We describe the results of the analysis of the devices implanted and conveyed to the Spanish Pacemaker Registry in 2015.
MethodsThe report is based on the processing of information provided by the European Pacemaker Patient Identification Card.
ResultsWe received information from 111 hospitals, with a total of 12 555 cards, representing 32.1% of all the estimated activity. The use of conventional generators and resynchronization devices was 820 and 73 units per million population, respectively. The mean age of the patients receiving an implantation was 77.7 years, and more than 50% of the devices were implanted in patients over 80 years of age. Overall, 58.6% of the implants and 58.8% of the replacements were performed in men. All of the endocardial leads employed were bipolar, 81.5% had an active fixation system, and 16.5% were compatible with magnetic resonance. Although dual chamber sequential pacing continues to be more widespread, pacing with VVI/R mode is used because up to 23.8% of the patients with sinus node disease are in sinus rhythm, as are 24.1% of those with atrioventricular block.
ConclusionsThe total use of pacemaker generators in Spain has increased by about 5% with respect to 2014. The majority of the leads implanted are of active fixation, and less than 20% are protected from magnetic resonance. The factors directly related to the selection of pacing mode are age and sex. In around 20% of patients, the choice of the pacing mode could be improved.
Keywords
The Spanish Pacemaker Registry was created with the object of establishing a record of pacemakers implanted in Spain, which would allow us to have updated information on all the aspects related to implantation, the creation of a census of patients with pacemakers (an information that makes control easier and the vigilance of these products) and the preparation of statistical analysis for the different factors collected. The first official report of the Spanish Pacemaker Registry was written in 19971 and, since then, it has been published every year and is an annual report of the data related to pacemakers implanted in Spain the previous year.2–14 The present report offers the cardiac pacing activity undertaken in 2015, in hospitals in Spain, and compares it with that carried out in previous years and with that performed in other countries of our vicinity.15
METHODSThe Spanish Pacemaker Registry is supplied by information obtained from 3 sources: the European Pacemaker Patient Identification Card (EPPIC), manufacturers who distribute the devices, and the Spanish National Institute of Statistics (Instituto Nacional de Estadística [INE]).
European Patient Pacemaker Identification CardThe information provided by each hospital on the pacemakers implanted comes from the EPPIC, which is sent to the Spanish Pacemaker Registry. There are centers that send the data electronically, from their own databases. There will soon be an online application, that will be developed in agreement with the Spanish Agency of Medications and Medical Products. This will allow implanting centers to introduce data concerning the implantation of a pacemaker, obtained directly from the data introduced into the EPPIC, and perform the appropriate statistical analyses. We hope that it will be made available in the next few months, and that its use be made extensive to the largest number of centers possible. It is thought that the information received will reflect more reliably the work being done in cardiac pacing in Spain.
Device SuppliersSince not all of the EPPIC are sent, although it is obligatory according to the law in force (Royal Decree 1616/2009, dated October 26), which regulates all active implantable health care products concerning the effects of remaining attentive to possible alerts. Every year, all the companies that supply devices involved in the information retrieved from implantable material (pacemaker generators and cardiac resynchronization therapy [CRT], of high- [CRT-D] and low- [CRT-P] energy) are asked for the data in all of Spain, and in each Spanish autonomous community. This information is sent to the European Confederation of Medical Suppliers Associations (Eucomed).
Spanish National Institute of StatisticsThe populations for calculating the incidence of devices implanted in all of Spain and in each autonomous community are obtained from the updated report of the INE for 2015.16 Specifically, the population on July 1, 2015, is used.
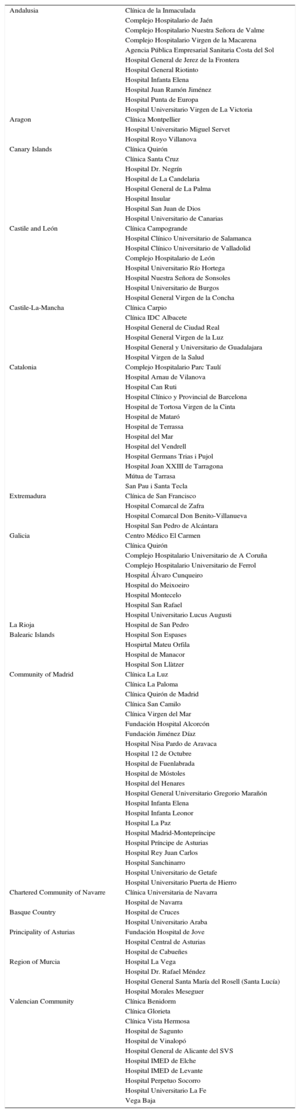
Sample AnalyzedOf the 111 hospitals who sent information on the procedures they had carried out (Table 1), with 12 507 implants conveyed, which represents 31.9% of the generators used, according to the information provided by the companies who distribute them. We consider that this should be representative of the activity involving “cardiac pacing” performed in Spain in 2015.
Public and Private Hospitals That Submitted Data to the Spanish Pacemaker Registry in 2015, Grouped by Autonomous Community
| Andalusia | Clínica de la Inmaculada |
| Complejo Hospitalario de Jaén | |
| Complejo Hospitalario Nuestra Señora de Valme | |
| Complejo Hospitalario Virgen de la Macarena | |
| Agencia Pública Empresarial Sanitaria Costa del Sol | |
| Hospital General de Jerez de la Frontera | |
| Hospital General Riotinto | |
| Hospital Infanta Elena | |
| Hospital Juan Ramón Jiménez | |
| Hospital Punta de Europa | |
| Hospital Universitario Virgen de La Victoria | |
| Aragon | Clínica Montpellier |
| Hospital Universitario Miguel Servet | |
| Hospital Royo Villanova | |
| Canary Islands | Clínica Quirón |
| Clínica Santa Cruz | |
| Hospital Dr. Negrín | |
| Hospital de La Candelaria | |
| Hospital General de La Palma | |
| Hospital Insular | |
| Hospital San Juan de Dios | |
| Hospital Universitario de Canarias | |
| Castile and León | Clínica Campogrande |
| Hospital Clínico Universitario de Salamanca | |
| Hospital Clínico Universitario de Valladolid | |
| Complejo Hospitalario de León | |
| Hospital Universitario Río Hortega | |
| Hospital Nuestra Señora de Sonsoles | |
| Hospital Universitario de Burgos | |
| Hospital General Virgen de la Concha | |
| Castile-La-Mancha | Clínica Carpio |
| Clínica IDC Albacete | |
| Hospital General de Ciudad Real | |
| Hospital General Virgen de la Luz | |
| Hospital General y Universitario de Guadalajara | |
| Hospital Virgen de la Salud | |
| Catalonia | Complejo Hospitalario Parc Taulí |
| Hospital Arnau de Vilanova | |
| Hospital Can Ruti | |
| Hospital Clínico y Provincial de Barcelona | |
| Hospital de Tortosa Virgen de la Cinta | |
| Hospital de Mataró | |
| Hospital de Terrassa | |
| Hospital del Mar | |
| Hospital del Vendrell | |
| Hospital Germans Trias i Pujol | |
| Hospital Joan XXIII de Tarragona | |
| Mútua de Tarrasa | |
| San Pau i Santa Tecla | |
| Extremadura | Clínica de San Francisco |
| Hospital Comarcal de Zafra | |
| Hospital Comarcal Don Benito-Villanueva | |
| Hospital San Pedro de Alcántara | |
| Galicia | Centro Médico El Carmen |
| Clínica Quirón | |
| Complejo Hospitalario Universitario de A Coruña | |
| Complejo Hospitalario Universitario de Ferrol | |
| Hospital Álvaro Cunqueiro | |
| Hospital do Meixoeiro | |
| Hospital Montecelo | |
| Hospital San Rafael | |
| Hospital Universitario Lucus Augusti | |
| La Rioja | Hospital de San Pedro |
| Balearic Islands | Hospital Son Espases |
| Hospirtal Mateu Orfila | |
| Hospital de Manacor | |
| Hospital Son Llàtzer | |
| Community of Madrid | Clínica La Luz |
| Clínica La Paloma | |
| Clínica Quirón de Madrid | |
| Clínica San Camilo | |
| Clínica Virgen del Mar | |
| Fundación Hospital Alcorcón | |
| Fundación Jiménez Díaz | |
| Hospital Nisa Pardo de Aravaca | |
| Hospital 12 de Octubre | |
| Hospital de Fuenlabrada | |
| Hospital de Móstoles | |
| Hospital del Henares | |
| Hospital General Universitario Gregorio Marañón | |
| Hospital Infanta Elena | |
| Hospital Infanta Leonor | |
| Hospital La Paz | |
| Hospital Madrid-Montepríncipe | |
| Hospital Príncipe de Asturias | |
| Hospital Rey Juan Carlos | |
| Hospital Sanchinarro | |
| Hospital Universitario de Getafe | |
| Hospital Universitario Puerta de Hierro | |
| Chartered Community of Navarre | Clínica Universitaria de Navarra |
| Hospital de Navarra | |
| Basque Country | Hospital de Cruces |
| Hospital Universitario Araba | |
| Principality of Asturias | Fundación Hospital de Jove |
| Hospital Central de Asturias | |
| Hospital de Cabueñes | |
| Region of Murcia | Hospital La Vega |
| Hospital Dr. Rafael Méndez | |
| Hospital General Santa María del Rosell (Santa Lucía) | |
| Hospital Morales Meseguer | |
| Valencian Community | Clínica Benidorm |
| Clínica Glorieta | |
| Clínica Vista Hermosa | |
| Hospital de Sagunto | |
| Hospital de Vinalopó | |
| Hospital General de Alicante del SVS | |
| Hospital IMED de Elche | |
| Hospital IMED de Levante | |
| Hospital Perpetuo Socorro | |
| Hospital Universitario La Fe | |
| Vega Baja |
The percentage of data lost for each parameter is highly variable, between 4.5% for the reason for lead explantation and 54.3% in the etiology of the implantation. Specifically, in other parameters, the following percentages have been reported as lost: 39.3% in the electrocardiogram prior to implantation, 27.4% due to the sex of the patient, 27.4% in the type of lead fixation, 17.8% due to patient age and 44.5% due to symptoms prior to implantation. The calculation of the percentages given below, make reference to the data available after exclusion of the losses.
Number of Pacemaker Generators ImplantedThe total number of generators implanted, according to the data of the Spanish Pacemaker Registry, is 12 507, corresponding to the 111 participating centers. According to the data provided by the distributors, the number of generators used in Spain was 38 055, 1082 pacemakers more than for CRT, with no capacity to defibrillate or using low-energy (CRT-P), with a total of 39 137 devices. The total of devices conveyed by Eucomed was 37 571, more than 1091 CRT-P,17 which is 5% more than in 2014.
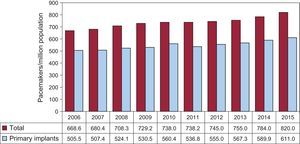
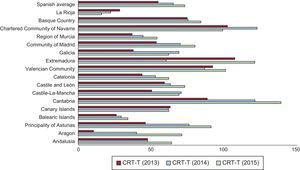
According to the data published by the INE, the population in Spain on the 1 of Julio 2015, was 46 423 064 (22 807 603 men and 23 615 461 women), 89 135 persons fewer than in July of 2014.16 The number of generators consumed was 820 per million population, according to the Spanish Pacemaker Registry (Figure 1) and 809 units per million, according to the Eucomed, which is a number clearly lower than the average of the countries who send their data to the Eucomed (954 units/million), although higher than that of certain countries with a higher per capita income like the United Kingdom, Denmark, The Netherlands, and Norway (712, 703, 729 and 758 units/million, respectively).
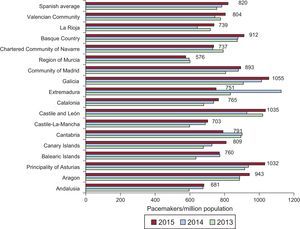
Spanish autonomous communities such as Galicia, Castile and León and the Principality of Asturias, continue to register, and in previous years, the greatest number of implantations/per million population, with more than 1000 units/million, followed by Aragon and the Basque Country with more than 900 units/million. We can also mentioned that, in Extremadura, the incidence of implantations has been reduced by more than 300 units/million (Figure 2).
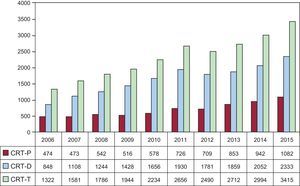
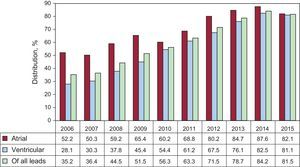
Cardiac Resynchronization DevicesThe total number of all CRT (CRT-T) implanted in 2015 (CRT-P and CRT-D) was 3415. The loss of CRT-T was 73 units/million, according to data from the Spanish Pacemaker Registry and from Eucomed. This year, the amounts for both registries coincide, with an increment of 12.7% with respect to 2014 (Figure 3). The number of CRT-P is 23 units/million, according to the Spanish Pacemaker Registry and from Eucomed, a finding that continues to be clearly lower than the average among countries who send their data to Eucomed (45 units/million), although higher than the rate of countries, like Poland or Greece, with 15 and 7 units/million, respectively. The number of CRT-D in Spain (50 units/million) is also significantly lower than the average of all European countries (126 units/million).
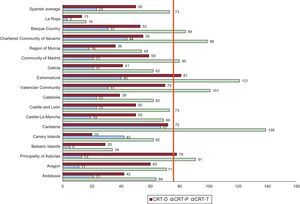
There continue to be differences between Spanish autonomous communities in the incidence of implantations, with Cantabria and Extremadura at the lead of implanted units CRT-T (139 and 121 units/million), followed by the Valencian Community, and the Chartered Community of Navarre and the Principality of Asturias. Extremadura has continued to recover the numbers of 2013, after a decrease in 2014, especially at the expense of the results for CRT-D. The Rioja continues to be the community with the fewest implantations of CRT-T. In CRT-P, the Chartered Community of Navarre, Cantabria, and Extremadura, accounted for 67, 44, and 40 units/million, respectively (Figure 4 and Figure 5).
The use of generators is greater for men than for women (58.2% vs 41.8%), both in primary implants (el 58.6% vs 41.4%) and in generator replacements (56.8% vs 43.2%).
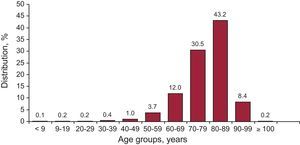
The average age of the patients reported to the Spanish Pacemaker Registry is 77.7 years, slightly higher than those who replaced a primary implantation (78.6 vs 77.5 years), and somewhat more in women than in men (78.8 vs 76.7 years). The greater percentage of implants continues to be in the decade of 80-89 years (43.2%), followed by that of 70-79 years (30.5%), 60-69 years (12%) and 90-99 years (8.4%). In all, 0.2% of implantations are performed in patients over 100 years (Figure 6).
Implantations and Generator ReplacementsPrimary implants involved 74.6% of the generators used in 2015. This fact implies an incidence of 611 units/million, plus replacements, 25.3%, an amount that includes the lead replacement associated with generator replacement, and constitutes 1.4% of the total activity.
The most common reason for explanting a generator is, as in previous years, the depletion of the battery life (90.4%), following selective replacement (2.2%), a change in the system for hemodynamic reasons or an upgrade due to pacemaker syndrome (1.8%), infection/erosion of the device (1.7%), early depletion because of elevated thresholds, high output energy programmed, or duration of the battery less than expected (1.3%), a complication of the lead (0.7%) or removal (0.5%). The remainder (1.4%) would correspond to unspecified reasons. The withdrawal of the generator due to infection occurs in 1.4% of all replacements, an incidence lower than in previous years.
Pacing LeadsPolarityIn all, 99.8% of the leads implanted are bipolar, with the same proportion in atrium as in right ventricle (99.9%). Of the unipolar leads, 56% correspond to pacing left ventricle via the coronary sinus; whereas 33% were intended for epicardial pacing in cardiac surgery (11% in right atrium and 22% in the right ventricle), and 11%, for epicardial pacing of the left ventricle. We should mention, however, that 64.3% of the leads implanted in coronary sinus vena are bipolar, in contrast to 34.1%, reported in 2014.14
Lead Fixation SystemsThe majority of the leads used (81.5%) are for active fixation, by means of a helical system that is inserted into the endocardium and confers stability in alternative sites of right ventricle apex and right atrial appendage. As in other years, the percentages of leads with active fixation in right atrium and ventricle are similar (82.1% and 81.1%) (Figure 7) and, in individuals of more than 80 years, and are fewer than in patients who have not reached that age (77.8% vs 82.4%).
Compatibility With Magnetic ResonanceThe use of electrodes compatible with magnetic resonance imaging (MRI) has been reduced since 2014 (from 16.5% to 21.3%), both in atrium (17%) and in ventricle (16.4%). With respect to the differences in their use, depending on the patient's age, they are implanted more in younger individuals than in patients of 80 years or more (18.4% vs 12.4%). With the information gathered from the EPPIC, it is not possible to communicate the percentage of generators implanted that are compatible with this radiological technique.
Change and Lead RemovalThere have been 179 explanted leads, a volume that is 1.1% of the total of the aforementioned leads implanted. The cause most widespread for removal is erosion-infection (40.9%), followed by dislodgment (13.6%), and defects in the insulation (13.6%), that required the elective change of the lead (9.1%) and lead conductor fracture (4.5%). The remainder were replaced due to unspecified causes.
A new lead in a patient with a pacemaker is 1.4% of the activity. The implantation of electrodes requires a replacement of the generator in the context of upgrading, with the objective of improving the hemodynamic system and symptoms of the patient. In 0.4% of the patients, it is usually the cable that has to be changed.
Symptoms, Etiology and Electrocardiogram, Prior to ImplantSymptomsSyncope continues to be the most common conduction defect (41.7%) to which to attribute these episodes, followed by dizziness (26.1%), dyspnea (16.2%), and bradycardia (10.4%). In all, 2.7% of the patients are asymptomatic, and the implant of the device was prophylactic. Less likely the causes are tachycardia (1.1%), chest pain (0.8%), cerebral dysfunction (0.4%), and cardiac arrest due to bradyarrhythmia (0.2%).
EtiologyThe most common cause of implantation continues to be fibrosis of the conduction system (45.8%) and unknown etiology (37.4%) and, to a lesser extent, ischemic etiology (4.4%; postinfarction, 0.2%), iatrogenic (3.6%); after ablation, 1%), valvular (2.4%), due to cardiomyopathies (2.9%; hypertrophic cardiomyopathy, 0,5%), congenital (0.6%), carotid sinus syndrome/sick sinus syndrome (SSS) (0.5%), vasovagal syncope (0.2%) and heart transplantation (0.2%). The remainder (2%) correspond to other etiologies that have not been codified.
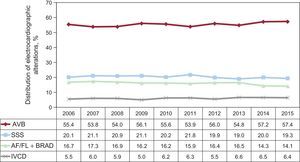
Electrocardiogram Prior to ImplantThe most common electrocardiographic alteration prior to implant continues to be atrioventricular block (AVB) (57.4%), including third degree AVB (36.6%), first and second degree AVB (16.2%), and atrial fibrillation (AF) with complete AVB (4.6%). It is followed in frequency by SSS (33.5%) and, that group also includes AF with bradycardia (14.1%) and bradycardia-tachycardia syndrome (6.9%). Branch block is reported in (6.4%) and, below that frequency, there is sinus rhythm with electrophysiological changes (2.4%), atrial tachycardia (0.2%) and, at a rate of<0.1%, plus ventricular tachycardia, with no specified rhythm (Figure 8).
Regarding sex-related differences, AVB (64.5% vs 56.0%), AF with bradycardia (19.4% vs 17.6%), and conduction defect (7.3% vs 3.6%) are all more frequent in men, whereas SSS is more common in women (25% vs 16.8%).
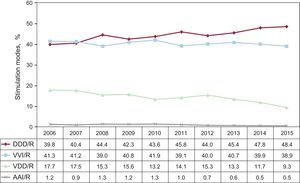
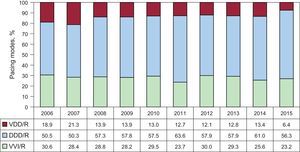
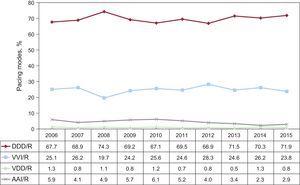
Pacing ModesSingle-chamber pacing constituted 39.4% of the total generators implanted in 2015. This percentage includes single-chamber atrial pacing (AAI/R), which is reported in 0.5%, and remains steady with respect to the findings for 2014 (Figure 9). The rate of primary implants with AAI/R mode is steady with respect to the previous year (0.4%),14 and the mode continues to decline progressively in terms of generator replacements (1%). On the other hand, single-chamber ventricular pacing (VVI/R), is reported for 38,9% of the total generators implanted; it has decreased in the case of primary implants (39.4%), but maintains its numbers with regard to replacements (37.4%) (Figure 9). Taking into account that the electrocardiographic diagnostic prior to the implant, in which only 18.7% of the patients have permanent atrial tachyarrhythmia, it can be estimated that up to 20.2% of the patients who receive single-chamber ventricular pacing could have received a pacemaker capable of maintaining atrioventricular synchrony. A number of factors can be considered in the final decision as to the pacing mode, and are analyzed in the next chapter, devoted to selecting the mode.
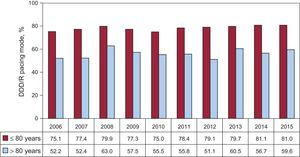
Dual-chamber sequential pacing, utilizing either 1 or 2 leads, comprises 57.7% of all the implanted generators, numbers that have remained steady in recent years.5–14 The use of single-lead sequential pacing (VDD/R) continues to decline, and represents only 9.3% of the total of implanted units (Figure 9). As occurs with AAI/R mode, the trend towards a less widespread utilization of single-lead sequential pacing remains evident, if we observe the progressively decreased use of this pacing mode for primary implants, as has been reported for previous years. However, there is also an accused decrease in the percentage of replacements involving this pacing mode (7.9% in primary implants and 13.6% in replacements). The use of dual-chamber pacing with 2 leads (DDD/R) is the mode most utilized, in general, with 48.4% of the total of implanted generators, 49.9% in primary implants, and 43.8% in replacements (Figure 9). Biosensors that enable the variation of pacing frequency are practically a standard, in DDD/R devices, as they are employed in 94.3% of the total production.
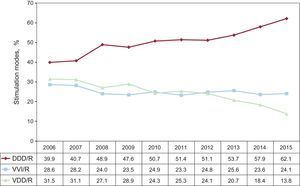
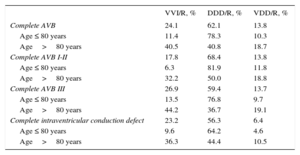
Pacing Mode SelectionAtrioventricular BlockTo assess the degree of adaptation to the most widely recommended pacing modes,18,19 we limit the study to nearly those patients who are in sinus rhythm, and exclude the group with permanent atrial tachyarrhythmia and AVB, C8 of the EPPIC codes; we analyze possible factors that could influence that selection, such as age, sex, and degree of block.
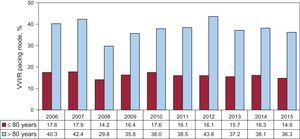
Pacing is mostly synchronous with the atrium (DDD/R and VDD/R) (75.9%), comparable to that of previous years. There seems to be an increase in the use of DDD/R mode (62.1%), fundamentally at the expense of a significant reduction in the utilization of VDD/R mode (13.8%). The use of VVI/R mode appears to be steady (24.1%) (Figure 10).
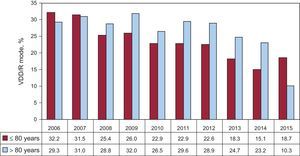
Age continues to greatly influence the pacing mode selected. Likewise, in patients of ≤ 80 years of age, atrioventricular synchrony, when maintained, is clearly the most widespread (88.6% of the cases); DDD/R mode is the most amply utilized (78.3%). In this age group, the increase in the use of DDD/R mode in detriment to VDD/R (10.3%) is still greater than in the total population, and there is a clear reduction in the use of VDD/R mode, with respect to previous years (Figure 11). In contrast, in patients older than 80 years, there is a significant reduction in the utilization of pacing modes that maintain the atrioventricular synchrony up to 59.5%, whereas single-chamber ventricular pacing is employed in 40.5%. In contrast to what occurs in younger age groups, we observe a greater use of VDD/R mode in patients older than 80 years (18.7%) in detriment to DDD/R (40.8%) (Table 2).
Distribution of Implant Pacing Modes Due to Electrocardiographic Alterations According to Age in 2015
| VVI/R, % | DDD/R, % | VDD/R, % | |
|---|---|---|---|
| Complete AVB | 24.1 | 62.1 | 13.8 |
| Age ≤ 80 years | 11.4 | 78.3 | 10.3 |
| Age>80 years | 40.5 | 40.8 | 18.7 |
| Complete AVB I-II | 17.8 | 68.4 | 13.8 |
| Age ≤ 80 years | 6.3 | 81.9 | 11.8 |
| Age>80 years | 32.2 | 50.0 | 18.8 |
| Complete AVB III | 26.9 | 59.4 | 13.7 |
| Age ≤ 80 years | 13.5 | 76.8 | 9.7 |
| Age>80 years | 44.2 | 36.7 | 19.1 |
| Complete intraventricular conduction defect | 23.2 | 56.3 | 6.4 |
| Age ≤ 80 years | 9.6 | 64.2 | 4.6 |
| Age>80 years | 36.3 | 44.4 | 10.5 |
AVB, atrioventricular block.
When pacing was analyzed based on the atrium, depending on the AVB grade, we could observe a greater utilization in the patients with first and second degree (82.2%) than in the patients with third degree AVB (73.1%). These differences are due to a larger utilization than DDD/R mode in first and second degree AVB, a trend that has been observed in recent years9–14 (Table 2). However, these differences are minimal in the case of individuals under 80 years of age (93.7% for first and second degree AVB, vs 86.5% for third degree AVB), although they are much more accused in the population over 80 years (67.8% and 55.8%, respectively) (Table 2).
As, in previous years, there continue to be sex-related differences in the manner of selecting a pacing mode.11–14 Accordingly, DDD/R pacing is utilized more frequently by men; however, VDD/R mode is used more by women. Among women of ≤ 80 years, the percentage of utilization of DDD/R pacing is up to 5 points lower than in men (69.7% vs 75.1%), and, this is due to a greater use of both VDD/R mode (18.1% vs 15.1%) and VVI/R mode (12.2% vs 9.9%). Overall, sequential pacing is utilized 2.6% less in women of ≤ 80 years and 4.6% less in the group of women who are older than 80 years.
There continues to be a high percentage of patients who receive single-chamber ventricular VVI/R pacing, when their electrocardiographic diagnosis shows AVB with preserved sinus rhythm. This means that, 24.1% of the total (Figure 10) is indicated especially for the most elderly patients (40.5% when those over 80 years are included) (Figure 12), and its use is higher in third degree blocks (Table 2) and in women from both age groups.
Intraventricular Conduction DefectsDual-chamber pacing in DDD/R mode remains the most widely used mode in this group of patients, involving 56.3% of the implants, followed by VVI/R pacing (23.2%). In the meantime, VDD/R continues in a clear decline, with 6.4% (Figure 13). Likewise, the increasingly utilized CRT-P devices in patients with intraventricular conduction defects, both in sinus rhythm (12.5%) and permanent AF (1.6%). In general, the pacing of these devices was mostly to preserve atrioventricular synchrony, 75.2% of all implants, a finding similar to that of recent years.
The pacing mode in most of this subgroup of patients is, again, influenced by age, as occurred with the AVB patients. Pacing in VVI/R mode is much more frequent among those older than 80 years (36.3% of all implanted patients), and nearly equals that of the percentage of DDD/R devices implanted in this age group (44.4%). In contrast, among patients of ≤ 80 years, the VVI/R mode is used only in 9.6% of this subgroup, whereas DDD/R mode is utilized more widely (64.2%). Overall, VDD/R mode is used much more frequently among patients older than<80 years (10.5% vs 4.6%) (Table 2).
Devices for CRT-P for the treatment of ventricular dysfunction with intraventricular conduction defect continue to grow constantly, with respect to those reported in recent years with 14.2%, an increase of 3 percentage points with respect to 2014.14 Again, the CRT-P device is much more frequent in patients of ≤ 80 years (21.6% of all implants), than among those over the age of 80 years (8.8%). With respect to previous years, the percentage of CRT-P in individuals under 80 years continues to be increasing significantly, and triplicates that of patients older than 80 years, which remains consistent with data from earlier years.5–14
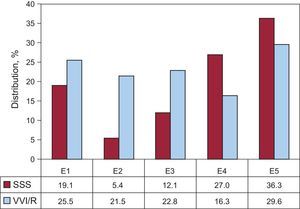
Sick Sinus SyndromeThe appropriateness of pacing modes to the recommendations in line with those proposed by clinical practice guidelines18,19 was assessed by separating the patients into 2 large groups: on the one hand, patients who are theoretically in permanent AF or atrial flutter with associated bradycardia (code E6 of the EPPIC); on the other hand, those who, at least, theoretically, remained in sinus rhythm.
A. Sick Sinus Syndrome in Permanent Atrial Tachyarrhythmia. As would be expected, in this situation, most of the implanted generators were VVI/R (94.1%). However, 3.8% received a DDD/R generator and 0.3% received a VDD/R device, which are hard to justify in SSS. The utilization of DDD/R mode could be explained in patients in whom restoration of sinus rhythm is expected. In all, 1.9% of the patients were reported to receive a CRT-P device.
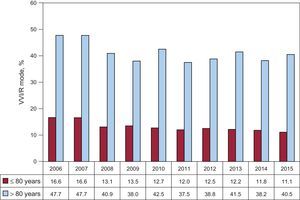
B. Sick Sinus Syndrome in Sinus Rhythm. In the remaining electrocardiographic manifestations of SSS, sinus rhythm is the predominating rhythm, whether steady or intermittent. Therefore, the most widely utilized pacing mode is DDD/R, as is recommended by current clinical practice guidelines,18 with 71.9%, followed by 23.8% with VVI/R, 2.9% with AAI/R, and 0.8% with VDD/R. Pacing mode AAI/R increases slightly with respect to the year before, but remains in very low levels, probably because of the recommendations of the most recent clinical practice guidelines18 (Figure 14). The percentage of patients with VDD/R pacing continues to decline with respect to recent years, in adjustment to clinical practice guidelines. This pacing mode is not suitable for SSS, unless there are other circumstances, such as a technical difficulty for the implantation of the atrial lead (Figure 14).
The different electrocardiographic manifestations of SSS were analyzed—excluding subgroups E7 and E8 of the EPPIC (interatrial block and chronotropic incompetence)—due to their minimal representation over the years. The percentage for VVI/R pacing ranges between 16.3% and 29.6%; again, the highest percentage corresponds to bradycardia-tachycardia syndrome (subgroup E5 of the EPPIC codes) (Figure 15). However, these data may have been magnified, because of the possibility of including erroneously, in this group, patients with permanent AF with fast-slow episodes, rather than in the E6 group, of which we spoke above.
Distribution of VVI/R pacing, according to the codes determined by the European Pacemaker Patient Identification Card in SSS. E1, SSS not specified; E2, exit block; E3, sinoatrial arrest; E4, bradycardia; E5, bradycardia-tachycardia syndrome; SSS, sick sinus syndrome; VVI/R, single-chamber ventricular pacing.
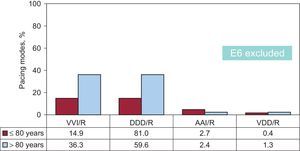
In regard to the influence of age in selecting the pacing mode for SSS, as occurred in AVB, in patients of ≤ 80 years, there was more frequent use of pacing modes that enable the detection and pacing of the atrium, that is, AAI/R and DDD/R (2.7% and 81%, respectively), vs only 14.9% in VVI/R. However, in the group of patients older than 80 years, there is more frequent utilization of VVI/R mode (36.3% vs 59.6% with DDD/R and 2.4% with AAI/R) (Figure 16). These results are consistent with those obtained in recent years. There is still a small representation of VDD/R pacing mode in both age groups (0.4% and 1.3%), which continues to be reduced progressively with regard to the findings of previous years (Figure 16). Age is shown to be influential in mode selection over the years studied (Figure 17 and Figure 18).
With regard to the analysis of the influence of sex on pacing mode selection, in the oldest population studied (> 80 years), VVI/R is used 2.9% more in men than in women. However, in patients aged ≤ 80 years, it is used 3.4% more in women than in men.
Home Monitoring/Follow-upIn all, 5% of the total of conventional pacemakers and 15.9% of CRT-P units are included in 2015 programs for home monitoring and follow-up.
Leadless PacemakersDuring 2015, data on the implantation of leadless pacemakers, from their only manufacturer, were obtained for the first time. These devices permit only VVI/R pacing mode.20 Overall, 77 units of this type have been implanted in all of Spain21; Catalonia is the Spanish autonomous community in which there are most units implanted, 36. All of the implants have been done in only 9 autonomous communities. Taking these data into account, leadless pacing constituted 1.6% of all the VVI/R devices implanted in 2015.
DISCUSSIONA first aspect that should be brought to light in the analysis of data for the registry is the percentage of data lost in the different parameters studied. Although the information provided by the registry is probably representative of the pacing activity done in Spain, although it is also certain that an area for improvement could be a better implementation of the data sent to a given registry. Along these lines, we are sure that an online application could certainly result in an advance in the quality of data collection and interpretation.
The total consumption of pacemaker generators in Spain grew by 5% with respect to 2014, and the trend observed in recent years is maintained. In fact, the change is greater than that registered for 2014 (from 1.1% with regard to 2013).14 If we take into account, the constant decline of the Spanish population, the increase in the number of implants could be explained by the aging of the population, with a mean age at the time of implantation of 77.7 years. The progressive financial recovery may have influenced this growth. The number of pacemakers (excluding CRT-P) per million population also increased from 820 units/million, a rise of 36/million more than in the previous year. Concerning the countries that send data to Eucomed, Spain continues to fall below the European average (954 units/million), in accordance with the lower per capita health cost than in countries in northern and western Europe, such as, Germany, Belgium, or France.17 However, there may even be other reasons, aside from economics, to explain, the disparity in the implantation rates among different countries, as some, like the United Kingdom, Denmark, Norway, or The Netherlands, present a lower number of implants per million population than Spain, despite the larger gross national income and greater health care spending. Other causes may be the lack of a labor supply, resources, or training programs, and a lower incidence of the diseases for which implantation is indicated and low rates of referral.
Regarding the findings for CRT-T, a proposal in 2015 is an increase of 12.7% with respect to 2014 (8 units/million), which would likewise affect high- and low-energy. The ratio of CRT-D and CRT-P is 2.2, with 50 CRT-D units/million and 23 CRT-P units/million population. Despite, the increase, in CRT, Spain remains under the European average in the rate of implants (45 CRT-P units/million and 126 CRT-D units/million in the European countries evaluated in Eucomed).
We also describe, as in other years,5–14 the disparity in the incidence of implants observed in Spanish autonomous communities. The most probable causes are the variations in the mean age of each population, the distinct health structures that are implicated in the differences in the density of arrhythmia units and heart failure units, as well as the rates for patient referral, the different situations and economic managements. More pacemakers are implanted in Galicia, Principality of Asturias, and Castile and León, probably because their populations are older. In contrast, there are more CRT devices implanted in Cantabria, the Chartered Community of Navarre, the Valencian Community, and Extremadura.
There is still a larger percentage of implantation among men, possibly because they are more predominant in this group of AVB and AF with bradycardia. Somewhat more than half of the implants are performed in patients over 80 years.
With respect to the type of lead implanted, most are bipolar, both in atrial and ventricular position. Unipolar electrodes are employed to pace left ventricle via the coronary sinus, although, in general, most of the electrodes implanted for this purpose are bipolar (64.3%). The registry does not collect the increasingly widespread use of quadripolar leads in the coronary sinus, which make it possible to choose, among the multiple electronic configurations, that which will have the best electrical behavior (the best pacing threshold) and without phrenic pacing.22 The majority of the leads are for active fixation systems (81.5%), both in atrium and ventricle, making it possible to place the leads at sites alternative to the apex of the right ventricle and atrial appendage, looking for a more physiological pacing pattern. Long-term pacing in right ventricular apex has detrimental effects on ventricular function and increases the incidence of AF and heart failure.
The use of leads compatible with MRI was less significant than even a year ago, which is not explicable if it is not taken into account that most manufacturers offer this feature as a protection against radiation of this type. In the oldest patients, the use of these leads is even less widespread. It could be that the greater cost of compatible generators, usually at the high-end of the price range, also limits the use of leads compatible with this technique. The incidence of compatible generators implanted is unknown, a fact that we hope to ascertain with the introduction of the online application. The more generalized use of MRI and the progressively more advanced age of the population to benefit from studies of this type make the extensive use of systems compatible with this radiological technique necessary.23
As occurred with anterior years, the most frequent electrocardiographic alteration prior to implant continues to be AVB, mainly in detriment to third degree AVB. The most widespread pacing mode in this setting, is still synchronous with the atrium (75.9%). Pacing with DDD/R mode continues growing with respect to previous years (62.1%), and we observe that the findings for the utilization of VVI/R remain steady (24.1%), whereas the percentage of the use of VDD/R mode (13.8%) keeps on declining. Age continues to be a determining factor when the time comes to decide the pacing mode in this context. In this manner, the majority of the patients under 80 years with AVB receive DDD/R pacing, whereas 40% of those over 80 years are receiving single-chamber pacing. Likewise, VDD/R pacing mode to maintain atrioventricular synchrony is used most frequently in individuals over 80 years (18.6% vs 10.3%), although we note that it has declined in both age groups with respect to previous years.
In SSS, the pacing mode based on the atrium continues to be the most widespread approach, with predominance of DDD/R mode (71.9%), as proposed by current clinical practice guidelines.18 We observe that VVI/R mode continues to be utilized in 23.8% of all the cases of SSS, although its use continues to decline with respect to previous years. Once again, age influences the selection of the pacing mode in SSS, as well. Thus, single-chamber VVI/R is more frequent among patients over 80 years (36.3%) and in bradycardia-tachycardia type SSS (38.9%), possibly because of the risk of permanent AF in a near future or because the individual has been erroneously included in the group of patients with permanent slow-fast AF. In any case, as recommended by current guidelines, DDD/R pacing is the most recommendable mode in SSS, mainly because of its positive effect by decreasing the rate of AF and stroke, and the reduced risk of pacemaker syndrome, which can deteriorate patient quality of life. Pacing with AAI/R mode continues to decline in accordance with current clinical practice guidelines, based on the results of the DANPACE study24 and the disadvantage offered by this pacing mode, taking into account que, each year, 0.6%-1.9% of the patients with SSS develops AVB. In atrial tachyarrhythmia with a slow ventricular response, the most widespread mode is VVI/R.
In intraventricular conduction defects, DDD/R pacing is the mode most frequently utilized (56.3%), followed by VVI/R (23.2%). Age again influences the selection of pacing mode, with a greater use of DDD/R mode in patients under 80 years, 6.8% of whom receive single-chamber pacing. Pacing mode VDD/R is utilized with less frequency and with no differences related to age. Pacing with CRT-P has increased over the past year in this group of patients, becoming 14.2% of the procedures with this electrocardiographic indication, reaching 21.6% in patients under 80 years, and is much less utilized (8.8%) among those over 80 years.
For the first time, the Spanish Pacemaker Registry includes data on leadless pacemaker implants. A total of 77 units were implanted during 2015.21 We observe that those implants were performed in only 9 Spanish autonomous communities. From the point of view of the physician, there are still very few indications for the implantation of devices of this type. Moreover, the present cost of this technology is much greater than that of the conventional single-chamber pacemaker. Thus, health administrators for each autonomous community have also had to establish a series of limitations to their use. These limitations will also probably be reduced over the next few years and, we will witness a progressive growth in leadless pacemaker implantations.
Home monitoring continues to have little application in pacing units, despite the growing evidence of the benefits of this follow-up system.25 There may be organizational and economic questions that introduce limitations for its generalized use.
CONCLUSIONSThere is still an increase in the incidence of conventional pacemaker and CRT-P implants, despite the fact that Spain continues below the average of our neighboring countries. Age is the major factor determining the pacing mode, which is unsuitable in approximately 20% of the cases of patients with AVB and SSS. Leadless pacing is an incipient in Spain, but promising, and its efficacy and safety will require the necessary long-term studies.
CONFLICTS OF INTERESTNone declared.