
| Hospital Mateu Orfila |
| Hospital Son Llàtzer |
| Hospital Universitario Son Espases |
| La Rioja |
| Hospital de San Pedro |
| Community of Madrid |
| Clínica La Paloma |
| Clínica Nisa Pardo Aravaca |
| Clínica Nuestra Señora de América |
| Clínica Quirón |
| Clínica Rúber |
| Clínica San Camilo |
| Clínica La Luz |
| Clínica Nuestra Señora del Rosario |
| Fundación Hospital Alcorcón |
| Fundación Jiménez Díaz |
| Hospital 12 de Octubre |
| Hospital de Fuenlabrada |
| Hospital de Móstoles |
| Hospital de Torrejón |
| Hospital del Henares |
| Hospital General Gregorio Marañón |
| Hospital Infanta Leonor |
| Hospital La Paz |
| Hospital Madrid-Montepríncipe |
| Hospital Príncipe de Asturias |
| Hospital Puerta del Sur Móstoles |
| Hospital Ramón y Cajal |
| Hospital San Francisco de Asís |
| Hospital San Rafael |
| Hospital Sanchinarro |
| Hospital Severo Ochoa |
| Hospital Universitario de Getafe |
| Hospital Universitario Puerta de Hierro |
| Hospital Universitario San Carlos |
| Region of Murcia |
| Clínica La Vega |
| Hospital General Santa María del Rosell |
| Hospital Morales Meseguer |
| Hospital Dr. Rafael Méndez |
| Hospital Universitario Virgen de la Arrixaca |
| Chartered Community of Navarre |
| Clínica Universitaria de Navarra |
| Complejo Hospitalario de Navarra |
| Hospital de Navarra |
| Basque Country |
| Hospital de Cruces |
| Hospital Universitario de Araba (Txagorritxu) |
| Principality of Asturias |
| Fundación Hospital de Jove |
| Hospital Central de Asturias |
| Hospital de Cabueñes |
| Valencian Community |
| Clínica de Benidorm |
| Clínica Vista Hermosa |
| Hospital de Sagunto |
| Hospital de Vinalopó |
| Hospital General de Alicante del SVS |
| Hospital General Universitario de Elche |
| Hospital IMED de Elche |
| Hospital Medimart |
| Hospital Perpetuo Socorro |
| Hospital Quirón Torrevieja |
| Hospital Universitari i Politècnic La Fe |
| Hospital Universitario de San Juan de Alicante |
| Hospital Vega Baja |
The percentage of missing data for each parameter varied widely, ranging from 2.5% for the polarity of implanted leads to 60.3% for the etiology of the implant. The following percentages were also missing: preimplantation symptoms, 47.9%; sex, 25.7%; age, 8.3%; type of lead fixation, 30.5%; preimplantation electrocardiogram, 42.1%; reason for generator explantation, 17.8%; and reason for lead explantation, 3.8%. The reported percentages were calculated based on the data available for each parameter after the exclusion of missing data.
Number of Pacemaker Generators ImplantedAccording to data obtained from the Spanish Pacemaker Registry, a total of 12 654 generators were implanted, corresponding to the 115 participating hospitals. According to the information provided by the suppliers, in 2016, 37 990 pacemakers and 1227 CRT-P devices were implanted, forming a total of 39 217 devices. According to Eucomed, 38 086 devices and 1207 CRT-P devices were implanted,18 representing a 1.6% increase compared with the number of devices implanted in 2015.
According to the INE report, as of 1 July, 2016, the Spanish population was 46 468 102 (females, 23 654 467; males, 22 813 635), representing an increase of 45 038 people (0.1%) compared with the population in 2015.17
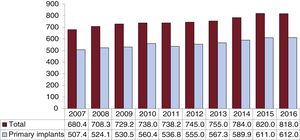
Based on these population data, the Spanish Pacemaker Registry and Eucomed reported an implantation rate of 818 and 820 units/million population (Figure 1), respectively. These figures are significantly lower than the European average (965 units/million population) and those of Germany, Belgium, Finland, and Italy (more than 1000 units/million population), but are higher than those of countries with higher per capita income, such as the United Kingdom, the Netherlands, Norway, and Switzerland (756, 726, 791, and 815 units/million population, respectively).18
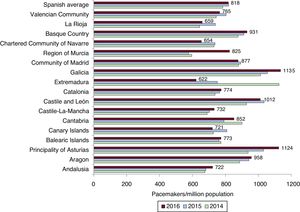
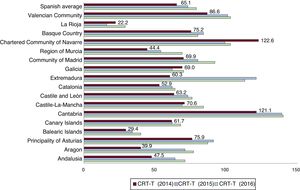
The autonomous communities with the highest implantation rates were Galicia, the Principality of Asturias, and Castile and León, with more than 1000 units/million population, whereas the lowest rates were found in La Rioja, Extremadura, and the Chartered Community of Navarre (less than 700 units/million population) (Figure 2). The implantation rate in the Region of Murcia was notable, with 825 units/million population, representing an increase of 43% compared with that of the previous year.
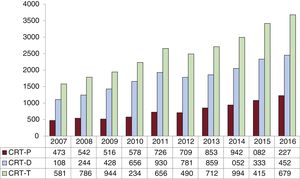
Cardiac Resynchronization DevicesAccording to the Spanish Pacemaker Registry, the total number of CRT (CRT-T) devices implanted in 2016 was 3679 (79 units/million population), a figure similar to that reported by Eucomed (80 units/million population), which represents an increase of 7.7% compared with that of the previous year (Figure 3). The Spanish Pacemaker Registry reported a CRT-P implantation rate of 26 units/million population, which was exactly the same figure as that reported by Eucomed. This rate was one of the lowest in Europe, and was only higher than those reported for Greece and Poland, with 6 and 18 units/million population, respectively. According to the Spanish Pacemaker Registry and Eucomed, the CRT-D implantation rate was 53 and 54 units/million population, respectively. These rates were the lowest in Europe, which has an average rate of 129 units/million population.
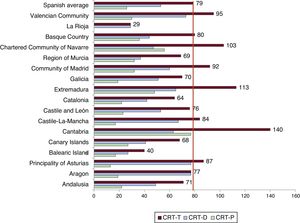
Cantabria, the Chartered Community of Navarre, the Valencian Community, and Extremadura were the autonomous communities with the highest CRT-T implantation rates, with more than 100 units/million population, followed by the Community of Madrid and the Principality of Asturias, with 92 and 87 units/million population, respectively (Figure 4 and Figure 5). La Rioja was the autonomous community with the lowest implantation rate, with 29 units/million population. As in 2015, Cantabria, the Chartered Community of Navarre, and Extremadura had the highest CRT-P implantation rates, with 77, 56, and 48 units/million population, respectively. The Valencian Community and the Principality of Asturias are noteworthy, with more than 70 units/million population.
Pacemaker use was still higher in men than in women (58.2% vs 41.8%), both in primary implants (59.0% vs 41.0%) and in generator exchanges (55.7% vs 44.3%).
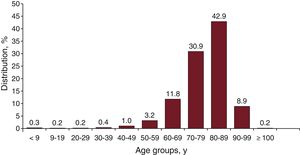
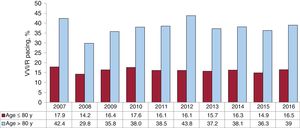
The mean age of all patients undergoing intervention was 77.8 years (78.9 years for exchanges and 77.6 years for primary implants). The mean age of female patients was slightly higher than that of male patients (78.9 years vs 77.6 years). The highest percentage of implants continued to be in the age-range 80 to 89 years (42.9%), followed by 70 to 79 years (30.8%), 60 to 69 years (11.8%), and 90 to 99 years (8.9%). The lowest percentage of implants was in patients younger than 60 years (< 6%). Patients older than 99 years received 0.2% of implants (Figure 6).
Implantations and Generator and Lead ExchangesPrimary implants comprised 74.9% of all procedures in 2016, with 632 primary implants/million population. Of the remaining procedures, generator exchanges comprised 23.4%, generator and lead exchanges 1.4%, and lead exchanges 0.3%.
The most common reason for generator exchange was battery depletion (87.8%), followed by elective exchange (4.1%), reintervention due to the hemodynamic consequences of pacemaker syndrome (1.8%), early depletion due to elevated thresholds, programmed high-output energy, or battery life less than expected (1.2%), malfunction or recall (1.1%), and unspecified causes (<1%). The generator removal rate due to erosion, infection, or protrusion was higher than that of the previous year (3.4% vs 1.4%).
There were 216 lead explantations. The most common reason was infection or ulceration (65.6%), followed by insulation fracture (7.7%), dislodgement (7.7%), and, less commonly, connection failure (3.8%), extracardiac pacing (3.8%), exit blockage (3.8%), or elective exchange (3.8%). The remainder were explanted due to unspecified causes (3.8%).
Pacing LeadsPolarityThe use of bipolar leads was very high, with the same percentage used in the right atrium as in the right ventricle (99.9%). In line with the upward trend in recent years (34.1% in 2014 and 64.3% in 2015), 95.1% of leads implanted in the coronary sinus for left ventricular pacing were bipolar.
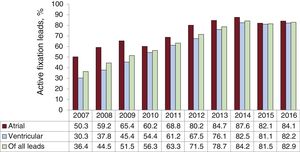
Lead Fixation SystemsMost of the leads used were active fixation leads (82.9%) fitted with retractable helixes allowing their placement in sites other than the apex of the right ventricle and right atrial appendage with a lower risk of dislodgement (Figure 7). Active fixation leads were mainly used in the right atrium (84.1%) and right ventricle (82.2%) and, unlike previous years, the use of active fixation was similar in patients older and younger than 80 years (81.6% and 83.5%, respectively).
Compatibility With Magnetic Resonance ImagingThe Spanish Pacemaker Registry reported 1616 leads compatible with magnetic resonance imaging (MRI), representing 16.1% of all implanted leads, with similar use in the right atrium (15.6%) and right ventricle (16.3%). The use of these leads continued to be lower in patients older than 80 years (12.9%) than in those younger than 80 years (17.5%). The information collected in the EPPIC is insufficient to report the percentage of MRI-compatible generators implanted.
Preimplantation Symptoms, Etiology, and ElectrocardiogramSymptomsThe most common preimplantation symptom was syncope (40.4%), followed by dizziness (24.7%), dyspnea (17.5%), and bradycardia (10.3%). Of the patients implanted with a pacemaker, 3.6% were asymptomatic and were fitted with the device with prophylactic intent. Less common symptoms were tachycardia (1.1%), chest pain (1.0%), cerebral dysfunction (0.4%), recovered sudden cardiac arrest (0.3%), and unspecified causes (0.7%).
EtiologyThe most common reason for implantation was conduction system fibrosis and unknown etiology (81.9%), followed by ischemic etiology (5%; postinfarction, 0.3%), iatrogenic etiology (4%; postablation, 1.1%), cardiomyopathy (3.1%; hypertrophic cardiomyopathy, 0.4%), valvular heart disease (2.4%), congenital heart disease (0.7%), carotid sinus syndrome (6%), vasovagal syndrome (0.2%) and, as rarer causes, myocarditis and heart transplant (< 0.1%). The remainder (1.9%) corresponded to as yet unspecified or coded etiologies.
Preimplantation ElectrocardiogramThe most common electrocardiographic abnormality was atrioventricular block (AVB) (57.5%), comprising third-degree AVB (37.8%), second-degree AVB (13.6%), atrial fibrillation (AF) with complete AVB (4.1%), and first-degree AVB (2.0%) (Figure 8). The second most common electrocardiographic abnormality was sick sinus syndrome (SSS) (31.4%), which included AF with bradycardia (12.9%), bradycardia-tachycardia syndrome (7.2%) and, less commonly, sinus bradycardia (4.9%), unspecified SSS (3.6%), sinus arrhythmia (1.7%), sinoatrial exit block (0.9%), interatrial block (0.1%), and chronotropic incompetence (0.1%). Other reasons for implantation were bundle branch block (5.4%), atrial tachycardia (0.4%), ventricular tachycardia (0.1%), normal sinus rhythm with or without electrophysiological abnormalities (5.1%), and unspecified causes (0.1%).
Regarding sex differences on preimplantation electrocardiogram, AVB was more common in men (55.5% vs 49.2%, excluding blocked AF), followed by blocked AF or AF with bradycardia (17.7% vs 15.5%), and bundle branch block (6.2% vs 3.2%). Sick sinus syndrome (excluding slow AF) was more common in women (25.1% vs 14.8%).
Remote Monitoring/Follow-upIn 2016, there was a significant increase in the use of remote monitoring, involving 4373 pacemakers (11.5% of all implanted pacemakers) and 781 CRT-P devices (65% of all CRT-P devices).
Leadless PacemakersFor the second consecutive year, data were available on leadless pacemaker implantation. In 2016, 200 leadless pacemaker units were implanted. All these units were supplied by a single manufacturer (Micra Model, Medtronic). The mean age of the patients who underwent implantation of this device was 79.9 ± 10.4 years. Compared with the previous year, there was a significant increase (61%) in implantations of leadless devices. Four more autonomous communities have also begun to perform this type of implant. Only 24 of the 200 implanted units have remote monitoring. Taking these figures into account, leadless pacing accounted for 5.3% of all VVI/R devices implanted in 2016.
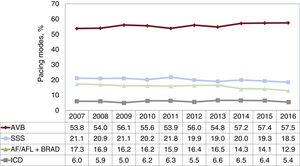
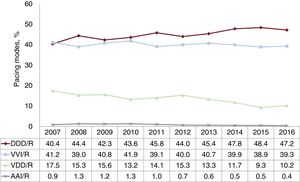
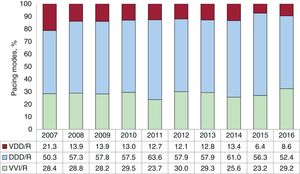
Pacing ModesIn 2016, single-chamber pacing comprised 39.8% of all implanted generators (Figure 9). This percentage included single-chamber atrial pacing (AAI/R) (0.4%), which represented a slight decrease compared with that of 2015. The number of primary implants in AAI/R mode significantly decreased compared with those of the previous year (0.3%) as the number of generator exchanges continued to fall (0.8% of all implants). The use of single-chamber ventricular pacing (VVI/R) underwent a slight increase compared with that of the previous year (39.3% of all implanted generators), mainly due to a slight increase in generator exchanges (39.2%), given that the number of primary implants remained almost identical (39.4%). Taking into account the electrocardiographic diagnosis prior to implantation, with only 7.4% of implants being performed in patients with permanent atrial tachyarrhythmia, an estimated 32% of the patients who received single-chamber ventricular pacing may have received a pacemaker capable of maintaining AV synchrony. However, the final decision on the choice of pacing mode can be affected by several factors, which are discussed in the section on pacing mode selection.
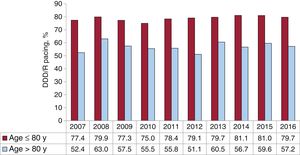
One- or 2-lead dual-chamber sequential pacing comprised 57.3% of all implanted generators. This percentage remained stable compared with that of previous years. Single-lead sequential pacing (VDD/R) was used in 10.2% of all implanted units, representing a slight increase compared with its use in the previous year (Figure 9). The gradual decrease in primary implants and generator exchanges in recent years was followed by a slight increase (8.9% in primary implants and 14% in exchanges). The most commonly used mode was 2-lead dual-chamber pacing (DDD/R) (47.2% of all implanted generators, 48.7% of primary implants, and 42.4% of exchanges) (Figure 9). The use of DDD/R devices fitted with biosensors that allow the pacing frequency to be varied has almost become standard practice (94.3% of all devices).
There was a continued upward trend in the use of biventricular pacing for CRT, both in defibrillator-associated mode and pacemaker-associated mode. In 2016, a total of 1227 CRT-P devices were implanted, representing an increase of 145 units compared with those implanted in 2015 (13.4%; 26 units/million population). In Spain, the use of CRT-P comprised 32.7% of all CRT devices implanted.
Pacing Mode SelectionAtrioventricular BlockTo assess the appropriate use of the most widely recommended pacing modes, this report was limited to patients in sinus rhythm, excluding patients with permanent atrial tachyarrhythmia with AVB (EPPIC code C8). We analyzed possible factors that could have influenced selection, such as patient age, sex, and degree of block.
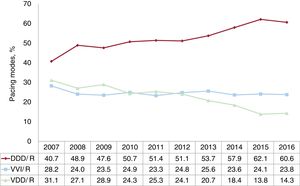
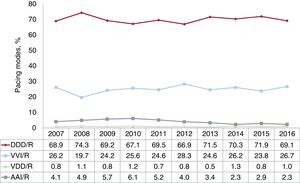
The most commonly used pacing mode was atrial synchronous pacing (DDD/R and VDD/R modes) (74.9%), a percentage that was similar to that of previous years (Figure 10). The use of DDD/R mode (60.6%) and VDD/R mode (14.3%) remained stable. Similarly, the use of VVI/R mode barely changed compared with data from the previous year (23.8%).
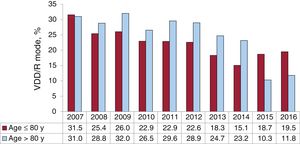
Age continued to influence the choice of pacing mode. In patients aged 80 years or younger, the use of pacing with preserved AV synchrony was clearly in the majority (86.9% of patients), with DDD/R being the most commonly used mode (75.1%). In this age group, DDD/R was the most commonly used mode, while the use of VDD/R mode (11.8%) slightly increased compared with its use in the previous year (Figure 11). In contrast, in patients older than 80 years, there was a significant decrease of pacing with preserved AV synchrony to 61.5%, and there was a slight decrease in single-chamber ventricular pacing to 37.8%, which was a slightly lower percentage than that of the previous year (Figure 12). The VDD/R mode was used more in patients older than 80 years than in younger patients, whereas DDD/R mode was used more in both age groups (19.5% vs 42%) (Figure 11).
Atrial-based pacing was analyzed according to the degree of AVB. This modality was more commonly used in patients with first- or second-degree AVB (77%) than in patients with third-degree AVB (72.6%). These differences were due to the greater use of DDD/R mode in patients with first- and second-degree AVB, a trend that has been observed in recent years. However, these differences were minimal in patients aged 80 years or younger (87.9% in first- or second-degree AVB vs 85.6% in third-degree AVB), whereas they were slightly more pronounced in those older than 80 years (64.3% in first- or second-degree AVB vs 58.1% in third-degree AVB).
As in previous years, there were sex-associated differences in the choice of pacing mode.11–14 The DDD/R pacing was used more often in men, whereas VDD/R pacing was used slightly more often in women. In women aged 80 years or younger, the use of DDD/R mode was still lower than its use in men, as was the case in previous years (72.3% vs 77.5%, respectively), due to the more frequent use of VDD/R mode in women than in men (14% vs 11%) and VVI/R mode (12.3% vs 9.6%). Overall, sequential pacing was used 2.4% less in women aged 80 years or younger and 4.2% less in women older than 80 years than in the equivalent male groups.
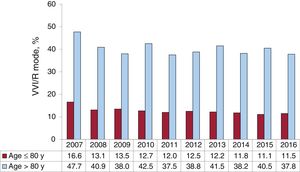
In the setting of an electrocardiographic diagnosis of AVB with preserved sinus rhythm, there continues to be a high percentage of patients who receive single-chamber VVI/R pacing. This pacing mode comprised 23.8% of the total (Figure 10). Its use was marked in the oldest patients (37.8% of those older than 80 years) (Figure 12), and its use was greater in patients with third-degree block and in women from both age groups.
Intraventricular Conduction DisordersIn this group of patients, dual-chamber DDD/R pacing remains the most widely used mode (52.4% of implants), although there has been a slight decrease due to the slight increase in the use of VVI/R (29.2%) and VDD/R (8.6%) (Figure 13). In general, the most commonly used devices were AV synchronous pacemakers (69.8% of all implants), a percentage slightly lower than that of previous years.
The pacing mode in this subgroup of patients was again influenced by patient age, as was the case in patients with AVB. VVI/R pacing was much more common in patients older than 80 years (47.5% of implants) and for the first time exceeded the percentage of DDD/R devices implanted in patients in this age group (35.7%). In contrast, in patients aged 80 years or younger, VVI/R mode was used in only 16.3%, and DDD/R was the most widely used mode (63.6%). VDD/R mode was more frequently used in patients older 80 years than in younger patients (11.2% vs 6.7%).
The implantation of CRT-P devices was much more common (12.9% of implants) in patients younger than 80 years (5.6%).
Sick Sinus SyndromeThe appropriateness of pacing modes according to current recommendations of clinical practice guidelines19,20 was assessed by dividing the patients into 2 large groups. One group comprised patients who were theoretically in atrial fibrillation or flutter with permanent bradycardia or associated bradycardia (EPPIC code E6), and the other group comprised patients who, at least theoretically, remained in sinus rhythm.
- A.
Sick sinus syndrome in permanent atrial tachyarrhythmia, As expected in this situation, most implanted generators were VVI/R (93.6%). However, 4.8% received a DDD/R generator and, as in previous years, 0.3% still received a VDD/R device, which is difficult to justify in SSS. The use of DDD/R mode could be explained in patients who are expected to recover sinus rhythm. A CRT-P device was used in 1.3% of patients. This percentage was more than twice the number of CRT-P implants performed in this setting in the previous year.
- B.
Sick sinus syndrome in sinus rhythm, In the remaining electrocardiographic manifestations of SSS, the predominant rhythm was sinus rhythm, either stable or intermittent. The most commonly used pacing mode continued to be DDD/R (69.1%), as recommended by current clinical practice guidelines, followed by VVI/R (26.7%), AAI/R (2.3%), and VDD/R (1%) (Figure 14). Compared with the percentages reported for the previous year, the use of AAI/R mode decreased slightly and remained very low. This decrease may have been due to increased compliance with the recommendations of the latest clinical practice guidelines published in 2013.19 There was a slight increase in the percentage of patients with VDD/R pacing compared with the previous year. The use of VDD/R mode in SSS continued to be anecdotal, which is also appropriate in relation with the recommendations of the clinical practice guidelines, because this pacing mode is not appropriate in SSS, unless there are other circumstances, such as technical difficulties for the implantation of the atrial lead.
Figure 14.Trends in pacing modes in sick sinus syndrome, 2007 to 2016 (excluding EPPIC code E6; chronic atrial fibrillation and bradycardia). AAI/R, single-chamber atrial pacing; DDD/R, sequential pacing with 2 leads; VDD/R, single-lead sequential pacing; VVI/R, single-chamber ventricular pacing.
(0.19MB).
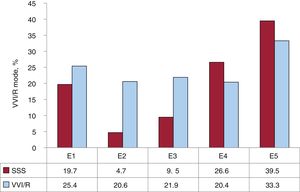
The various electrocardiographic manifestations of SSS were analyzed, excluding EPPIC subgroups E7 and E8 (interatrial block and chronotropic incompetence), due to their minimal representation over the years. The percentage of VVI/R pacing ranged from 20.4% to 33.3%; once again, the highest percentage corresponded to bradycardia-tachycardia syndrome (EPPIC subgroup E5) (Figure 15). However, these percentages may have been inflated due to the erroneous inclusion of patients with permanent AF with slow-fast episodes in group E5 rather than in group E6 mentioned above.
Distribution of VVI/R, according to the codes established in the European Pacemaker Patient Identification Card in SSS. E1, unspecified sick sinus syndrome; E2, exit block; E3, sinoatrial arrest; E4, bradycardia; E5, bradycardia-tachycardia syndrome; SSS, sick sinus syndrome; VVI/R, single-chamber ventricular pacing.
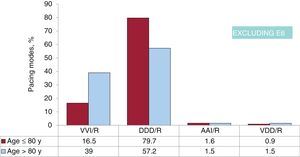
As was the case in AVB, age continued to influence pacing mode selection in SSS. In patients aged 80 years or younger, there was more frequent use of pacing modes that enable sensing and pacing in the atrium, that is, AAI/R and DDD/R (1.6% and 79.7%, respectively), compared with just 16.5% in VVI/R mode (Figure 16 and Figure 17). However, in patients older than 80 years, VVI/R mode (39% vs 57.2% DDD/R and 1.5% AAI/R) was used much more frequently (Figure 16 and figure 17). These figures are consistent with those obtained in recent years. VDD/R mode was little used in both age ranges (0.9% and 1.5%), although these percentages were slightly greater than those of the previous year (Figure 16). Age was shown to be a factor influencing pacing mode selection over the years studied (Figure 17 and Figure 18).
Pacing modes in sick sinus syndrome by age (cutoff point at 80 years). AAI/R, single- chamber pacing; E6, chronic atrial fibrillation and bradycardia; DDD/R, sequential pacing with 2 leads; SSS, sick sinus syndrome; VDD/R, single-lead sequential pacing; VVI/R, single-chamber ventricular pacing.
The influence of sex on pacing mode selection was analyzed. In contrast to previous years, it is noteworthy that in patients older than 80 years, VVI/R mode was used 13.2% more in women than in the men. However, in patients aged 80 years or younger, VVI/R mode was used much less and with very similar percentages in both sexes (16.2% in men vs 15.4% in women).
DISCUSSIONThe EPPIC remains the primary source of information submitted to the Spanish Pacemaker Registry. This information was provided by just 115 implantation centers and there was variation in the amount of information completed on each patient card. Although this information can be considered representative of cardiac pacing activity in Spain, the quality of data collection should be improved to obtain a more reliable account of the different aspects of pacing in Spain. We believe that this improvement can be achieved by the implementation of the online application and its widespread use in the implantation centers.
The total use of pacemaker generators in Spain, including CRT-P devices, slightly increased (1.6%) compared with 2015, although this change was less marked than that between 2015 and 2014 (5%). This increase was due to the use of CRT-P devices, which increased by 13.4%, whereas the number of conventional pacemaker generators remained almost the same as that of the previous year. In fact, despite the slight increase in the population, there was a slight decrease in the implantation rate (818 units/million population), breaking the upward trend of recent years. Despite the gradual economic recovery taking place in Spain, it continues to be among the European countries with the lowest rate of pacemaker implantations per million population. The real causes of this low implant rate are unknown, but it is probably influenced by factors other than economics, because countries such as the United Kingdom, the Netherlands, Norway, and Switzerland, with higher per capita income, have a lower implant rate than that of Spain. Other causes may be the lack of training programs and human and material resources, indications not in accordance with clinical guidelines, or health centers with few referral units (arrhythmia and heart failure units).
The number of CRT-T devices increased by 7.7% compared with 2015 (7 units/million population), with a higher increase in the number of CRT-P devices (13.4%) than of CRT-D devices (5.1%). The CRT-D/CRT-P ratio was 2:1 (53:26 units/million population). Despite the above-mentioned increase, the number of units implanted in Spain remains below the European average of the 18 countries reporting their data to Eucomed (mean CRT-P and CRT-D, 48 and 129 units/million population, respectively).
Regarding autonomous communities, the Principality of Asturias, Galicia, and Castile and León implanted the most pacemakers, with more than 1000 units/million population, whereas communities such as the Chartered Community of Navarre, Cantabria, and Extremadura implanted more CRT-P devices, with more than 40 units/million population. In the Region of Murcia, there has been a marked increase in the rate of conventional pacemaker implants (from 576 to 825 units/million population) and CRT-P implants (from 18 to 32 units/million population). Factors that could influence the different implant rates between autonomous communities include differences in the age of the population, economic management, health structure, and the availability of arrhythmia and heart failure units, with consequent differences in the rates for patient referral for implantation.
As in previous years, there was a higher percentage of primary implants and exchanges in men (58.2%). Just over half of implants (52%) are performed in patients older than 80 years.
The most common electrocardiographic abnormality prior to implantation was AVB (57.5%), including second- and third-degree AVB (51.4%), SSS (18.5%), blocked AF or AF with bradycardia (17.0%). Bundle branch block (5.4%) was the least common indication.
Most implanted leads were bipolar, both in the right atrium and right ventricle, and also, following the trend described above, in the coronary sinus (95.1% in 2016). The information submitted to the Spanish Pacemaker Registry does not include the use of quadripolar left ventricular pacing leads through the coronary sinus. This technique makes it possible to choose, among multiple electronic configurations, the one with the best electrical behavior and without phrenic pacing. Neither is information available on the use of multipoint pacing in cardiac resynchronization, which is a novel therapy with initial benefits in acute hemodynamics and left ventricular asynchrony, with medium-term clinical benefit.21 Most leads were for active fixation systems (82.9%), both in the atrium and ventricle. Unlike previous years, a similar percentage was used in patients older or younger than 80 years, probably because of their demonstrated benefit in stability, alternative implant sites, optimal electrical behavior, and low complication rates. The use of MRI-compatible leads was still low (16.1%). This percentage may be due to the low implant rate of MRI-compatible generators (although these data are not included in EPPIC), which are high-end devices with higher costs. The use of these leads was even lower in older patients (12.9% in patients older than 80 years). Because of the progressive population aging and the increasing use of MRI, it is advisable to greatly increase the use of systems compatible with this radiological technique.
Of note was the growing application of home monitoring systems, with a significant increase compared with that of previous years (from 5% to 20% in conventional pacemakers and from 15.9% to 65% in CRT-P devices). This is a clearly positive trend, as it is a safe, cost-effective strategy that enables the early detection and response to events.
For the second consecutive year, the Spanish Pacemaker Registry included data on leadless pacemaker implantation. During 2016, the number of such devices implanted (200) was twice that of the previous year.15 The number of autonomous communities implanting these devices also increased from 9 to 13. Although the cost of these pacemakers continues to be higher than that of a conventional VVI/R pacemaker, the long-term benefits of the absence of cables in the vascular space, the increased availability of this technology, and the scientific evidence corroborating its effectiveness and mid-term safety may explain the progressive increase in the number of implants.22,23
As in previous years, the most common preoperative electrocardiographic abnormality was AVB (mainly third-degree AVB). In AVB, the most frequently used pacing mode continued to be atrial synchronous pacing (74.9%). The use of DDD/R pacing slightly decreased compared with that of the previous year (60.6%), and it is noteworthy that the use of VVI/R and VDD/R mode remained stable (23.8% and 14.8%, respectively). In AVB, age continued to be a determining factor in pacing-mode selection. Most patients aged 80 years or younger with AVB received DDD/R pacing, whereas in those older than 80 years the percentage of single-chamber pacing continued to be high, although it slightly decreased compared with the previous year (37.8%). Pacing in VDD/R mode to maintain AV synchrony was used more frequently in patients older than 80 years than in the younger group (19.5% vs 11.8%) and its use slightly increased slightly compared with that of the previous year.
In SSS, atrial-based pacing continued to be the most commonly used mode, with a predominance of DDD/R mode (69.1%), as recommended by current clinical practice guidelines. However, VVI/R mode continued to be used in 26.7% of SSS patients, representing a change in the downward trend observed in recent years. In SSS, age also continued to influence pacing-mode selection. Single-chamber VVI/R pacing was more common in patients older than 80 years (39%) and in bradycardia-tachycardia syndrome (53.5%), possibly due to the risk of going into permanent AF in the near future or because of the erroneous inclusion of patients with permanent slow-fast AF in this group. The current guidelines recommend pacing with DDD/R mode in SSS, mainly because it decreases the incidence of AF and stroke and lowers the risk of pacemaker syndrome, which can adversely affect patients’ quality of life. Pacing in AAI/R mode continued to decrease, probably due to increased compliance with the current clinical practice guidelines based on the results of the DANPACE study,24 and to the disadvantages of this pacing mode (0.6% to 1.9% of patients with SSS develop AVB each year). In atrial tachyarrhythmia with slow ventricular response, VVI/R pacing was the most commonly used mode.
In intraventricular conduction defects, DDD/R (52.4%) was the most frequently used mode, followed by VVI/R (29.2%). In patients older than 80 years, for the first time, VVI/R mode was used more often than DDD/R mode (47.5% vs 35.7%). In contrast, most patients aged 80 years or younger received DDD/R pacing, although the percentage of single-chamber pacing doubled compared with that of the previous year (16.3%). VDD/R mode was used less frequently, and its deployment in patients older than 80 years was twice that of the younger age group. Low-energy CRT pacing continued to be relevant in this patient subgroup (9.6% of implants), but its use decreased compared with that of the previous year. In patients with intraventricular conduction defects, age was once again an important factor in the use of CRT-P (≤ 80 years, 12.9%; > 80 years, 5.6%).
CONCLUSIONSThe use of conventional pacemakers and CRT-P has continued to increase, although the average number of such implantations remains below that of other European countries. Age was the main factor affecting the choice of pacing mode, which was inappropriate in up to 20% of patients with AVB and SSS. Leadless pacing has become established, and its use significantly increased in 2016 with a greater number of implantation centers. There was a significant increase in the percentage of remote monitoring devices.
CONFLICTS OF INTERESTNone declared.