Keywords
INTRODUCTION
The Spanish Registry of Pacemakers (BNDM, Banco Nacional de Datos de Marcapasos) has been compiling data on the use of these devices since 1990.1 Because of the changes brought about in the computer systems, with improvements and adaptations to the software used in other databases of the Spanish Society of Cardiology (SEC, Sociedad Española de Cardiología), comparative analysis of data from successive years has been possible since 1994.
Prior information on the status of cardiac pacing with the use of pacemakers in Spain was published in 19972 and 2004.3 This information, which includes the changes in this activity occurring over the years, is available in the Cardiac Pacing Section of the SEC website (www.marcapasossec.org).
In addition to the registry information from 2003, the data now presented focus on changes that have taken place in the pacing modes used for the various electrocardiographic indications prompting the placement of these devices since 1994. The information has been compiled from the European Pacemaker Patient Identification Card notification system, which has been compulsory since 1993 (Spanish Royal Decrees 634/1993 and 414/1996).
The hospitals that reported their data in 2002 and 2003 are shown in Appendix.
POPULATION
In 2003, 8417 cards with data on pacemaker implantation or replacement of pacemaker generators were sent to the BNDM from among an estimated total of 22 098, based on information provided by the various industries implicated (38% of the total). This implies a rate of approximately 521.85 implanted generators per million population. Among patients receiving their first pacemaker, the rate was 415.4 per million population. These estimations are based on the Spanish population at the end of 2003 (42 345 342 inhabitants, 20 801 989 men, and 21 543 353 women), according to the website of the Spanish Statistics Institute (www.ine.es).
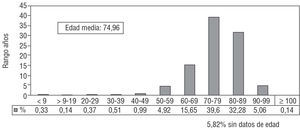
The mean age of patients requiring a pacemaker was 75.1 years, with women showing a slightly higher mean age than men (74.2 years in men and 76.3 years in women). Mean age was 74.9 years in patients receiving their first pacemaker, and 76 years in those requiring generator replacement.
The largest number of indications for pacemaker implantation were produced in patients in their seventies, accounting for nearly 40% of the total, followed by patients in their eighties, accounting for more than 30% (Figure 1).
Figure 1. Percent distribution of the population receiving their first pacemaker according to age, 2003.
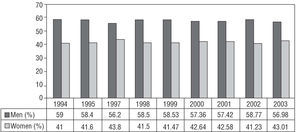
Among the initial implants, the percentage of men requiring a pacemaker was significantly higher than that of women (Figure 2), with similar figures recorded for pacemaker generator replacements (in 2003, 55% in men, 44.9% in women).
Figure 2. Percent distribution of the population receiving their first pacemaker generator according to sex, 1994-2003.
TYPE OF ACTIVITY
Initial implantation of a pacing system accounted for 79.6% of the total of units and replacement of a generator or a generator plus electrode encompassed 20.3% of the units. Among the latter, 1.6% included replacement of one or more electrodes, either to change the pacing modality or to add or replace (due to deterioration) leads. These percentages have remained stable over the last 2 years. Electrode replacement alone accounted for 0.1% of the procedures carried out.
ELECTRODES, POLARITY, AND FIXATION
The vast majority of electrode leads implanted (atrial, 28.5%; ventricular, 71.5%) were bipolar, in keeping with the clear increase in this polarity in recent years, which now accounts for 98.8% of all pacing leads. The small percentage of unipolar types reported (1.2%) mainly correspond to leads, which, by their design or caliber, are intended for special cases or sites: e.g., epicardial pacing through the coronary sinus (28% of all unipolar leads) or unipolar epicardial pacing in cardiac surgery (6%). Bipolar atrial pacing was recorded at 99.7%. Active fixation was used in 41.2% of atrial leads and 16.1% of ventricular leads.
PACING MODES
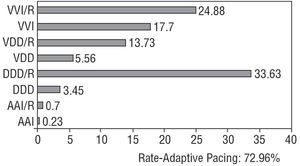
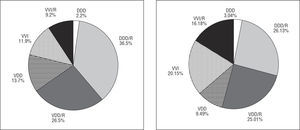
In 2003, the most frequently used modality was single-chamber ventricular pacing in 42.5%, followed by dual chamber pacing with 2 leads in 37%. Overall, physiological pacing accounted for 57.4% of the total and single-chamber atrial pacing, 0.9% (Figure 3).
Figure 3. Percent distribution of the various pacing modes and rate-adaptive pacing (first implants and generator replacements), 2003.
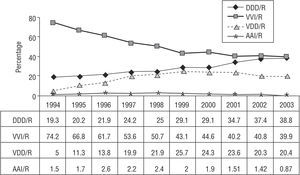
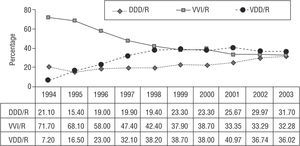
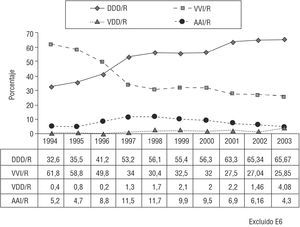
From 1994 up to 1999, so-called physiological pacing, in which atrioventricular synchrony is maintained (AAI/R, VDD/R, and DDD/R pacing) showed a considerable increase as compared to single-chamber ventricular pacing. This trend continued thereafter, although to a smaller degree (the ratio changed from 25.8:74.2 to 57.4:42.5). This was mainly a consequence of a notable increase in the VDD/R mode (particularly up to 1999-2000), and a somewhat smaller increase in the DDD/R mode. Single-chamber atrial pacing has remained generally stable, with an approximately 1% decrease since 1999 (Figure 4).
Figure 4. Pacing modes used in patients receiving their first pacemaker, 1994-2003.
Rate-adaptive pacing, mediated by various sensors, was provided by 72.9% of the generators implanted in 2003. Cardiac pacing to achieve ventricular resynchronization (first implants and replacements) accounted for 0.7% of the generators implanted in 2002 and 1.2% in 2003. The distribution of these devices in 2003 consisted of 1.1% for atrioventricular pacing and 0.2% for biventricular pacing among the total of first implants, and 0.5% and 0.2%, respectively, among the replacements.
ETIOLOGY
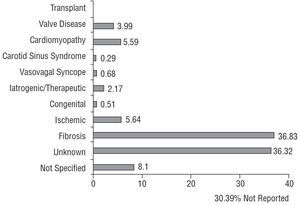
The most common reasons for pacemaker implantation were conduction system fibrosis and unknown causes, which together accounted for 73.1% of the total. The group of cardiomyopathies comprised 5.5% of the causes, and among them myocardial hypertrophy reached 0.7%. Pacing for clinical conditions mediated by the autonomic nervous system (carotid sinus syndrome or malignant vasovagal syndrome) represented 0.9%, with a range over the years included in the registry of 0.9% to 1.9% (Figure 5).
Figure 5. Percent distribution of the etiological reasons for pacemaker implantation, 2003.
SYMPTOMS
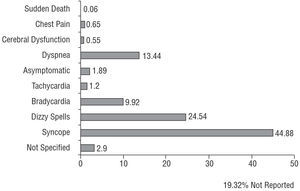
The most frequently reported signs and symptoms prior to or prompting pacemaker implantation were syncope, dizzy spells, dyspnea or signs of heart failure, and bradycardia. The incidence of prophylactic pacemaker implantation in asymptomatic patients was 1.8% (Figure 6).
Figure 6. Percent distribution of the symptoms prompting pacemaker implantation, 2003.
ELECTROCARDIOGRAPHIC ALTERATIONS
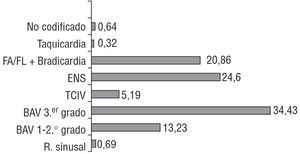
Among the electrocardiographic alterations leading to an indication of pacemaker implantation, atrioventricular conduction defects (AVCD) were the most numerous at 47.6%, followed by sick sinus syndrome (SSS) at 24.6% and atrial fibrillation with atrioventricular block (AVB) at 20.8% (Figure 7).
Figure 7. Percent distribution of the electrocardiographic alterations indicating pacemaker implantation, 2003. AVB indicates atrioventricular block; SSS, sick sinus syndrome; AF/FL + Brady., atrial fibrillation or flutter with slow ventricular response or complete AVB; Sinus r, normal sinus rhythm; Tachycardia, all tachycardia indications (supraventricular plus ventricular); IVCD, intraventricular conduction defect.
PACING IN ATRIOVENTRICULAR BLOCK
The predominant mode was VDD/R, accounting for 36%, followed by VVI/R at 32.2% and DDD/R at 31.7% (Figures 8, 9, and 10). Among the countries reporting data to the European Working Group on Cardiac Pacing, Spain uses VDD/R pacing more than any other, both in overall terms and specifically for AVB.
Figure 8. Pacing modes used for atrioventricular block (overall data, including first to third degrees, corresponding to identification card codes C1 to C7 and excluding cases of chronic atrial fibrillation, code C8), 1994-2003.
Figures 9 and 10. Pacing modes used for first- and second-degree atrioventricular block (codes C1-C4) and third-degree atrioventricular block (codes C1-C7), 2003.
The incidence of single-chamber ventricular pacing in AVB is 53.1% in patients 80 years of age or older and 21.2% in patients under 80 years of age.
PACING IN SICK SINUS SYNDROME
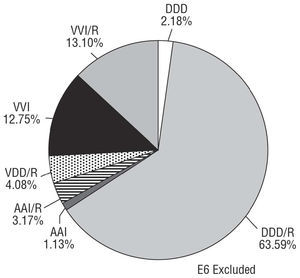
Pacing in DDD/R mode accounted for 65.7% of the total in 2003 after showing a steady increase since 1994, and has now duplicated the use reported at that time. Pacing in AAI/R mode has experienced a slow decrease to 4.3% in 2003, even though this mode has been demonstrated to be safe when there are no associated intraventricular conduction defects (IVCD).4,5 There has been a clear decrease in the use of the VVI mode, which, however, still holds steady at 25.8% (Figures 11 and 12).
Figure 11. Pacing modes used in sick sinus syndrome (codes E1-E8, excluding patients with atrial fibrillation plus bradycardia, code E6), 2003.
Figure 12. Percent distribution of the pacing modes used in first pacemaker implants in patients with sick sinus syndrome, excluding those with chronic atrial fibrillation, 1994-2003.
Analysis of the variations in the use of pacing modes according to age (cut-off at 80 years) showed the following results: in SSS patients, VVI pacing was 42% in persons over the age of 80 and 19.1% in younger patients; atrial single-chamber pacing in the 2 groups showed similar rates, at 5.1% and 4%, respectively.
PACING IN INTRAVENTRICULAR CONDUCTION DEFECTS
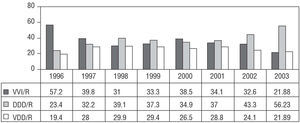
DDD/R pacing was the most extensively used in patients with IVCD, and there was a high rate of single-chamber ventricular pacing (21.8%), although the trends show a clear decrease in this mode (Figure 13).
Figure 13. Percent distribution of pacing modes used for intraventricular conduction defect (due to a change in the data processing system, no data are available before 1996), 1996-2003.
Pacing in IVCD patients for ventricular resynchronization has continued to show a slow increase, accounting for 1.2% of the total of pacemakers implanted in 2003 and 13.8% in the subgroup of patients with IVCD.
CONCLUSIONS
- There has been a notable increase in physiologic pacing modes, both overall and in each of the electrocardiographic indications recorded.
- The VDD/R mode, following a significant increase up to 1999-2000 when it reached 25% of the total, has initiated a decrease in favor of DDD/R pacing.
- The rate of AAI/R pacing has remained constant, without major variations over the period analyzed.
- Age was seen to be one of the factors that influences the pacing mode selected.
- Pacing for ventricular resynchronization accounted for more than 1% of the overall activity.
- Bipolar pacing was chosen for virtually all the electrodes used, whether atrial or ventricular.
- Finally, it is important to emphasize the advantages of increasing the use of pacing modes that maintain atrioventricular synchrony,6 and to send out a call for greater participation in submitting Pacemaker Patient Identification Cards to the pacemaker registry in order to make more complete and reliable information available. The sample obtained to derive the data for 2003 only represented 38% of the total. Further details for the other years cited can be consulted in the Cardiac Pacing Section of the SEC website.
ACKNOWLEDGEMENTS
We are grateful to Brígida Martínez Noriega, R.N., and Pilar Gómez Pérez, R.N., and to Gonzalo Justes Toha, computer engineer of the SEC, for their invaluable and vital assistance with the maintenance and quality control of the Spanish Pacemaker Registry (BNDM) data.
Correspondence: Dr. R. Coma Samartín.
Arturo Soria, 184, esc. 1.a, 3.o C. 28043 Madrid. España.
E-mail: coma@vitanet.nu