The cardiology day hospital (CDH) is an alternative to hospitalization for scheduled cardiological procedures. The aims of this study were to analyze the activity, quality of care and the cost-effectiveness of a CDH.
MethodsAn observational descriptive study was conducted of the health care activity during the first year of operation of DHHA. The quality of care was analyzed through the substitution rate (outpatient procedures), cancellation rates, complications, and a satisfaction survey. For cost-effectiveness, we calculated the economic savings of avoided hospital stays.
ResultsA total of 1646 patients were attended (mean age 69 ± 15 years, 60% men); 2550 procedures were scheduled with a cancellation rate of 4%. The most frequently cancelled procedure was electrical cardioversion. The substitution rate for scheduled invasive procedures was 66%. Only 1 patient required readmission after discharge from the CDH due to heart failure. Most surveyed patients (95%) considered the care received in the CDH to be good or very good. The saving due to outpatient-converted procedures made possible by the CDH was € 219 199.55, higher than the cost of the first year of operation.
ConclusionsIn our center, the CDH allowed more than two thirds of the invasive procedures to be performed on an outpatient basis, while maintaining the quality of care. In the first year of operation, the expenses due to its implementation were offset by a significant reduction in hospital admissions.
Keywords
In a publically-funded health system, and especially in times of budgetary deficits, it is essential to make the most of available resources.1 Clinical management encourages cost containment by avoiding unnecessary hospitalizations without decreasing the quality of the medical care provided. One approach to achieve this objective is to perform lower-risk, elective, diagnostic and therapeutic invasive procedures on an ambulatory basis by creating minor surgery units within day hospitals.
Day hospitalization refers to a hospital stay lasting some hours for various purposes: diagnostic testing, clinical and other examinations, and treatments that cannot be performed in the outpatient clinic, but do not justify hospital admittance.2 It is a medical care unit where certain interventions are performed and postprocedure medical or nursing attention is provided under the supervision or indication of a specialized physician.3
In the field of cardiovascular disease, several diagnostic and therapeutic activities can be carried out during a short stay limited to the day of the procedure, and these would be amenable to the medical care available in a day hospital. Certain factors, such as radial artery access in catheterization, have been key elements in this regard, as they reduce the incidence of complications and the need for puncture site care in both diagnostic and interventional procedures.4,5 The safety of ambulatory treatment has also been verified in device implantation and arrhythmia ablation procedures.6,7
Heart failure (HF) is one of the most prevalent cardiovascular syndromes, leading to heave resource utilization.8,9 HF units have proven effective in the treatment of these patients and have reduced the number of emergency room visits and rehospitalizations.10,11 Day hospitals are an excellent support tool for these units, as they facilitate close follow-up after hospital discharge and offer patients fast access to care in situations of clinical worsening. This benefit would apply not only to HF patients; it could be extended to others with a prompt hospital discharge or patients seen in the emergency department (eg, pericardial syndromes, atrial fibrillation, following heart surgery), who might need preferential access to reassessment, diagnostic tests, or therapeutic interventions that cannot be covered in the outpatient setting.
The cardiology day hospital (CDH) is conceived as an area designed to provide complex or sophisticated medical care with little delay and avoiding hospitalization in patients with cardiovascular conditions that can be treated in an ambulatory setting.12
Although numerous hospital cardiology departments have converted a large part of their invasive procedures to ambulatory ones because of CDH availability, there are no studies evaluating the clinical and cost-effectiveness of these areas within the specific field of cardiology. The aim of this study was to perform a descriptive analysis of the activity carried out, evaluate the quality of the care provided, and determine the cost-effectiveness of a CDH in the first year of operation.
METHODSA retrospective, descriptive, observational study was performed of all activity recorded in the CDH during its first year of operation (June 2014 to May 2015). We collected information on the reason for the visit, clinical and demographic data, and the origin and destination of the patients following the CDH visit (hospital discharge or admission).
Cardiology Day Hospital OrganizationLocation, Facilities, and StaffThe CDH is located at the entrance to the cardiology ward in a space previously occupied by 2 rooms for hospitalized patients. It has 7 medical care stations (4 hospital chairs and 3 beds), and equipment for basic cardiovascular care (eg, electrocardiography, blood pressure monitoring, pharmacy, telemetry) and for potential complications (eg, cardiac arrest cart with a defibrillator, intubation material).
The medical staff consists of a permanent team including 2 nurses and 2 auxiliary nursing technicians with extensive experience in the care of cardiology patients, working in 2 shifts, morning and afternoon. In addition, 1 supervising cardiologist is assigned to the morning shift.
The nursing care depends on the patient's procedure and is standardized according to the cardiology department protocols. Before discharge, all patients receive a medical report with their test results, the therapeutic approach, and nursing information on the necessary recommendations and the care required.
The CDH is open on weekdays from 8 in the morning to 10 in the evening.
Procedures Covered- 1.
Complex clinical examinations that do not need hospitalization and cannot be reasonably carried out in the outpatient clinic.
- 2.
Invasive procedures requiring preprocedure and postprocedure medical care in patients who are not at high risk and do not require postprocedure hospitalization.
- 3.
Invasive procedures in patients referred from other centers, who can then be discharged or referred back to their center of origin without the need for hospitalization.
- 4.
Noninvasive therapeutic procedures requiring subsequent posterior monitoring.
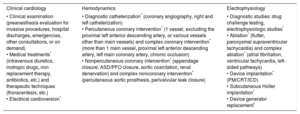
The various types of procedures are specified in Table 1.
Processes and Procedures That can be Carried out in the Cardiology Day Hospital, by the Section in Charge
| Clinical cardiology | Hemodynamics | Electrophysiology |
|---|---|---|
| • Clinical examination (preanesthesia evaluation for invasive procedures, hospital discharges, emergencies, other consultations, or on demand) • Medical treatments* (intravenous diuretics, inotropic drugs, iron replacement therapy, antibiotics, etc.) and therapeutic techniques (thoracentesis, etc.) • Electrical cardioversion* | • Diagnostic catheterization* (coronary angiography, right and left catheterization) • Percutaneous coronary intervention* (1 vessel, excluding the proximal left anterior descending artery, or various vessels other than main vessels) and complex coronary intervention* (more than 1 main vessel, proximal left anterior descending artery, left main coronary artery, chronic occlusion) • Nonpercutaneous coronary intervention* (appendage closure, ASD/PFO closure, aortic coarctation, renal denervation) and complex noncoronary intervention* (percutaneous aortic prosthesis, perivalvular leak closure) | • Diagnostic studies: drug challenge testing, electrophysiologic studies* • Ablation* (flutter, paroxysmal supraventricular tachycardia) and complex ablation* (atrial fibrillation, ventricular tachycardia, left-sided pathways) • Device implantation* (PM/CRT/ICD) • Subcutaneous Holter implantation* • Device generator replacement* |
ASD, atrial septal defect; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; PFO, patent foramen ovale; PM, pacemaker.
There are no quality indicators specifically designed for CDH evaluation. According to the recommendations of the Spanish National Health System,2 we adapted and evaluated some of the indicators proposed for day hospitals:
- •
Cancellation of sessions: Includes the cancellation rate—(number of patients scheduled in the CDH who do not attend/total number of patients scheduled in the CDH) × 100—and the suspension rate—(number of patients attending the CDH who do not receive the intervention/total number of patients attending the CDH) × 100.
- •
Conversion to ambulatory care: Evaluated by the substitution rate, defined as the percentage of procedures amenable to potential inpatient-outpatient substitution carried out by the CDH relative to the total scheduled. Only elective invasive procedures were included in this indicator.
- •
Adverse events: Complications attributable to an invasive procedure, occurring within the first 48hours after CDH discharge and requiring an emergency room visit or rehospitalization.
- •
User satisfaction: During the last month of the study period, an anonymous, voluntary survey was conducted by the CDH nursing staff in patients discharged from the CDH. Patients were asked to respond to questions about punctuality, the attention by the staff, the information received, a general evaluation of the CDH, and whether the patient would recommend it to other users. The satisfaction index was calculated as the percentage of responses in each response category.
In this study, cost-effectiveness was established when the health coverage provided by the CDH was identical to that of conventional hospitalization meeting the quality indicators, but at a lower cost.13 To determine cost-effectiveness, we calculated the hospital stays avoided because of the CDH and the final economic impact in terms of conventional hospitalization.
Calculation of Avoided Hospital StaysTo determine the impact of this new health care model on hospital admissions, we used as a reference the number of patients attended in the CDH for scheduled invasive procedures in the first year of operation and the number attended in hospital during 1 year (2013, control). The data on hospital admissions and the length of hospital stay were recorded for each case. Patients already hospitalized (in the emergency department, hospitalization ward, or other centers) were excluded from the analysis. We then calculated the length of hospital stays (mean and median of days hospitalized) and the hospitalization costs per each type of procedure for each care model.
Economic ImpactThe estimated savings were calculated as the difference in the mean cost per procedure of hospitalization expenditure between the control group and the CDH group. The hospitalization rates were obtained from the price list for publically-funded medical activity and health services established by the Regional Healthcare Management, updated in 2013. The corresponding cost for 1 day of hospitalization was €408.74 in a hospital ward and €1053.72 in the coronary unit (for a hospital in section 1).14 The total savings were obtained by multiplying the estimated average cost saving for each type of procedure by the number of these procedures performed in the CDH.
The final economic impact was calculated as the difference between the expenditure generated by the CDH (cost of remodeling the area, equipment, and personnel) and the savings in avoided hospital stays for scheduled ambulatory procedures.
Statistical AnalysisContinuous variables are expressed as the mean ± standard deviation and the median [interquartile range], and qualitative variables as the absolute frequency (number) and relative frequency (percentage). Continuous variables with a normal distribution were compared using the Student t test for independent samples and those with a nonnormal distribution with the Mann-Whitney U test. The statistical analysis was carried out with the SPSS software, version 20.0.0 (IBM Corp; Armonk, New York, United States), and Microsoft Office Excel, 2013.
RESULTSDuring its first year of operation, the CDH was open for 246 weekdays. A mean of 10 ± 3 patients were attended per day, and a mean of 1.5 visits were made per patient (range, 1-20). In total, 1646 patients were attended (mean age, 69 ± 15 years), and 60% were men. Among the total of visits, 67% were first visits and 33% were successive visits.
The most common reason for the appointment was a clinical examination, performed in 850 patients (35%); the most prevalent diagnosis was HF (65%). In addition, some type of medical treatment was administered to 182 patients (7%), mainly intravenous diuretics, (Table 2). HF patients attended in the CDH came from the emergency department (20%), hospital discharge (16%), and scheduled visits referred from the outpatient clinic or other departments (13%).
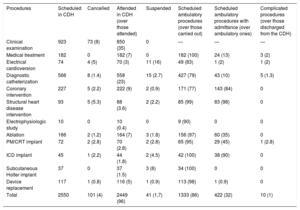
Summary of the CDH Activity in the First Year of Operation
| Procedures | Scheduled in CDH | Cancelled | Attended in CDH (over those attended) | Suspended | Scheduled ambulatory procedures (over those carried out) | Scheduled ambulatory procedures with admittance (over ambulatory ones) | Complicated procedures (over those discharged from the CDH) |
|---|---|---|---|---|---|---|---|
| Clinical examination | 923 | 73 (8) | 850 (35) | 0 | — | — | — |
| Medical treatment | 182 | 0 | 182 (7) | 0 | 182 (100) | 24 (13) | 3 (2) |
| Electrical cardioversion | 74 | 4 (5) | 70 (3) | 11 (16) | 49 (83) | 1 (2) | 1 (2) |
| Diagnostic catheterization | 566 | 8 (1.4) | 558 (23) | 15 (2.7) | 427 (79) | 43 (10) | 5 (1.3) |
| Coronary intervention | 227 | 5 (2.2) | 222 (9) | 2 (0.9) | 171 (77) | 143 (84) | 0 |
| Structural heart disease intervention | 93 | 5 (5.3) | 88 (3.6) | 2 (2.2) | 85 (99) | 83 (98) | 0 |
| Electrophysiologic study | 10 | 0 | 10 (0.4) | 0 | 9 (90) | 0 | 0 |
| Ablation | 166 | 2 (1.2) | 164 (7) | 3 (1.8) | 156 (97) | 60 (35) | 0 |
| PM/CRT implant | 72 | 2 (2.8) | 70 (2.8) | 2 (2.8) | 65 (95) | 29 (45) | 1 (2.8) |
| ICD implant | 45 | 1 (2.2) | 44 (1.8) | 2 (4.5) | 42 (100) | 38 (90) | 0 |
| Subcutaneous Holter implant | 37 | 0 | 37 (1.5) | 3 (8) | 34 (100) | 0 | 0 |
| Device replacement | 117 | 1 (0.8) | 116 (5) | 1 (0.9) | 113 (98) | 1 (0.9) | 0 |
| Total | 2550 | 101 (4) | 2449 (96) | 41 (1,7) | 1333 (86) | 422 (32) | 10 (1) |
CDH, cardiology day hospital; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; PM, pacemaker.
Values are expressed as No. (%).
In total, 2550 procedures were scheduled. The cancellation rate (excluding rescheduled procedures for which the patient did not attend the CDH) was 4%, and the suspension rate was 1.7%. The most prevalent reasons for cancellation were hospital admission for another cause (58%) and failure to attend the appointment (19%). The type of procedure with the highest suspension rate (16%) was electrical cardioversion (Table 2).
The incidence of complications could be analyzed in 716 patients discharged from the CDH following an invasive procedure. Fifteen patients presented to the emergency room within the first 48hours after discharge. There were 4 cases of HF, 3 contrast-related adverse reactions, 1 posttransfusion reaction, 1 pacemaker lead displacement, and 1 hematoma at the puncture site for catheterization. Only 1 of the HF patients required hospitalization.
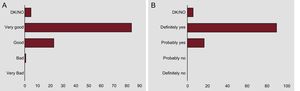
During the last month of the first year of operation, 113 satisfaction surveys were carried out. Among the total, 94% of patients surveyed considered that the care provided by the nursing staff was good or very good, and 92% rated the care by the medical staff as good or very good. Ninety percent considered that the clinical information provided on the procedure and at the time of discharge was adequate. Only 5 patients (4%) had difficulties in finding or gaining access to the CDH, and 12 (11%) were not attended within the first 15minutes after the scheduled time for admission. The overall rating of the CDH was good or very good in the opinion of 107 users (95%), and 90 (80%) stated they would definitely recommend it to other patients (Figure 1).
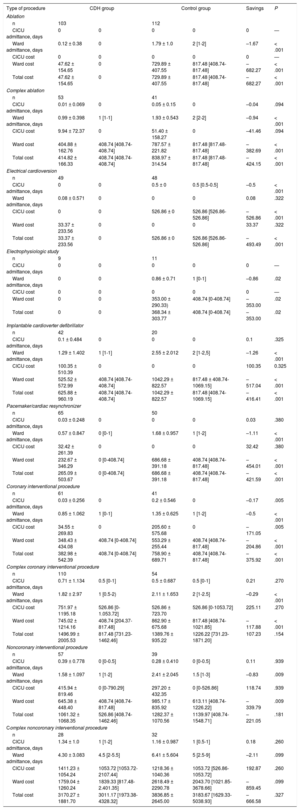
The cost of hospital stays and the average estimated savings are shown in Table 3, together with a comparison of the mean cost of each type of scheduled procedure before and after implementation of the day hospital.
Comparison of Mean Hospitalization Costs for Each Type of Scheduled Procedure Before and After Implementation of the Day Hospital, and Estimated Cost Savings in Hospital Stays
| Type of procedure | CDH group | Control group | Savings | P | ||
|---|---|---|---|---|---|---|
| Ablation | ||||||
| n | 103 | 112 | ||||
| CICU admittance, days | 0 | 0 | 0 | 0 | 0 | — |
| Ward admittance, days | 0.12 ± 0.38 | 0 | 1.79 ± 1.0 | 2 [1-2] | –1.67 | < .001 |
| CICU cost | 0 | 0 | 0 | 0 | 0 | — |
| Ward cost | 47.62 ± 154.65 | 0 | 729.89 ± 407.55 | 817.48 [408.74-817.48] | –682.27 | < .001 |
| Total cost | 47.62 ± 154.65 | 0 | 729.89 ± 407.55 | 817.48 [408.74-817.48] | –682.27 | < .001 |
| Complex ablation | ||||||
| n | 53 | 41 | ||||
| CICU admittance, days | 0.01 ± 0.069 | 0 | 0.05 ± 0.15 | 0 | –0.04 | .094 |
| Ward admittance, days | 0.99 ± 0.398 | 1 [1-1] | 1.93 ± 0.543 | 2 [2-2] | –0.94 | < .001 |
| CICU cost | 9.94 ± 72.37 | 0 | 51.40 ± 158.27 | 0 | –41.46 | .094 |
| Ward cost | 404.88 ± 162.76 | 408.74 [408.74-408.74] | 787.57 ± 221.82 | 817.48 [817.48-817.48] | –382.69 | < .001 |
| Total cost | 414.82 ± 166.33 | 408.74 [408.74-408.74] | 838.97 ± 314.54 | 817.48 [817.48-817.48] | –424.15 | < .001 |
| Electrical cardioversion | ||||||
| n | 49 | 48 | ||||
| CICU admittance, days | 0 | 0 | 0.5 ± 0 | 0.5 [0.5-0.5] | –0.5 | < .001 |
| Ward admittance, days | 0.08 ± 0.571 | 0 | 0 | 0 | 0.08 | .322 |
| CICU cost | 0 | 0 | 526.86 ± 0 | 526.86 [526.86-526.86] | –526.86 | < .001 |
| Ward cost | 33.37 ± 233.56 | 0 | 0 | 0 | 33.37 | .322 |
| Total cost | 33.37 ± 233.56 | 0 | 526.86 ± 0 | 526.86 [526.86-526.86] | –493.49 | < .001 |
| Electrophysiologic study | ||||||
| n | 9 | 11 | ||||
| CICU admittance, days | 0 | 0 | 0 | 0 | 0 | — |
| Ward admittance, days | 0 | 0 | 0.86 ± 0.71 | 1 [0-1] | –0.86 | .02 |
| CICU cost | 0 | 0 | 0 | 0 | 0 | — |
| Ward cost | 0 | 0 | 353.00 ± 290.33) | 408.74 [0-408.74] | –353.00 | .02 |
| Total cost | 0 | 0 | 368.34 ± 303.77 | 408.74 [0-408.74] | –353.00 | .02 |
| Implantable cardioverter defibrillator | ||||||
| n | 42 | 20 | ||||
| CICU admittance, days | 0.1 ± 0.484 | 0 | 0 | 0 | 0.1 | .325 |
| Ward admittance, days | 1.29 ± 1.402 | 1 [1-1] | 2.55 ± 2.012 | 2 [1-2,5] | –1.26 | < .001 |
| CICU cost | 100.35 ± 510.39 | 0 | 0 | 0 | 100.35 | 0.325 |
| Ward cost | 525.52 ± 572.99 | 408.74 [408.74-408.74] | 1042.29 ± 822.57 | 817.48 ± 408.74-1069.15] | –517.04 | < .001 |
| Total cost | 625.88 ± 960.19 | 408.74 [408.74-408.74] | 1042.29 ± 822.57 | 817.48 [408.74-1069.15] | –416.41 | < .001 |
| Pacemaker/cardiac resynchronizer | ||||||
| n | 65 | 50 | ||||
| CICU admittance, days | 0.03 ± 0.248 | 0 | 0 | 0 | 0.03 | .380 |
| Ward admittance, days | 0.57 ± 0.847 | 0 [0-1] | 1.68 ± 0.957 | 1 [1-2] | –1.11 | < .001 |
| CICU cost | 32.42 ± 261.39 | 0 | 0 | 0 | 32.42 | .380 |
| Ward cost | 232.67 ± 346.29 | 0 [0-408.74] | 686.68 ± 391.18 | 408.74 [408.74-817.48] | –454.01 | < .001 |
| Total cost | 265.09 ± 503.67 | 0 [0-408.74] | 686.68 ± 391.18 | 408.74 [408.74-817.48] | –421.59 | < .001 |
| Coronary interventional procedure | ||||||
| n | 61 | 41 | ||||
| CICU admittance, days | 0.03 ± 0.256 | 0 | 0.2 ± 0.546 | 0 | –0.17 | .005 |
| Ward admittance, days | 0.85 ± 1.062 | 1 [0-1] | 1.35 ± 0.625 | 1 [1-2] | –0.5 | < .001 |
| CICU cost | 34.55 ± 269.83 | 0 | 205.60 ± 575.68 | 0 | –171.05 | .005 |
| Ward cost | 348.43 ± 434.08 | 408.74 [0-408.74] | 553.29 ± 255.44 | 408.74 [408.74-817.48] | –204.86 | < .001 |
| Total cost | 382.98 ± 542.39 | 408.74 [0-408.74] | 758.90 ± 689.71 | 408.74 [408.74-817.48] | –375.92 | < .001 |
| Complex coronary interventional procedure | ||||||
| n | 110 | 54 | ||||
| CICU admittance, days | 0.71 ± 1.134 | 0.5 [0-1] | 0.5 ± 0.687 | 0.5 [0-1] | 0.21 | .270 |
| Ward admittance, days | 1.82 ± 2.97 | 1 [0.5-2) | 2.11 ± 1.653 | 2 [1-2.5] | –0.29 | < .001 |
| CICU cost | 751.97 ± 1195.18 | 526.86 [0-1.053.72] | 526.86 ± 723.70 | 526.86 [0-1053.72] | 225.11 | .270 |
| Ward cost | 745.02 ± 1214.16 | 408.74 [204.37-817.48] | 862.90 ± 675.68 | 817.48 [408.74-1021.85] | –117.88 | < .001 |
| Total cost | 1496.99 ± 2005.53 | 817.48 [731.23-1462.46] | 1389.76 ± 935.22 | 1226.22 [731.23-1871.20] | 107.23 | .154 |
| Noncoronary interventional procedure | ||||||
| n | 57 | 39 | ||||
| CICU admittance, days | 0.39 ± 0.778 | 0 [0-0.5] | 0.28 ± 0.410 | 0 [0-0.5] | 0.11 | .939 |
| Ward admittance, days | 1.58 ± 1.097 | 1 [1-2] | 2.41 ± 2.045 | 1.5 [1-3] | –0.83 | .009 |
| CICU cost | 415.94 ± 819.46 | 0 [0-790.29] | 297.20 ± 432.35 | 0 [0-526.86] | 118.74 | .939 |
| Ward cost | 645.38 ± 448.40 | 408.74 [408.74-817.48] | 985.17 ± 835.92 | 613.11 [408.74-1226.22] | –339.79 | .009 |
| Total cost | 1061.32 ± 1068.35 | 526.86 [408.74-1462.46] | 1282.37 ± 1070.56 | 1139.97 [408.74-1548.71] | –221.05 | .181 |
| Complex noncoronary interventional procedure | ||||||
| n | 28 | 32 | ||||
| CICU admittance, days | 1.34 ± 1.0 | 1 [1-2] | 1.16 ± 0.987 | 1 [0.5-1] | 0.18 | .260 |
| Ward admittance, days | 4.30 ± 3.083 | 4.5 [2-5.5] | 6.41 ± 5.604 | 5 [2.5-9] | –2.11 | .099 |
| CICU cost | 1411.23 ± 1054.24 | 1053.72 [1053.72-2107.44] | 1218.36 ± 1040.36 | 1053.72 [526.86-1053.72] | 192.87 | .260 |
| Ward cost | 1759.04 ± 1260.24 | 1839.33 [817.48-2.401.35] | 2618.49 ± 2290.78 | 2043.70 [1021.85-3678.66] | –859.45 | .099 |
| Total cost | 3170.27 ± 1881.70 | 3011.17 [1973.38-4328.32] | 3836.85 ± 2645.00 | 3183.67 [1629.33-5038.93] | –666.58 | .327 |
CDH, cardiology day hospital; CICU, cardiac intensive care unit; n, number of procedures.
Values are expressed as the mean ± standard deviation (second and fourth columns) and median [interquartile range] (third and fifth columns). The Savings column was obtained as the difference of means per procedure (in hospital stays or hospitalization cost, as appropriate) between the group attended in the CDH and the 2013 control group.
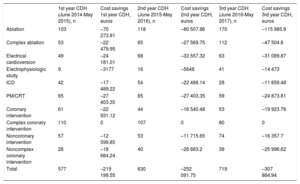
After the CDH became operational, there was an estimated saving of €219 199.55 in hospitalization expenditure, which remained stable or even increased in successive years (Table 4). Within the total amount saved, €103 804.29 (47%) was attributable to hospitalizations avoided the day before the procedure.
Scheduled Invasive Procedures and Estimated Hospitalization Cost Savings in the First 3 Years of CDH Operation
| 1st year CDH (June 2014-May 2015), n | Cost savings 1st year CDH, euros | 2nd year CDH (June 2015-May 2016), n | Cost savings 2nd year CDH, euros | 3rd year CDH (June 2016-May 2017), n | Cost savings 3rd year CDH, euros | |
|---|---|---|---|---|---|---|
| Ablation | 103 | –70 273.81 | 118 | –80 507.86 | 170 | –115 985.9 |
| Complex ablation | 53 | –22 479.95 | 65 | –27 569.75 | 112 | –47 504.8 |
| Electrical cardioversion | 49 | –24 181.01 | 68 | –33 557.32 | 63 | –31 089.87 |
| Electrophysiologic study | 9 | –3177 | 16 | –5648 | 41 | –14 473 |
| ICD | 42 | –17 489.22 | 54 | –22 486.14 | 28 | –11 659.48 |
| PM/CRT | 65 | –27 403.35 | 65 | –27 403.35 | 59 | –24 873.81 |
| Coronary intervention | 61 | –22 931.12 | 44 | –16 540.48 | 53 | –19 923.76 |
| Complex coronary intervention | 110 | 0 | 107 | 0 | 80 | 0 |
| Noncoronary intervention | 57 | –12 599.85 | 53 | –11 715.65 | 74 | –16 357.7 |
| Noncomplex coronary intervention | 28 | –18 664.24 | 40 | –26 663.2 | 39 | –25 996.62 |
| Total | 577 | –219 199.55 | 630 | –252 091.75 | 719 | –307 864.94 |
CDH, cardiology day hospital; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; PM, pacemaker.
As the expenditure for remodeling the area and purchasing the equipment needed was €12 000 and the cost of the permanent staff (2 nurses and 2 auxiliary nursing care technicians) was €135 746, the total balance was a saving of €71 453.5 in hospitalization expenditure. Hence, the start-up cost of the CDH was recouped in the first year of operation.
DISCUSSIONThis is the first study to analyze the activity and cost-effectiveness of a CDH. In our center, it was found to be a useful health care tool that significantly decreased the need for hospitalization related to scheduled procedures without detriment to the care provided, and produced a considerable saving in expenditure for hospital stays.
The document on standards and recommendations for care units in cardiology depatrtments12 has established that a CDH should be designed to allow patients to recover following an invasive procedure before they are discharged or referred back to their center of origin. Furthermore, an HF unit should have day hospital stations for administering medication. In the present case, the CDH was conceived as a multifunctional unit that carries out widely heterogeneous activity; therefore, it was decided that the staff should consist of specifically dedicated nursing personnel.
In the morning, the CHD mainly attends patients referred for procedures, and in the afternoon, patients requiring clinical examinations. As a large part of the activity involves care for HF patients, the fact that the staff is a stable team facilitates their involvement in the HF unit and their participation in activities such as patient instruction. The CDH has become an essential health care resource for administration of intravenous medication (diuretics, iron replacement therapy, antibiotics, and inotropic agents such as levosimendan) with proven safety of use in the ambulatory setting.15,16 The quality of the care provided is actually improved, and not only because patients do not have to be hospitalized, which can imply a disruption of family life. The CDH provides closer monitoring of this type of patient, prompt detection of complications, and fast treatment initiation before hospital or emergency room admission is needed.
There are no standards for the quality indicators evaluated here. However, the results obtained are useful for future comparisons and setting goals for improvement. With regard to the cancellation and suspension rates, it could be effective to call the patient 24 or 48hours before their scheduled visit as a reminder. This would also identify patients who cannot attend their appointment, and enable scheduling of another person in their place.17 Electrical cardioversion was the procedure associated with the highest suspension rate; 11 procedures (16%) were not carried out, indicating the need to design a plan for improvement. The reasons were the presence of sinus rhythm (n = 6), poor anticoagulation (n = 3), atrial appendage thrombus (n = 1), and the consideration that electrical cardioversion was not indicated (n = 1). It may be necessary to optimize the coordination with primary care to improve this indicator. This could include confirmation of adherence to anticoagulant therapy, measuring the international normalized ratio, or even a previous electrocardiography examination to avoid unnecessary visits by patients already in sinus rhythm.
Most of the invasive procedures scheduled do not require special preparation; therefore, patients can arrive the same day as the procedure. Centers equipped with hemodynamic and arrhythmia areas attend patients from other hospitals in the region and offer coverage for both scheduled and emergency processes. Thus, an area is needed where patients can wait and where care can be provided during the procedure and before patients can be transferred to their center of origin.18 If these areas are not available, hospital admission is often required, even though the procedure may be a low-risk one without complications. This can lead to problems of overcrowding, which makes it difficult to schedule other procedures or even admit emergency patients. The CDH not only decreases hospital stays in scheduled procedures, it also enables increased scheduling of ambulatory procedures.
Considerable cost savings were achieved by eliminating the preprocedure hospital stays in all types of scheduled procedures, even the more complex ones for which hospitalization cannot be avoided. The remaining savings were, to a great extent, the result of complete conversion of some invasive procedures to ambulatory procedures, for which postprocedure hospital monitoring could be prolonged without hospital admittance. Even though the performance of the CDH was lower during the first year of operation compared with successive years, the entire cost of implementing the day hospital was recouped in this period.
LimitationsThe operational aspects and activity described show the characteristics and particular needs of a cardiology department in a third level hospital. One such need arises from the overcrowding and delays in attention that sometimes occur in the outpatient clinic. The availability of a CHD allows timely assessment of patients attended in the emergency room and those with prompt hospital discharge, without delays and without additional overload in the outpatient clinic. Furthermore, the CDH is a component of the HF unit, where intravenous medical treatment is administered. In no case was the aim of this study to defend this model as the only one feasible. Any center contemplating the creation of a CDH should adapt it to the local circumstances and optimize the available resources.
With regard to complications, we were unable to collect those occurring in all patients referred from other centers and health areas; hence, the incidence of complications is likely larger than that recorded. Nor were we able to include those that did not require an urgent or additional visit to the hospital (eg, hematomas seen during the consultation for pacemaker review) as treatment for these was considered to be on an outpatient basis or they took place at a later time point.
The number of satisfaction surveys is small for the total size of the sample (7%) and the survey was conducted only in the last month studied. This limited sample could involve a bias, as the organization and experience of the CDH staff improved after a period in operation and this would undoubtedly affect the quality of the care. However, the perception is that the results are in accordance with the opinion of users attended in the CDH.
In the calculation of cost savings, only hospitalization expenditure was taken into account. The cost per process and other indirect costs were not included, as the procedures, in themselves, did not change: material, equipment, and human resources were the same whichever place patients were admitted. In addition, only scheduled ambulatory procedures were included in the estimation of avoided hospital stays and cost savings. In the absence of a CDH, other procedures, such as intravenous medical treatment, would often require hospital admittance. The impact in terms of cost savings derived from the total activity carried out by the CDH is likely greater than the amount estimated in this study.
CONCLUSIONSThe CDH is a quick-to-respond, dynamic health care tool that promotes a change in the organization of cardiologic hospital care. CHD implementation in our center has enabled conversion of two-thirds of the scheduled invasive procedures to ambulatory ones. This has considerably reduced procedure-related hospital stays, with consequent cost savings, without incurring a reduction in the quality of care. Furthermore, patients who need preferential attention that cannot be covered in the outpatient clinic can be attended with this model, and it provides support for the HF unit for administering intravenous treatment.
FUNDINGThis study was carried out in the scientific setting of the Cardiovascular Research Network and CIBERCV (Biomedical Research Network Center for Cardiovascular Diseases; Centro de Investigación Biomédica en Red de Enfermedades Cardiovasculares) of the Carlos III Health Institute of the Spanish Ministry of Economy, Industry, and Competitiveness. M. Gallego-Delgado received grants through the Carlos III Health Institute within the Action Plan for the promotion of clinical and translational research (contract for a professional who has passed specialized medical training).
CONFLICTS OF INTERESTNone declared.
- –
The CDH is an alternative to conventional hospitalization and a component of care units in cardiology services. Numerous invasive procedures performed in cardiology can be carried out on an ambulatory basis, with discharge on the same day as the procedure, and without hospital admittance. There are no other published studies to date reporting the economic impact of implementing a CDH.
- –
This is the first study to analyze the economic impact of a CDH.
- –
The cost of implementing the CDH was recouped in its first year of operation, and it achieved a considerable saving in hospitalization expenditure. Furthermore, the safety of performing invasive procedures on an ambulatory basis was verified, there was no reduction in the quality of the care provided, and patients expressed a high degree of satisfaction with the CDH.
- –
The availability of a CDH allows appropriate care for patients with complex clinical conditions, such as HF, who require frequent examinations and administration of treatments, which cannot be covered in outpatient clinics.
We thank Desiré Rodríguez Bezos and Sabiela Ojeda Enrique de Boston Scientific Iberica S.A. for their advice and review of the manuscript.