This report describes the cardiac pacing activity performed in Spain in 2020, including the number and type of implanted devices, demographic and clinical factors, and data on remote monitoring.
MethodsInformation consisted of the European Pacemaker Patient Card, data submitted to the cardiodispositivos.es online platform, the databases of participating centers, and supplier-reported data.
ResultsA total of 14 662 procedures were registered from 102 hospitals, representing 39.2% of the estimated activity. The implantation rates of conventional and low-energy resynchronization pacemakers were 759 and 31 units per million population, respectively. In all, 520 leadless pacemakers were implanted, 70 with atrioventricular synchrony. The mean age at implantation was high (78.8 years), and the most frequent electrocardiographic change was atrioventricular block. There was a predominance of dual-chamber pacing mode but VVI/R single-chamber pacing was used in 19% of patients in sinus rhythm, depending on age and sex. Remote monitoring capability was present in 18.5% of implanted conventional pacemakers and 45.6% of low-energy resynchronization pacemakers, although registration in this system increased by 53% in 2020.
ConclusionsIn 2020, in the context of the SARS-CoV-2 pandemic, the number of implanted conventional pacemakers decreased by 8% and cardiac resynchronization therapy by 4.6%. The number of leadless pacemakers increased by 16.5%. Sequential pacing was predominant, influenced by age and sex. Home monitoring played a fundamental role as a mode of follow-up in this SARS-CoV-2 pandemic year.
Keywords
The present report, drafted by the Cardiac Pacing Section of the Spanish Society of Cardiology (SEC), contains the cardiac pacing activity corresponding to Spain in 2020, previously collected in the Spanish National Pacemaker Data Bank. This document includes overall data on devices implanted and compares the data with those of previous years1–9 and those provided by our neighboring countries.10 Clinical and demographic data are also collected on the individuals receiving these devices.
The health care crisis triggered by the SARS-CoV-2 pandemic has had a major impact on cardiac pacing activity, as on all health care fields, particularly on the device implantation rate and the preferential selection of remote monitoring as follow-up.
METHODSThe information sources used were the European Pacemaker Patient Identification Card (EPPIC), sent to the Spanish National Pacemaker Data Bank, the information submitted to the online platform CardioDispositivos.es,11 and the proprietary databases of some of the centers.
Population statistics were obtained from the Spanish National Institute of Statistics on March 22, 2021, and refer to the population of Spain as of July 1, 2020.12
Given that the information provided by the implanting centers is still scarce, the total implantation figures were based on the data provided by the device manufacturers and checked against those provided by the European Confederation of Medical Suppliers Association (Eucomed).10
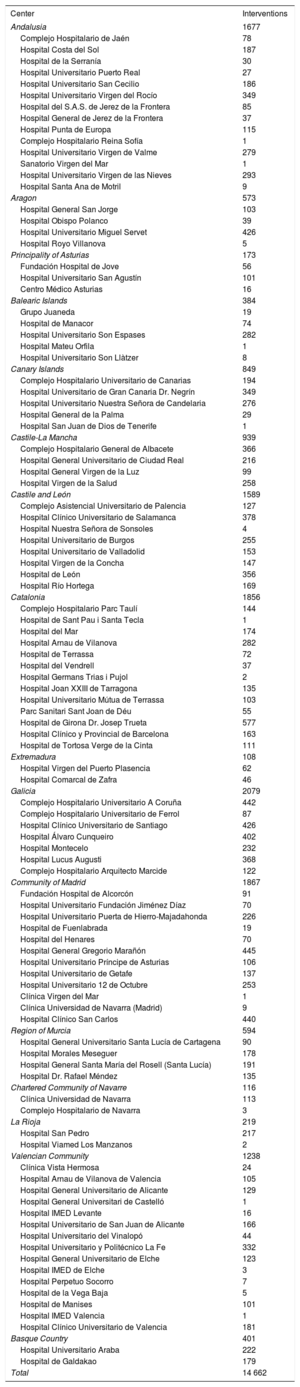
RESULTSSample qualityIn 2020, 14 662 procedures were recorded in 102 hospitals (table 1), 6040 obtained via the CardioDispositivos.es platform and 8622 from the EPPICs or proprietary databases.
Public and private hospitals submitting data to the Spanish Pacemaker Registry in 2020, grouped by autonomous community and with the numbers of interventions performed in each center.
| Center | Interventions |
|---|---|
| Andalusia | 1677 |
| Complejo Hospitalario de Jaén | 78 |
| Hospital Costa del Sol | 187 |
| Hospital de la Serranía | 30 |
| Hospital Universitario Puerto Real | 27 |
| Hospital Universitario San Cecilio | 186 |
| Hospital Universitario Virgen del Rocío | 349 |
| Hospital del S.A.S. de Jerez de la Frontera | 85 |
| Hospital General de Jerez de la Frontera | 37 |
| Hospital Punta de Europa | 115 |
| Complejo Hospitalario Reina Sofía | 1 |
| Hospital Universitario Virgen de Valme | 279 |
| Sanatorio Virgen del Mar | 1 |
| Hospital Universitario Virgen de las Nieves | 293 |
| Hospital Santa Ana de Motril | 9 |
| Aragon | 573 |
| Hospital General San Jorge | 103 |
| Hospital Obispo Polanco | 39 |
| Hospital Universitario Miguel Servet | 426 |
| Hospital Royo Villanova | 5 |
| Principality of Asturias | 173 |
| Fundación Hospital de Jove | 56 |
| Hospital Universitario San Agustín | 101 |
| Centro Médico Asturias | 16 |
| Balearic Islands | 384 |
| Grupo Juaneda | 19 |
| Hospital de Manacor | 74 |
| Hospital Universitario Son Espases | 282 |
| Hospital Mateu Orfila | 1 |
| Hospital Universitario Son Llàtzer | 8 |
| Canary Islands | 849 |
| Complejo Hospitalario Universitario de Canarias | 194 |
| Hospital Universitario de Gran Canaria Dr. Negrín | 349 |
| Hospital Universitario Nuestra Señora de Candelaria | 276 |
| Hospital General de la Palma | 29 |
| Hospital San Juan de Dios de Tenerife | 1 |
| Castile-La Mancha | 939 |
| Complejo Hospitalario General de Albacete | 366 |
| Hospital General Universitario de Ciudad Real | 216 |
| Hospital General Virgen de la Luz | 99 |
| Hospital Virgen de la Salud | 258 |
| Castile and León | 1589 |
| Complejo Asistencial Universitario de Palencia | 127 |
| Hospital Clínico Universitario de Salamanca | 378 |
| Hospital Nuestra Señora de Sonsoles | 4 |
| Hospital Universitario de Burgos | 255 |
| Hospital Universitario de Valladolid | 153 |
| Hospital Virgen de la Concha | 147 |
| Hospital de León | 356 |
| Hospital Río Hortega | 169 |
| Catalonia | 1856 |
| Complejo Hospitalario Parc Taulí | 144 |
| Hospital de Sant Pau i Santa Tecla | 1 |
| Hospital del Mar | 174 |
| Hospital Arnau de Vilanova | 282 |
| Hospital de Terrassa | 72 |
| Hospital del Vendrell | 37 |
| Hospital Germans Trias i Pujol | 2 |
| Hospital Joan XXIII de Tarragona | 135 |
| Hospital Universitario Mútua de Terrassa | 103 |
| Parc Sanitari Sant Joan de Déu | 55 |
| Hospital de Girona Dr. Josep Trueta | 577 |
| Hospital Clínico y Provincial de Barcelona | 163 |
| Hospital de Tortosa Verge de la Cinta | 111 |
| Extremadura | 108 |
| Hospital Virgen del Puerto Plasencia | 62 |
| Hospital Comarcal de Zafra | 46 |
| Galicia | 2079 |
| Complejo Hospitalario Universitario A Coruña | 442 |
| Complejo Hospitalario Universitario de Ferrol | 87 |
| Hospital Clínico Universitario de Santiago | 426 |
| Hospital Álvaro Cunqueiro | 402 |
| Hospital Montecelo | 232 |
| Hospital Lucus Augusti | 368 |
| Complejo Hospitalario Arquitecto Marcide | 122 |
| Community of Madrid | 1867 |
| Fundación Hospital de Alcorcón | 91 |
| Hospital Universitario Fundación Jiménez Díaz | 70 |
| Hospital Universitario Puerta de Hierro-Majadahonda | 226 |
| Hospital de Fuenlabrada | 19 |
| Hospital del Henares | 70 |
| Hospital General Gregorio Marañón | 445 |
| Hospital Universitario Príncipe de Asturias | 106 |
| Hospital Universitario de Getafe | 137 |
| Hospital Universitario 12 de Octubre | 253 |
| Clínica Virgen del Mar | 1 |
| Clínica Universidad de Navarra (Madrid) | 9 |
| Hospital Clínico San Carlos | 440 |
| Region of Murcia | 594 |
| Hospital General Universitario Santa Lucía de Cartagena | 90 |
| Hospital Morales Meseguer | 178 |
| Hospital General Santa María del Rosell (Santa Lucía) | 191 |
| Hospital Dr. Rafael Méndez | 135 |
| Chartered Community of Navarre | 116 |
| Clínica Universidad de Navarra | 113 |
| Complejo Hospitalario de Navarra | 3 |
| La Rioja | 219 |
| Hospital San Pedro | 217 |
| Hospital Viamed Los Manzanos | 2 |
| Valencian Community | 1238 |
| Clínica Vista Hermosa | 24 |
| Hospital Arnau de Vilanova de Valencia | 105 |
| Hospital General Universitario de Alicante | 129 |
| Hospital General Universitari de Castelló | 1 |
| Hospital IMED Levante | 16 |
| Hospital Universitario de San Juan de Alicante | 166 |
| Hospital Universitario del Vinalopó | 44 |
| Hospital Universitario y Politécnico La Fe | 332 |
| Hospital General Universitario de Elche | 123 |
| Hospital IMED de Elche | 3 |
| Hospital Perpetuo Socorro | 7 |
| Hospital de la Vega Baja | 5 |
| Hospital de Manises | 101 |
| Hospital IMED Valencia | 1 |
| Hospital Clínico Universitario de Valencia | 181 |
| Basque Country | 401 |
| Hospital Universitario Araba | 222 |
| Hospital de Galdakao | 179 |
| Total | 14 662 |
Because the EPPICs and the online platform forms are not always fully completed, some data were missing on all parameters analyzed: 7.2% on pacing mode, 14% on lead position, 13.1% on age, 18% on sex, 25.9% on lead polarity, 24% on type of lead fixation, 49.1% on the preimplantation electrocardiogram, 55.2% on symptoms, 67.2% on etiology, 68.9% on reason for generator explantation, and 84.1% on reason for lead explantation. The results reported here were based on the available data, after exclusion of missing information.
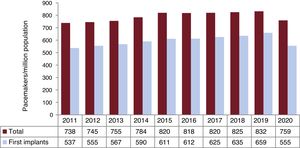
Numbers of conventional pacemakersAccording to Spanish Pacemaker Registry data, 35 926 conventional pacemakers were implanted in Spain in 2020, representing a rate of 759 units/million population (figure 1). However, according to Eucomed, the pacemaker implantation rate was 766 units/million in Spain in 2020.
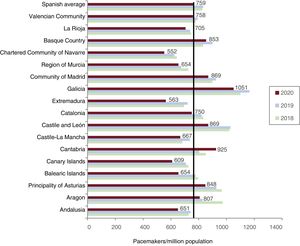
Regarding the distribution by autonomous community, Galicia and Cantabria stood out with 1051 and 925 units/million population, respectively, as well as Castile and León and Madrid with 869 units/million (figure 2); the autonomous communities with the lowest rates were the Canary Islands, Extremadura, and Navarre with 609, 563, and 552 units/million, respectively.
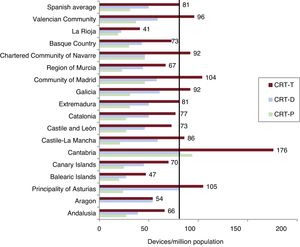
Cardiac resynchronization devicesAccording to the Spanish Pacemaker Registry, 3850 total cardiac resynchronization therapy (CRT-T) devices were implanted in Spain in 2020, comprising 1463 cardiac resynchronization therapy without defibrillation (CRT-P) devices and 2387 cardiac resynchronization therapy with defibrillation (CRT-D) devices. The CRT-T device rate was 81 units/million population, whereas that of CRT-P devices was 31 units/million, which was the same figure as that reported by Eucomed.
For CRT-T devices, Cantabria stood out with 176 units/million population, followed at quite a distance by Asturias and the Community of Madrid with 105 and 104 units/million, respectively. Regarding CRT-P devices, Cantabria was once again top of the list with 94 units/million population, followed by the Community of Madrid and Navarre with 46 units/million. La Rioja had the lowest number of CRT-T devices with 19 units/million population, whereas Aragon implanted 0 CRT-P devices (figure 3).
Cardiac resynchronization therapy devices per million population in 2020 (national average and by autonomous community). CRT-D, cardiac resynchronization therapy with defibrillation; CRT-P, cardiac resynchronization therapy without defibrillation; CRT-T, total cardiac resynchronization therapy.
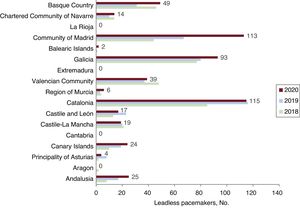
In 2020, 520 Micra (Medtronic, United States) model leadless pacemakers were implanted, 70 with the ability to maintain atrioventricular (AV) synchrony. Catalonia and Madrid continued to be the autonomous communities with the highest number of such implants (115 and 113 units), followed by Galicia with 93; these 3 provinces represented 61.7% of leadless pacemakers implanted. Aragon, Cantabria, Extremadura, and La Rioja did not implant any pacemakers of this type (figure 4).
Age and sexPacemaker implantation was much more frequent in men (59.3% of devices vs 40.7% in women), both for first implants (60.1% vs 39.9%) and replacements (57.2% vs 42.7%).
The average age of pacemaker recipients was 78.8 years. It was slightly higher in women than in men (80.2 vs 77.8 years) and for replacements vs first implants (80.7 vs 78.2 years). Just 1.7% of devices were implanted in individuals younger than 50 years, as well as 2.8% in those 50 to 59 years, 10.7% in those 60 to 69 years, 30.6% in those 70 to 79 years, 42.5% in those 80 to 89 years, 11.6% in those 90 to 99 years, and 0.1% in those older than 100 years.
Etiology and symptoms prompting implantationConduction system fibrosis continued to be the predominant etiology (85.4% of implants). The other etiologies were infrequent: ischemia (2.9%), infarction (0.6%), iatrogenic due to surgery (3.5%), ablation (0.9%), TAVI (1.1%), carotid sinus syndrome (0.4%), vasovagal syncope (0.4%), congenital heart disease (0.7%), unspecified cardiomyopathy (0.6%), hypertrophic cardiomyopathy (0.5%), dilated cardiomyopathy (1%), endocarditis/myocarditis (0.1%), heart transplant (0.1%), and valvular heart disease (1.8%).
Syncope was the symptom most frequently prompting implantation (41.8% of cases), followed by dizziness (25.1%) and heart failure (14.6%).
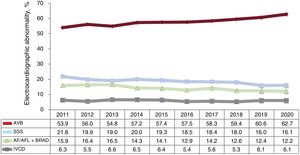
Preimplantation electrocardiogramAtrioventricular block (AVB) was the most frequent preimplantation electrocardiographic abnormality (62.7% of cases). Third-degree AVB predominated (40.1%), followed by second-degree (14.7%) and first-degree (1.3%). Atrial fibrillation (AF) with complete heart block was seen in 6.6% of preimplantation electrocardiograms. AVB was followed by sick sinus syndrome (SSS) (28.3% of cases). Sinus bradycardia/sinus pauses prompted 6.2% of implants, followed by bradycardia-tachycardia syndrome (5.9%) and, with lower frequency, sinoatrial block/pause (1.9%). Other abnormalities such as chronotropic incompetence and interatrial block represented less than 1% of implants. The SSS subtype was unspecified in 1.8% of implants. Slow AF was present in 12.2% of preimplantation electrocardiograms and an intraventricular conduction defect was found in 6.1% (figure 5).
Regarding the distribution by sex, AVB was more frequent in men than in women (57.5% vs 53.8%, excluding blocked AF), whereas SSS was more frequent in women (21.9% vs 9.7%, excluding slow AF). Slow or blocked AF prompted 19.2% of implants in men and 16.4% of those in women. Intraventricular conduction defect was practically twice as common in men as in women (8.0% vs 4.2%).
Type of procedureOf procedures, 73.1% were first implants and 25.3% were exclusively generator replacements. Generator and lead replacements represented 2.1% of cases, whereas lead replacement alone comprised 0.5%. The most frequent reason for generator replacement continued to be end-of-life battery depletion (73.9%), followed by elective replacement (18.4%), pacemaker syndrome (1.5%), infection/erosion (2.7%), premature depletion (1%), dysfunction (0.7%), advisories (0.7%), and other unspecified causes.
In the case of lead explantation, the most frequent cause was infection/ulceration (45.9%), followed by displacement (19.7%), insulation failure or conduit rupture (18.1%), dysfunction (6.5%), perforation (1.6%), and other unspecified causes (8.2%).
Electrode typeActive-fixation leads represented 89.6% of leads, with similar rates for the right atrium and ventricle (90.4% and 90.9%, respectively), as well as 22.1% of coronary sinus leads. Most leads were bipolar (98.5%; 99.6% in the right atrium and 99.3% in the right ventricle). In addition, 65.4% of coronary sinus leads were tetrapolar, according to CardioDispositivos.es data.11
Magnetic resonance imaging-compatible leads comprised 82.1% of leads, with a slightly higher rate for patients ≤ 80 years than in those > 80 years (83.2% vs 80.3%) and in the right atrium than in the right ventricle (85.5% vs 81.4%), according to data submitted to the CardioDispositivos.es platform, the most reliable information source for this parameter.11
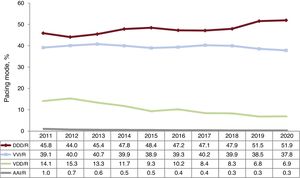
Pacing modesSequential dual-chamber pacing with 2 leads (DDD/R) continued to be the most commonly used pacing mode in 2020 (51.9% of all procedures, 55% of first implants, and 43.4% of pacemaker replacements), in line with the upward trend of recent years. In contrast, the use of VDD pacemakers broke the previously recorded downtrend trend and stabilized at 6.9% of procedures (4.3% of first implants and 14% of replacements).
Single-chamber pacing was used in 37.8% of all procedures, vs 38.5% in 2019, largely due to single-chamber ventricular pacing (VVI/R) (37.5% of all interventions). Single-chamber atrial pacing (AAI/R) continued to be negligible in Spain, with 36 reported procedures (0.3%); just 18 were first implants (figure 6).
Still underused, although becoming more common, biventricular CRT-P pacing represented 3.1% of all implants (2.7% with atrial leads vs 0.4% with biventricular pacing alone).
Compared with men, women received more single-chamber VVI/R pacing (39.7% vs 36.5% of procedures) and VDD pacing (8.5% vs 6.4% of procedures reported) but less dual-chamber pacing DDD/R pacing (49.8% vs 53.3%).
Pacing mode selectionAtrioventricular blockThis section excludes patients with AVB and permanent atrial tachyarrhythmia (EPPIC code C8) to properly assess the degree of adherence to the most recommended pacing modes in the clinical practice guidelines. Factors possibly influencing this selection were analyzed, such as patients’ age and sex and the degree of AVB.
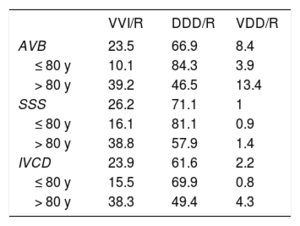
Pacing capable of maintaining AV synchrony increased again, accounting for 76.5% of cases, and DDD/R mode was the most commonly used mode (66.9% of implants); VDD/R mode comprised 8.4%. A notable finding was the negligible use of CRT-P therapy with atrial pacing for this conduction disorder, at 1.2% of implants (figure 7).
Age and sex continued to determine whether AV synchrony will be maintained. In patients ≤ 80 years, pacemakers capable of maintaining AV synchrony were used in 89.8% of cases, vs 60.5% of cases in patients > 80. VDD implantation continued to fall in patients ≤ 80 years and represented 3.9% of cases in 2020 vs 5.3% in 2019; however, it was still frequent in those > 80 years (13.4%). Regarding sex, the differences seen in previous years decreased, although men were more likely to benefit from sequential pacing, which maintains AV synchrony. Thus, 78.6% of men received this pacing mode, with DDD/R mode documented in 69.9% of EPPICs reported. In women, pacing capable of maintaining AV synchrony represented 72.1% of cases and VDD pacing was more common than in men (11.3% vs 7.1%). Nonetheless, this difference was magnified by the disparity in reported procedures because there were more men ≤ 80 years. When these differences were analyzed by age, men ≤ 80 years used sequential AV pacing (DDD/R, VDD/R, or CRT-P) in 90.7% of cases vs 88.8% in women. For those > 80 years, these pacing types were used in 61.7% of men and in 60.4% of women (table 2).
Distribution (%) of pacing modes by electrocardiographic abnormality and age group in 2020.
| VVI/R | DDD/R | VDD/R | |
|---|---|---|---|
| AVB | 23.5 | 66.9 | 8.4 |
| ≤ 80 y | 10.1 | 84.3 | 3.9 |
| > 80 y | 39.2 | 46.5 | 13.4 |
| SSS | 26.2 | 71.1 | 1 |
| ≤ 80 y | 16.1 | 81.1 | 0.9 |
| > 80 y | 38.8 | 57.9 | 1.4 |
| IVCD | 23.9 | 61.6 | 2.2 |
| ≤ 80 y | 15.5 | 69.9 | 0.8 |
| > 80 y | 38.3 | 49.4 | 4.3 |
AVB, atrioventricular block; DDD/R, sequential pacing with 2 leads; IVCD, intraventricular conduction defect; SSS, sick sinus syndrome; VDD/R, single-lead sequential pacing; VVI/R, single-chamber ventricular pacing.
Regarding pacing mode, no major changes were seen vs previous years, with pacemakers capable of maintaining AV synchrony implanted in 81.5% of patients with first- or second-degree AVB and in 74.4% of patients with complete AVB. By age, this pacing mode was much less frequent in patients > 80 years. This was particularly evident for those with complete AVB, with rates of 59.1% in men and 59.6% in women. It was used in 15.9% of women and 12.7% of men in this age group and with this indication (complete AVB), which is considered more amenable to VDD pacing.
Single-chamber ventricular pacemaker implantation (VVI/R) for the treatment of AVB in patients with preserved sinus rhythm fell again, representing 23.5% of procedures. The use of this pacing mode continued to be prominent in patients > 80 years (39.5% of cases, a slight drop vs the 40.2% of cases in 2019).
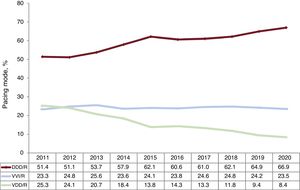
Intraventricular conduction defectsPacemakers capable of maintaining AV synchrony continued to be the most commonly used device (75.7% of procedures), largely due to DDD/R (61.6%); 11.4% were triple-chamber CRT-P pacemakers. VDD and single-chamber VVI/R pacing fell again to 2.2% and 23.9% of cases, respectively.
The most commonly used mode continued to be DDD/R in both individuals ≤ 80 years (69.9%) and those > 80 years (49.4%). In patients > 80 years, 38.3% of patients received a VVI/R pacemaker vs 15.5% of those ≤ 80 years, breaking the downward trend of recent years. In addition, the fall in VDD pacemaker implants continued (2.2% of all pacemakers), with 4.3% in patients > 80 years vs 0.9% in patients ≤ 80 (table 2).
Regarding CRT-P devices, there was a decrease from previous years, with 12.3% of implants vs 15.7% in 2019; 8% were in patients > 80 years vs 13.8% in those ≤ 80 years.
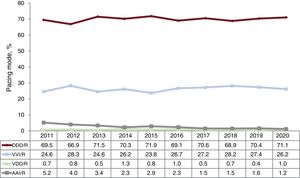
Sick sinus syndromeAs usual, patients with SSS were divided between those who theoretically were in permanent AF or atrial flutter and had bradycardia and those who were in sinus rhythm. In this way, the aim was to evaluate the adherence of the pacing modes to the current recommendations in the clinical practice guidelines.13,14
1. Sick sinus syndrome in permanent atrial tachyarrhythmia. VVI/R pacing predominated (92.2% of all implants). A DDD/R system was used in 6.23% and biventricular pacing in 1.4%; the implantation of other pacing types was negligible. There were no major differences by age, except in the use of DDD/R pacemakers, which were used in 4.4% of patients > 80 years and in 9.1% of those ≤ 80 years. We assume that this pacing mode was used because an at least partial return to sinus rhythm was expected in many of the patients.
2.Sick sinus syndrome in sinus rhythm. Adherence to clinical practice guideline recommendations is gradually improving, with increases in the pacing modes permitting atrial pacing and AV synchrony maintenance. Accordingly, DDD/R pacemakers were implanted in 71.1% of cases and VVI/R in 26.2%. The reported data showed the low uptake of AAI/R pacing, with only 13 patients (1.2% of the total with this indication); the other pacing modes—biventricular and VDD/R—were rare (figure 8).
The electrocardiographic manifestation is key when the device is being chosen in SSS patients. Thus, VVI/R pacemaker implantation may be inflated by the erroneous inclusion of patients with AF or permanent atrial tachyarrhythmia in subgroup E2 of the EPPIC (bradycardia-tachycardia syndrome). Moreover, 59.3% of single-chamber pacemakers implanted in SSS were indicated for bradycardia-tachycardia syndrome.
Analysis of the SSS data in patients in sinus rhythm by age and sex revealed the presence of differences in the devices used, with a higher frequency of dual-chamber pacing in younger patients and in men. In patients ≤ 80 years, DDD/R pacing comprised 81.6%; AAI/R comprised 0.7% and VVI/R mode just 16.1%. In patients > 80 years, VVI/R pacing represented 38.8% of cases, although 56.8% of these had bradycardia-tachycardia syndrome (table 2). Women more commonly received single-chamber VVI/R pacing than men (28.5% vs 23.2%), particularly those ≤ 80 years, in whom VVI/R pacing comprised 18.7% of cases in women vs 14.3% of those in men.
Remote monitoringIn 2020, 6637 conventional pacemakers were included in a remote monitoring program, as well as 1854 CRT-D devices and 668 CRT-P devices (18.5%, 77.7%, and 45.7% of all devices implanted). By autonomous community, La Rioja stood out with 68.2% of all devices included, followed by Aragon, Murcia, the Canary Islands, Navarre, and the Basque Country, with figures around 50%. Notable for their low implementation were Cantabria and the Balearic Islands (2.9% and 4.1% of devices included).
In addition, in this pandemic year, remote monitoring systems were provided to individuals with devices implanted in previous years that were subject to face-to-face follow-up, specifically to 3174 patients with conventional pacemakers, 170 with CRT-D devices, and 93 with CRT-P devices. This represents a 53% increase, with a total of 12 596 devices included vs 8241 in 2019.
DISCUSSIONThe sample obtained in 2020 represented 39% of the activity reported by the device manufacturers, similar to previous years. Notably, more data were submitted through CardioDispositivos.es,11 with 6040 procedures included (41% of all procedures reported) and a 35% increase vs 2019. Once again, we must stress the importance of data submission via this platform11 as a way to obtain high-quality information, as well as its value as an optimal monitoring system for medical devices in the cardiac pacing field.
The SARS-CoV-2 pandemic of 2020 led to major changes in social, economic, and particularly health care circumstances worldwide, which necessitated major alterations to the activity conducted in both hospitals and primary care centers. During the first wave, hospitals were forced to limit all nonessential medical acts and to maintain emergency procedures alone, which also affected cardiac pacing activity. Salgado-Aranda et al.15 described this activity reduction, specifically a drop of 35.2% in the number of urgent/preferential pacemakers in the period from March 15 to May 15, 2020, vs the same period in 2019. This reduction was particularly due to a lower frequency of implants vs the previous year in asymptomatic patients or those with mild symptoms and with AVB as the most frequent cause of implants based on proportion. Factors possibly contributing to this fall in nonurgent activity included competing risk, with higher COVID-19-related impact and mortality in the candidate population for pacemaker implantation, lower physical activity during lockdown, with a lower frequency of symptoms, lower probability of early diagnosis due to the closure of nonessential activity, and patients’ fear of being infected in the hospital setting.15
In this context, the number of conventional pacemakers implanted in 2020 decreased by 8% vs 2019, which broke the upward trend and led to the lowest rate of the last 5 years, with 766 units/million population according to the data provided by Eucomed. This figure is lower than the European average (899 units/million population), which also suffered a major decrease vs 2019 (963 units/million), probably also due to the pandemic. Germany and Finland stand out regarding implantation rates, as well as Denmark, which also exceeded 1000 units/million population in 2020.
The number of CRT-T devices also fell by 4.6%, with reductions of 3.7% in CRT-P devices and of 5.1% in CRT-D devices. As in 2019, the CRT-D/CRT-P ratio was once again 1.6. CRT-P devices represented 38% of CRT-T devices and Spain continued to have one of the lowest rates in Europe, whose average is 57 units/million population; only Poland and Greece (with 24 and 11 units/million population, respectively10) have lower rates than Spain (31 units/million).
Leadless pacemaker implantation is gradually increasing year on year, with a 16.5% increase vs 2019. In 2020, data were included on leadless pacemakers capable of maintaining AV synchrony, a device that represents a notable advance in the development of this technology and whose initial results are highly promising.16 Once again, the data showed a highly heterogeneous distribution in terms of implantation activity by autonomous community: Madrid, Catalonia, and Galicia implanted the highest number of leadless devices, whereas other communities did not implant any devices of this type. A major increase in leadless pacemaker use is likely in the coming years due to the advantages of this device in settings such as a lack of superior venous access routes (due to occlusion or venous system abnormalities), previous device infection, or high infection risk (for various reasons, such as diabetes mellitus, chronic kidney disease, central lines, cardiac prostheses, or immunosuppression), as well as in very old patients,17 particularly those with dementia at risk of lead displacement. Its low current implementation and irregular distribution among autonomous communities are probably due to economic factors.
In 2020, we also received data specifically submitted through the online platform11 on the magnetic resonance imaging compatibility of the implanted leads (a more reliable source in this aspect), with the results indicating greater use of this type of lead (82.1%). These data are crucial, given the ever growing use of this radiological technique. No reliable data were available on the physiological pacing carried out in 2020 in Spain because these data are not recorded in the EPPICs, which are still the information source for preparing this report. The Task Force of the Cardiac Pacing Section of the SEC has begun a registry to record this activity, which will prove vital for the present and future development of pacing.18
Regarding pacing modes, AVB maintained the trend seen in recent years for atrial-based pacing, which comprised 76.5% of cases in 2020 vs 74.3% in 2019; DDD/R mode predominated (66.9% of procedures). In patients > 80 years, single-chamber VVI/R pacing was more widespread, with abandonment of atrial pacing/sensing in up to 39.5% of cases. This result confirmed that age is one of the main factors determining the selection of pacing mode. In this age group and for this conduction disorder, VDD reached its peak implementation (13.4% of patients with these characteristics). Other parameters such as frailty, cognitive decline, or dependency possibly explain the less strict adherence to clinical practice guideline recommendations because, although increased mortality has not been linked to single-chamber pacing vs dual-chamber pacing in AVB, the former pacing mode has been associated with a decreased functional class and the onset of AF or pacemaker syndrome.
Despite the 2020 COVID-19 pandemic, which could have led to a simplification of procedures and greater use of VVI/R or VDD pacemakers, we actually saw increased use of DDD/R pacing, which allows atrial pacing, and a progressive fall in VDD pacemakers, which are now used in less than 5% of first implants for this indication. The coming years may show a stabilization or even an increase in this pacing mode, after the development of atrial-sensing algorithms for leadless pacemakers.
A notable finding in intraventricular conduction defects was the apparent decrease in biventricular pacing, which dropped from 15.7% in 2019 to 12.3% in 2020 (predominantly with atrial lead), and the slight uptick in single-chamber VVI/R pacing, from 21.8% in 2019 to 23.9% in 2020. Although the exact reasons are unknown, it is highly probably that this pattern is related to the increased and widespread use of conduction system pacing techniques, exemplified by bundle of His and left branch pacing, with a shift from biventricular CRT-P pacing devices to conventional DDD/R or VVI/R pacemakers.
In patients with permanent atrial tachyarrhythmia (mainly AF or atrial flutter), as would be expected, single-chamber VVI/R devices continued to dominate (92.1% of patients). Pacemakers capable of stimulating the atrium increased again in patients with SSS. Conventional DDD/R pacing was used in 71.1% of patients, very similar to previous years, and the limited implantation of AAI/R devices, very residual in Spain, comprised more than 1% of interventions. The guidelines recommend DDD/R mode in SSS because of its ability to reduce the incidence of AF, strokes, and pacemaker syndrome. VVI/R mode was used in 26.2% of cases (38.8% in patients > 80 years), and this high percentage is probably because, within SSS, patients with permanent AF are erroneously diagnosed with bradycardia-tachycardia syndrome; the appropriate pacing mode for such patients is VVI/R.
In this pandemic year, remote monitoring gained importance as a crucial follow-up mode for devices, due to its particular ability to avoid or reduce face-to-face visits at times of high infection risk without compromising safety.19 Discharges with home-based monitoring systems increased by 53% in 2020, which is particularly noteworthy because the use of such systems not only increased for devices implanted in 2020, but also for those implanted in previous years. This increment was largely due to the 69% jump in inclusions of conventional pacemakers in remote monitoring programs, a striking figure given that this type of follow-up has always been less common in this type of device than in CRT-D and CRT-P devices. The use of this follow-up system was mainly driven by the need for a restructuring of health care activity during the pandemic. We hope that this trend continues due to the clinical advantages and safety of this approach. As noted in the de-escalation document published after the first wave of the pandemic, the Cardiac Pacing Section of the SEC is opting for device follow-up largely based on an organized and well-structured remote monitoring program.20
CONCLUSIONSIn 2020, in the context of the SARS-CoV-2 pandemic, falls were recorded of 8% in the implantation rate of conventional pacemakers and of 4.6% in that of cardiac resynchronization devices, whereas the inclusion significantly increased of devices in remote monitoring programs. The number of leadless pacemakers jumped, including that of the new device with AV synchrony capability. Atrial-based pacing predominated, particularly in the younger population. Greater use of the CardioDispositivos.es platform will boost data quality.
FUNDINGFor the maintenance and collection of the data included in the present registry, the SEC has been supported by a grant from the Spanish Agency of Medicines and Medical Devices (AEMPS), the proprietor of these data.
AUTHORS’ CONTRIBUTIONSJ. Chimeno drafted the section on pacing modes; V. Bertomeu prepared the section on remote monitoring; Ó. Cano reported the information related to the conventional pacemaker and cardiac resynchronization therapy data; and M. Pombo prepared the clinical and demographic data and coordinated the work.
CONFLICTS OF INTERESTNone.