Keywords
One of the aims of the Cardiac Stimulation Department is to collect and analyse pacing data from Spain, so the Spanish Pacemaker Registry, National Pacemaker Database1 was created for this purpose. The register holds information about the most relevant characteristics of cardiac stimulation and its development since 1994. This continually updated information allows us to understand the truth about the clinical practice and the diverse aspects of the quality of the stimulation carried out annually so as to compare it with our own activities or with other records or with information from other countries.
Since the publication2 of the first official report in the Revista Española de Cardiología in 1997, this has been published periodically.3-7 The current report presents data which correspond with cardiac stimulation by pacemakers during 2007.
Detailed information dating back to 1999, which is updated and distributed annually, is freely available on the Cardiac Stimulation Department's Website: www.marcapasossec.org; www.estimulacioncardiaca.org.
METHODS
The data and information used are taken from the various sections of the European Pacemaker Patient Identification Card.2 This information is voluntarily sent to the registry in electronic format or paper format by those responsible for the registry in each centre (each centre's database is included and compliant with relevant security measures as laid out in Data Protection Regulations). The card has a carbon copy which is sent to the registry directly from the hospital units where the implant was carried out or from the various companies involved, as required by the current legislation on inserting devices.3
The data is studied by 2 nurses with extensive experience in the field of cardiac stimulation, both of whom are regular collaborators with the registry. They process the information from the Spanish Cardiology Society using a special software programme. Under the management of Dr Jesús de Juan Mondiel, the Cardiac Stimulation Unit has developed its own database in an attempt to unify and facilitate data collection. To date it has not been significantly successful. We believe that above all, this is due to the effort of changing the routine achieved with current databases which are already adjusted to the particular needs and local networks of the different hospitals.
The total number of pacemakers used in a year, both on a national scale and a regional scale, has been gleaned from data supplied to the National Spanish Pacemaker Database (BNDM) by the various supply companies in Spain. The information is also submitted to Eucomed (European Confederation of Medical Suppliers Associations).
The national and regional population data for the various calculations for each year are extracted from the report periodically updated and distributed by the National Institute of Statistics (INE) (www.ine.es).
The analysis was carried out on the total information supplied in each section of the card.
A general extract of the procedure was also submitted to contribute to the European Pacemaker Registry8 which holds comparative information of various European countries which also submit their data. In 2007, 114 private and public hospitals submitted data.
RESULTS
Number of Pacemakers Implanted per Million Inhabitants
In 2007 a total of 30 284 general pacemakers were implanted or replaced and 473 cardiac pacing devices were implanted for cardiac resynchronization therapy (CRT) without defibrillation, according to the data provided by the various BNDM industries. According to information supplied by the Spanish Statistics Institute (INE), the population census recorded 45.2 million inhabitants.
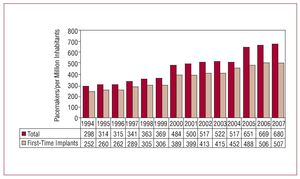
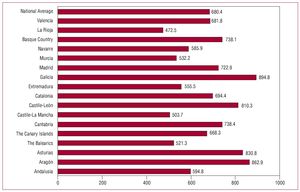
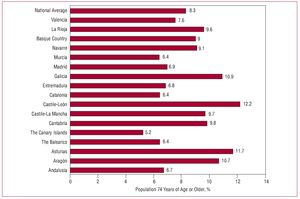
The number of pacemakers used per million inhabitants was 680.4 (Figure 1) and 10.4 CRT devices were used. Analysing distribution across the different autonomous communities and according to the number of inhabitants as recorded for 2007 by the INE, noticeable differences were seen in the number of implants per million inhabitants, the most significant differences were seen in Galicia, Castilla y León, Aragón, and Asturias in which more than 800 pacemakers were fitted per 1 million inhabitants (Figure 2). These communities have an older population which is reflected in the average age for implant as submitted to the BNDM, and in the percentage of the population who were over the age of 75 according to INE data. For example, the population over the age of 75 is 12.2% in Castilla y León, 11.7% in Asturias, 10.9% in Galicia, 10.7% in Aragón, 6.7% in Andalusia, 6.4% in Catalonia and the Balearics, 5.2% in the Canary Islands, etc (Figure 3). This variation in the number of implants was also noted in 2006, the other year analysed with similar data.
Figure 1. Number of pacemakers and first-time implants per million inhabitants, 1994-2007
Figure 2. Pacemakers implanted per million inhabitants, national average, and autonomous community average, 2007.
Figure 3. Percentage of the population 74 years of age or older, national average, and distribution over autonomous community, 2007.
Samples Analysed. Participating Centres
Data have been submitted by 114 participating hospitals, which are listed in the appendixes and grouped per Spanish Autonomous Community (Appendix 1). A total of 11360 cards were submitted corresponding both to pacemaker implants and replacements. This figure constitutes 36.9% of the total units used that year, which is an increase in both the number of units and percentage of the estimated total with regard to previous years, but it is still far off the ideal 100%. However, it is a very representative sample and will allow us to understand the diverse aspects of cardiac pacing carried out in Spain. The results described below correspond to the analysis of said sample.
Age and Gender of the Population
Age
The average age of patients receiving a pacemaker implant for the first time in 2007 was 76.1. There is a slight difference in this average with regard to gender; lower in males than in females (75.4 and 77.1 respectively). This difference of almost 2 years remains about the same in each year analysed since data became available. The average age of patients receiving a replacement pacemaker is almost the same as for the first time implants: 76.3 years. A continuous increase in the average age is seen as the population experiences higher longevity.3-7
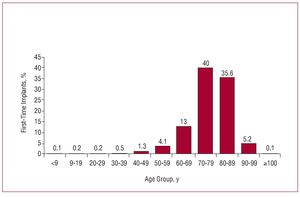
The age group with the highest number of implants includes people in their seventies, making up 40% of the total; this is followed by those in their eighties with 35.6% (Figure 4). With regard to replacement implants, the highest figures were seen in the population in their eighties (37.2%) followed by those in their seventies (36.1%). Although only a token figure (0.1%), some replacements and implants have been carried out in patients 100 years old and above.
Figure 4. First-time implants, distribution by age group, 2007.
Gender
As with previous years,7 more implants were carried out in males (58%) than in females, despite the number of women in the population being higher (22.3 million men and 22.8 million women, according to INE data). This higher incidence is seen both in the first-time implants (57.9%) and in replacements (58.4%) and across all the different age groups.
Type of Procedure. First-Time Implant and Pacemaker Replacement
Seventy-four point six percent of patients were to have a pacemaker fitted for the first time. The tendency of a decrease in first-time implants in comparison with the number of replacements was 25.4%, with the exception of 2006.7 The replacement procedures which also required the substitution or addition of a new electrode lead constituted 1.8% of the total procedures registered.
The most frequent causes for explant or generator replacement were the battery running out (88.9%). Cases of the battery running out prematurely constituted 1%. Other causes were as follows: infection (2%), deterioration of the pouch (0.9%), change of system for haemodynamic improvement (1.6%), change of system for pacemaker syndrome (0.4%), and generator defects (0.4%) (0.3% were minor and 0.1% major).
Electrode Cables: Polarity and Attachment System of the Implanted Leads. Explant or Exchange of the Electrode Lead
The pacing leads used were mainly all bipolar (99.6%). In the atrial position these were almost the only pacing methods employed with 99.9% of leads implanted in this cavity. Sixty percent of the leads implanted through the coronary sinus for pacing of the left ventricle were bipolar.
With regards the distribution of the small percentage of single leads (0.4% of the total), most of them were electrode leads designed specifically for implant through the coronary sinus (65%) for epicardial stimulation of the left ventricle (for CRT or to solve access issues of the implant to the right ventricle as can happen in the presence of a mechanical prosthesis, tricuspid atresia, severe tricuspid valvular insufficiency, etc). Another 10.9% of the single leads were epicardial leads, implanted at the same time as cardiac surgery or specifically used for problems relating to infections such as endocarditis where the preference is not to use intravascular prosthetic material. The others are implanted in the right ventricle (21.7%).
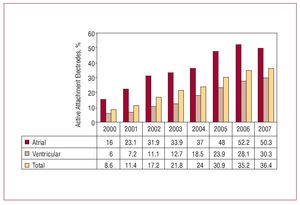
The attachment system used for the electrode leads to achieve stability in the endocardium is usually passive via the use of elastic tabs (63.5% of cases). However, active attachment is carried out using a helix or spiral (usually retractable) and its use is gradually increasing and constitutes 36.4% of all electrode leads. Its application is increasing for reasons such as pacing in non-conventional areas, or the ease of explant, where necessary. Pacing in alternative areas, other than the right ventricular apex, continues to increase due to the possible decrease in deterioration of ventricular function and the ease of implant in the septal area of patients with large cavity dilation and severe tricuspid insufficiencies. In the atrial cavity, placement somewhere other than the usual atrial appendage, such as in the lower or upper atrial septum, tends to be indicated for the potential decrease of atrial arrhythmias, above all when there is high intra-atrial conduction disorder. Active attachment is essential for stabilising the lead when the location of the implant is not trabeculated as is the case in the para-Hisian areas or the sinus node. The active attachment system was used in 50.3% of atrial placement and 30.3% of ventricular placement (Figure 5).
Figure 5. Active attachment electrodes with regard to the total and the implants in the atrial and ventricular cavity. Details from 2002-2007.
The implant of a new electrode-lead for the pacing system constituted 2% of all the procedures registered in 2007. Said procedures correspond in part to 1.8% of those in which generator replacement was carried out at the same time as electrode replacement to improve the pacing method, or it was chosen due to deterioration of pacing resistances or thresholds of the lead or due to the lesion of this lead during the generator replacement procedure. Intervention for replacement of the cardiac pacing leads due to alterations in their function constituted 0.2% of all the interventions carried out.
The causes or reasons that have been pointed out as indications for replacement or explant of the electrode lead were, in order of frequency; infection or ulceration (35.9%), breakage of the lead insulator (15.3%), strain/displacement (7.6%), breakage of the conductor (5.1%), connection defects (5.1%), incorrect choices (5%), and exit blocks (2.5%).
Symptoms
The symptoms or clinical expression for the alterations originating from the pacemaker implant were, in order of frequency: syncope (43.5%), presyncope (28.1%), dyspnoea or signs of cardiac insufficiency (13.2%), and bradycardia (10%). The implants in patients who were asymptomatic or had prophylactic implants were (2.5%); chest pain and cerebral dysfunction (0.7% each), and sudden death due to bradyarrhythmia 0.2%.
Aetiology
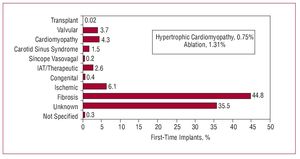
Amongst the etiological reasons submitted as indications for implants, fibrosis of the conduction system continues to be the most frequent (44.8%), followed by unknown aetiology (35.5%). The group of iatrogenic therapeutic causes remain almost identical to the previous year7 (2.6%) and ablation of the atrioventricular node is at 1.3%.
In the myocardial group, obstructive hypertrophy was present in 0.7% of the indications. Other causes can be seen in the graph (Figure 6).
Figure 6. Aetiology of stimulation by pacemaker in first-time implant, 2007. IAT/therapeutic indicates iatrogenic or therapeutic.
Electrocardiographic Alterations
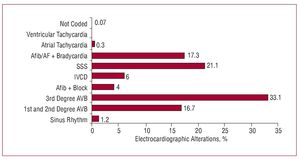
Conduction disorders were the electrocardiographic alteration which most frequently led to implant indication. Of these, atrioventricular block (AV block) was the most common (53.8%), including those with atrial fibrillation. In the data from previous years this has always been the predominant alteration with figures close to 50%.7 The intraventricular conduction disorders (IVCD) made up 6% of the electrocardiographic alterations and over time have remained between 5% and 6%.
Sick sinus syndrome (SSS), in its various manifestations (sinoatrial block, sinus arrest, tachycardia-bradycardia syndrome, sinus bradycardia), constituted 21.1% and if we include atrial fibrillation/flutter or bradycardia (Afib/AF) (group E6), this totals 38.4%. Details of the subgroups can be found in Figure 7.
Figure 7. Distribution of the pre-implant electrocardiographic alterations in 2007. AV block indicates atrioventricular block; Afib, atrial fibrillation; Afib/AF + bradycardia, atrial fibrillation / atrial flutter with slow ventricular response; IVCD, intraventricular conduction disorder.
With regard to gender, it is important to note that as has been the case over the last 5 years, the incidence of conduction disorders, both AV and IVCD is much more frequent in men. However, SSS is similar in both sexes (numerical relationship of male/women, 1.37 AVB; 2.17 IVCD; 1.09 SSS). The deterioration or degeneration of the conduction system as a reason for pacemaker implant is higher in males than females.
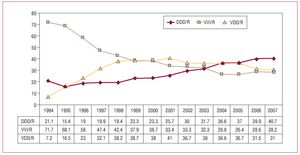
Pacing Methods
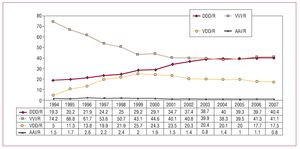
Considering the total number of pacemakers used over the year, isolated atrial pacing (AAI/R) does not constitute any more than 0.8% of all the generators used, and the percentage is much more similar both in the group of first-time implants (0.8%) and the replacement group (0.9%), which indicates low usage, even in previous years.
VVI/R constituted 41.1% of the pacing methods used, and there were no major variations between first-time implants and replacements (41.2% and 41% respectively). Given that with electrocardiographic alterations the percentage of patients who had a pacemaker fitted and were in permanent atrial tachyarrhythmia (Afib/AF) were only 21.3% (combination of Afib/AF with bradycardia [17.3%] and Afib/AF with AV block [4%]), there is a significant group of patients who used the VVI/R method despite normal sinus rhythm. The distribution of these patients over the different groups in accordance with electrocardiographic alteration prior to implant are analysed in the following sections. The influence of age on the group for this method of pacing in patients with normal sinus rhythm is also possible.
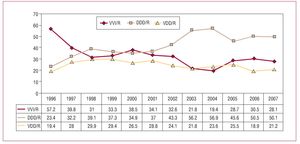
Sequential stimulation, whether it is with 2 electrodes, atrial or ventricular, DDD/R, or single lead with atrial floating rings or VDD/R pacing; totalled 57.9%. VDD/R pacing (17.5% of the total units used) remained stable over the last 2 years. However, there is marked difference in this VDD/R method when we analyse the group of first-time implants (16.4%) in comparison with replacements (20.5%), which is an indication of the decrease in use of this model in comparison with previous years. The details from the different years studied can be seen in Figure 8.
Figure 8. General information of the evolution of the pacing methods, 1994-2007.
The possibility of variation in the frequency of pacing due to some kind of biosensor (accelerometer, ventilator rate, etc) was associated with 79.6% of cases.
The use of pacing for cardiac resynchronisation therapy with no defibrillation, which is the aim of our analysis, saw an increase in 2006 compared to the previous year7 (474 units in 2006 and 407 in 2005), and has stabilised in 2007 (473 units), but this implies a slight proportional slip in total pacemakers (1.5%). However, the units associated with defibrillation continue to increase and in 2007 they reached 1108 units (848 in 2006). From the information submitted to the registry, we understand that biventricular units make up 1.2% of first-time implants and 1.7% of generator replacements (due to the implant of more up to date units or simply because the battery ran out).
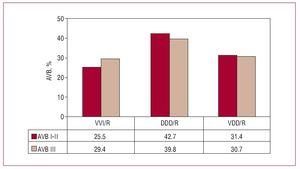
AV Block Stimulation
For the analysis of this group, the C8 subgroup coded on the European Pacemaker Patient Identification Card corresponding to patients in atrial fibrillation and patients with AV block, was excluded. Therefore it can be seen that in patients who had a pacemaker implanted due to AV block with normal sinus rhythm, pacing is based on atrial synchronisation in 71.7% of cases. This percentage is higher for patients with first and second degree AV block (74.5%) than in those with third degree AV block (70.6%). Of these, 40.7% correspond to the DDD/R method and the rest to VDD/R (31%) pacing. The details of the methods according to the various degrees of AV block can be seen in Figure 9. In the general data collected over the years a slow decline in the use of VDD/R pacing is noted (its highest rate of use was in 2001 when it was the most used AV block method), and it is mainly due to the change to DDD/R pacing.7
Figure 9. Pacing types in 1st, 2nd, and 3rd degree atrioventricular block (AV block), 2007.
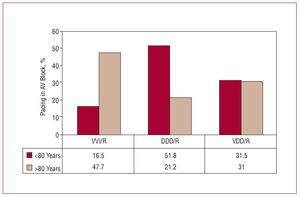
It should be pointed out that if we consider the types of pacing used separating patients into age groups of 80 years old or more and the under eighties, the percentage of application of VDD/R pacing was the same in both groups (31%). This was not the case with DDD/R pacing which was 51.8% in the younger group and only 21.2% in the older group.
There is still a high percentage of VVI/R pacing in patients with AV block with normal sinus rhythm (28.2% of the total) a method which alters from the that which is most recommended for this type of electrocardiographic alteration,9-11 and it has only slightly decreased in relation to 2006 (Figure 10). This percentage is somewhat less for the patient group with a certain level of AV conduction. In patients with first and second degree AV block it was 25.5% compared with 29.4% for third degree AV block (Figure 9). In the choice of VVI/R pacing, age continues to play an important factor as in the group of 80 year olds and above it reaches 47.7% whilst in the younger age group the figure is 16.5% (Figure 11).
Figure 10. Development of pacing methods used in AV block, excluding patients with fibrillation or permanent atrial flutter, 1994-2007.
Figure 11. Pacing methods used in AV block, in accordance with 2 age groups 80 years old or more and under 80, excluding the patients in permanent atrial fibrillation.
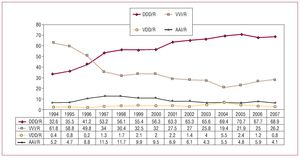
Pacing in Sick Sinus Syndrome
As with previous reports, the study of this group is done in 2 sections, the E6 group from European Pacemaker Patient Identification Card (patients with Afib/AF with brachycardia) and the E1-E8 group with electrocardiographic alterations of SSS, in which in theory, sinus rhythm is maintained and therefore interference is avoided which can be caused by assessing the ideal suitability of the selection of pacing methods in this group.
In the subgroup of patients with permanent atrial arrhythmia (Afib/AF), although it would be hoped that they would all use the VVI/R method, and this is the case in the majority of cases (93.8%), DDD/R was the choice in 5.5% of cases. This is understood to correspond to patients who were expected to revert to normal sinus rhythm a second time. Less explicable is the low percentage (0.4%) that used the VDD/R method. This can only be justified by technical reasons or unsuitability of choice of method.
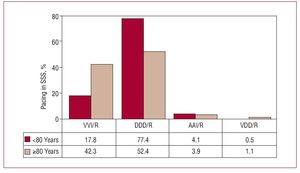
In the rest of the subgroups of SSS (excluding the previous ones who had atrial tachyarrhythmia), the recommendations from the current clinical guidelines9-11 for the type of pacing method to be used are for atrial based pacing units (with pacing ability and detection of atrial activity). Pacing in 2007 was mainly carried out with the DDD/R method (69%) and the AAI/R method constituted 4.1%. Seventy-three point one percent used the most advised method. Isolated single chamber atrial pacing was at the lowest percentage of all the years in 1994, based on data from the BNDM and this was possibly due to the gradual introduction of the units with new algorithms with the capability of changing the pacing method from AAIR to DDD/R (Figure 12).
Figure 12. Pacing methods used in sick sinus syndrome, excluding patients with permanent atrial tachyarrhythmia, 1994-2007.
As with previous years, VVI/R has remained almost the same with just a slight increase which constitutes 26.2% of this subgroup. The VDD/R group which is not very suitable for this type of disorder is still used in a small number of cases but it is decreasing and represents 0.8% (Figure 12). In general these 2 pacing methods with little justification can entail some symptoms, such as pacemaker syndrome, due to persistent retrograde conduction and also it can increase the incidence of atrial fibrillation.
If, as on previous occasions, we analyse the possible influence of patient age on the suitability and selection of the method and we compare with the groups of under and over eighties, a marked difference can be seen in the usage and selection of the methods. The DDD/R method is used in 77.4% of the under eighties group and 52% in the over eighties group, and the single chamber ventricular pacing stood at 17.8% in comparison with 42.3%. The use of the AAI/R method is similar in both age groups. This therefore shows that in a significant proportion of the population, a certain deviation from the most recommended pacing method is occurring,9-11 above all in older patients as is the case in previous years (Figure 13).
Figure 13. Pacing methods in sick sinus syndrome (SSS) by 2 age groups, 2007.
Pacing in Intraventricular Conduction Disorders
The pacing method most frequently used was DDD/R (50.1%) which was similar to the previous year. VDD/R pacing reached 21.2%. Both constitute a total of 71.3% of the methods which maintain AV synchronisation. The single chamber ventricular VVI/R pacing was 28.1%. The use of the VVI/R methods in this group of electrocardiographic alterations in some cases can be justified by pacing only being required in very isolated occasions, and it is only used as a safety measure and for prevention of symptoms, basically in patients with syncope in which other causes have been ruled out and they have AV conduction. The percentage of use of the VVI/R method has seen a certain decline and has remained at levels similar to those from 2005 which is a change from the tendency to increase over the 2 previous years7 (Figure 14).
Figure 14. Pacing methods in intraventricular conduction disorders, year 2007, and evolution.
The devices used for CRT in dilated cardiomyopathy associated with intraventricular conduction disorder made up 10% of the pacemakers implanted for IVCD and reached 12.7% in the under eighty patient group and 6.2% in the older age group.
In other pacing methods differences are also seen with regard to the analysis of the 2 age groups mentioned; as such the DDD method is the most used in the under eighties group (56.5%), in comparison with 39.3% in the 80 and above age group. The VVI/R method is the most frequently used in the over 80 age group (37.5%), in comparison with 22% in the under eighties age group. The use of the VDD/R method was almost the same in both age groups (21.3% in the first group and 22.1% in the second).
CONCLUSIONS
An increase can be seen in the number of pacemakers used per million inhabitants, rising to 680 in 2007, and a notable variation in the number of units implanted per million inhabitants across the different autonomous communities. We believe the unequal aging of the population across these regions is largely influential in this increase.
The replacement of generators constitutes 25.3% of the procedures carried out.
The average age of a patient receiving their first pacemaker is 76.1 years of age and as in previous years it is seen that this age is somewhat lower in males than in females. There is a higher frequency of implants in men due to them having a higher incidence of conduction disorders.
Almost all of the endocardial leads used are bipolar and 60% of coronary sinus leads are bipolar. There continues to be an increase in the acceptance of leads which use an active attachment method (36.4% of the total). There is no variation by age group with regards the choice of attachment method.
Age continues to be a determining factor in the selection and suitability of the pacing method seeing a movement from DDD/R to VVI/R in all the electrocardiographic groups studied (SSS, AV block, IVCD). This is not the case with VDD/R in AV block or IVCD, or A AI/R in SSS, in those which have similar pacing percentages.
In the overall total of the pacemakers, the single lead VDD/R method constituted 17.5% of the units implanted; more than 30% of the AV block used this pacing method which means that Spain is one of the countries with the highest use of this pacing method. The number of pacing devices remains stable for non-fibrillation CRT, but there is a slight decrease in the overall percentage of units and the number of units per million inhabitants.
The number of hospitals supplying their data is continuously increasing (114 currently) and they cover 37% of generators implanted, though this is far off 100%.
ACKNOWLEDGEMENTS
To the nursing graduates Pilar González Pérez and Brígida Martínez Noriega and to Gonzalo Justes Toha, information technician from SEC. Without their dedication and collaboration the maintenance and usage of the pacemaker database would not have been possible.
To all the experts, doctors and nurses from the hospitals who collaborated with the Registry in the completion and submission of the European Pacemaker Patient Identification Cards.
To the personnel of the various pacemaker industries in Spain (Biotronik, Boston, Medico, Medtonic-Viatron, Saint Jude, and Sorin Group) for their continuous collaboration both in the submission of the cards and in providing the necessary information to calculate the units used each year.
ABBREVIATIONS
Afib/AF: atrial fibrillation / atrial flutter
AVB: atrioventricular block
BNDM: National Spanish Pacemaker Database
CRT: cardiac resynchronization therapy
INE: National Institute of Statistics
IVCD: intraventricular conduction disorder
SSS: sick sinus syndrome
Correspondence: Dr. R. Coma Samartín. Arturo Soria, 184. 28043 Madrid. España.
E-mail: coma@vitanet.nu