Thoracic aortic dissection (TAD) is infrequent in young people and its characteristics differ from those in the adult population. This study aimed to analyze the clinical and pathological characteristics of sudden death due to TAD in people aged 1 to 35 years.
MethodsMulticenter population-based study based on forensic autopsies conducted in the provinces of Biscay (1991-2016), Valencia (2000-2016), and Seville (2004-2016).
ResultsWe identified 35 individuals with sudden death due to TAD (80% males), with a mean age of 29±5 years. The incidence was 0.09/100 000 inhabitants/y. Eighteen persons had at least 1 risk factor for TAD, and this figure increased to 29 when postmortem findings were included: congenital heart disease (n=16), suspicion of familial TAD (n=11), cocaine use (n=6), and hypertension (n=5). Twenty-four individuals, 12 with at least 1 risk factor, had prodromal symptoms, and 16 of them visited their physician, but TAD was not suspected in any of them. The most frequent symptom was chest pain (n=12). The main autopsy findings were cystic degeneration of the media (n=27), dilatation of the ascending aorta (n=21), cardiac hypertrophy (n=20), and bicuspid aortic valve (n=14).
ConclusionsThe incidence of sudden death due to TAD in young people was very low. The most frequent risk factors were congenital heart disease followed by suspicion of familial TAD and cocaine use. TAD should be included in the differential diagnosis of chest pain in young people, mainly male patients with at least 1 risk factor.
Keywords
Thoracic aortic dissection (TAD) is an emergency clinical situation with high mortality; hence, early diagnosis and treatment are essential for a favorable prognosis. The condition usually affects individuals older than 50 years, and the main risk factor is hypertension. It usually begins with severe chest pain of sudden onset, thus sometimes allowing the condition to be diagnosed in life.1 Occasionally, sudden death (SD) is the first manifestation of the disease.
In young people, TAD is extremely rare,2–5 and in persons younger than 35 years it is a rare cause of sudden cardiac death (SCD).6–10 This age group is considered to have unique clinical and pathologic characteristics compared with adults, as well as unusual risk factors and an atypical presentation. The most important risk factors are connective tissue abnormalities and congenital cardiovascular anomalies.2–5
Only a few clinical series of TAD in young people have been published,2–5 and most reports describe isolated cases retrospectively.11–21 To our knowledge, there are no published series of SCD secondary to TAD in young people and, therefore, the characteristics of this group are poorly defined.
The purpose of our forensic study was to analyze the epidemiologic, clinical, and pathologic characteristics and the risk factors of SD due to TAD in a population aged 1 to 35 years.
METHODSLegislation and Definition of Sudden DeathA multicenter population-based study was conducted of the forensic autopsies of victims aged 1 to 35 years who had died suddenly due to TAD.
According to the definition of SD, death occurs naturally, unexpectedly, and within 6hours of symptom onset in persons in apparent good health carrying out their normal activities at the time of the fatal event. The definition also includes unwitnessed deaths in which the victim was last seen alive and in good health within 24hours prior to death.22
Study Population. Sample SelectionBecause SCD due to TAD is rare in young people, this multicenter study was designed to include the forensic services of the provinces of Biscay, Seville, and Valencia. In each province, a single forensic service performs all court-ordered autopsies for deaths occurring within their borders. The 3 forensic services created an SD registry of individuals aged 35 years or younger, and the time period analyzed covered from the date the registry was created in each province (Biscay, 1991; Valencia, 2000; Seville, 2004) up to and including 2016. The study analyzed SD registry data from the 3 forensic services for victims up to age 35 years to identify the total number of cases of SCD and the number of SCDs due of TAD. Additionally, cases of SCD due to TAD at all ages were identified. Demographic, clinical, and pathologic variables were collected for all SCD due to TAD up to age 35 years.
Autopsy ProtocolAutopsies were performed by trained forensic pathologists according to international recommendations.22,23 We retrospectively collected information on medical history, inspection of the place of death, external examination, complete autopsy with macroscopic and microscopic examination, and toxicological analysis of blood, urine, and vitreous humor.
The diameter of the ascending aorta was measured at a distance of 1.5-2cm from the sinotubular junction. There are no anatomic pathology criteria to define dilatation of the aorta. Postmortem studies established that the mean diameter of the ascending aorta was 2.2cm.24 Based on this datum and the mean age of our sample, aortic dilatation was diagnosed when the diameter was ≥ 3.5cm (1.5-fold the normal value). Coronary atherosclerosis was considered severe when vascular lumen stenosis was> 75% and moderate between 50% and 75%.22 The heart was considered to have an increased weight, indicative of left ventricular hypertrophy, when the value was more than 20% above the estimated weight for the victim's body weight.25
Epidemiological and Statistical AnalysisThe incidence of SD due to TAD in persons aged 1 to 35 years subject to forensic autopsy were calculated based on 2011 population census data from the National Institute of Statistics. The population aged 1 to 35 years in Biscay was 411 220, 1 057 166 in Valencia, and 861 358 in Seville. Incidences were calculated for each sex and as a whole, and the relative risk between the sexes and the 95% confidence interval were confirmed. The numerator was the number of forensic cases of SD due to TAD in persons aged 1 to 35 years, and the denominator was the total population aged 1 to 35 years in each province, multiplied by the number of years analyzed in each province. Continuous variables are expressed as mean±standard deviation with the percentage and range. SPSS for Windows, version 21.0, was used for the statistical analysis.
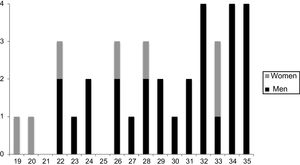
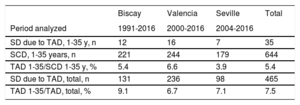
RESULTSDemographic and Epidemiologic DataA total of 35 cases of TAD were identified in the population aged 1 to 35 years; 80% were male, and all were Caucasian. The mean age was 29±5 (19-35) years (males, 30±4 years; females, 26±5 years) (Figure 1). TAD accounted for 5.4% of all forensic autopsies for SCD in young people and 7.5% of SCD due to TAD in all age brackets (Table 1). According to the forensic autopsy data, the incidence of SD due to TAD in the population aged 1 to 35 years was 0.09/100 000 inhabitants/y. The relative risk was 4-fold higher in males (95% confidence interval, 2.3-19.2).
Distribution of Cases of SD Due to TAD in Individuals Aged 1-35 Years Among All Cases of SCD in Individuals Aged 1 to 35 Years and All Cases of SD Due to TAD at All Ages. Autopsy Data From the Forensic Pathology Services of the Provinces of Biscay, Valencia, and Seville
| Biscay | Valencia | Seville | Total | |
|---|---|---|---|---|
| Period analyzed | 1991-2016 | 2000-2016 | 2004-2016 | |
| SD due to TAD, 1-35 y, n | 12 | 16 | 7 | 35 |
| SCD, 1-35 years, n | 221 | 244 | 179 | 644 |
| TAD 1-35/SCD 1-35 y, % | 5.4 | 6.6 | 3.9 | 5.4 |
| SD due to TAD, total, n | 131 | 236 | 98 | 465 |
| TAD 1-35/TAD, total, % | 9.1 | 6.7 | 7.1 | 7.5 |
SCD; sudden cardiac death; SD, sudden death; TAD, thoracic aortic dissection.
Most (74%) deaths were out-of-hospital, while the rest occurred during ambulance transfer or very soon after admission to the emergency room. Death usually occurred at home (60%), during a routine activity, at rest (46%), or while sleeping (11%) (Table 2).
Clinical Data for SD Due to TAD in Individuals Aged 1 to 35 Years (n=35)
| n (%) | |
|---|---|
| Origin of cadaver | |
| Out-of-hospital (cadaver release) | 26 (74) |
| Hospital (dead on arrival or early death in emergency room, undiagnosed) | 9 (26) |
| Place of symptom onset | |
| Home | 21 (60) |
| Place of leisure | 5 (14) |
| Work | 3 (8) |
| Public site | 2 (5) |
| Unknown | 4 (11) |
| Activity | |
| Rest | 16 (46) |
| Sleep | 4 (11) |
| Physical activity | 3 (8) |
| Unknown | 12 (34) |
| Risk factors for TAD | 18 (51)a |
| Family history | 5 (14) |
| Medical history | 10 (28)b |
| Hypertension | 5 |
| Congenital heart diseases | 4 |
| Hereditary connective system disorders | 2 |
| Severe kidney disease (dialysis) | 1 |
| Cocaine use | 5 (14) |
| Symptoms prior to death | 24 (68) |
| Chest pain | 12 |
| Lower back pain | 3 |
| Digestive symptoms | 3 |
| Other | 6 |
| No | 9 |
| Unknown | 2 |
SD, sudden death; TAD, thoracic aortic dissection.
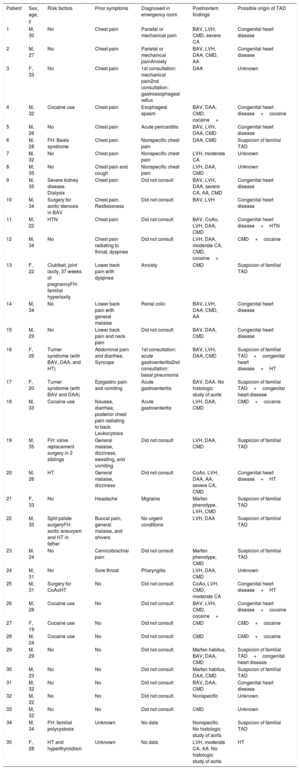
Eighteen (51%) people had a TAD-related risk factor: personal medical history (n=10), illicit drug use (n=5), or family history (n=5) (Table 2 and Table 3). Before death, 24 patients had some symptoms, with chest pain being the most common (n=12); 16 (67%) patients had visited a physician, but none suspected TAD and the diagnoses were extremely varied (Table 3).
Demographic, Clinical, and Pathologic Characteristics of Cases of Sudden Death Due to TAD (n=35)
| Patient | Sex, age, y | Risk factors | Prior symptoms | Diagnosed in emergency room | Postmortem findings | Possible origin of TAD |
|---|---|---|---|---|---|---|
| 1 | M, 30 | No | Chest pain | Parietal or mechanical pain | BAV, LVH, CMD, severe CA | Congenital heart disease |
| 2 | M, 27 | No | Chest pain | Parietal or mechanical painAnxiety | BAV, LVH, DAA, CMD, AA | Congenital heart disease |
| 3 | F, 33 | No | Chest pain | 1st consultation: mechanical pain2nd consultation: gastroesophageal reflux | DAA | Unknown |
| 4 | M, 32 | Cocaine use | Chest pain | Esophageal spasm | BAV, DAA, CMD, cocaine+ | Congenital heart disease+cocaine |
| 5 | M, 26 | No | Chest pain | Acute pericarditis | BAV, LVH, DAA, CMD | Congenital heart disease |
| 6 | M, 28 | FH: Beals syndrome | Chest pain | Nonspecific chest pain | DAA, CMD | Suspicion of familial TAD |
| 7 | M, 32 | No | Chest pain | Nonspecific chest pain | LVH, moderate CA | Unknown |
| 8 | M, 35 | No | Chest pain and cough | Nonspecific chest pain | LVH, DAA, CMD | Unknown |
| 9 | M, 35 | Severe kidney disease. Dialysis | Chest pain | Did not consult | BAV, LVH, DAA, severe CA, AA, CMD | Congenital heart disease |
| 10 | M, 34 | Surgery for aortic stenosis in BAV | Chest pain. Restlessness | Did not consult | BAV, LVH | Congenital heart disease |
| 11 | M, 22 | HTN | Chest pain | Did not consult | BAV, CoAo, LVH, DAA, CMD | Congenital heart disease+HTN |
| 12 | M, 34 | No | Chest pain radiating to throat, dyspnea | Did not consult | LVH, DAA, moderate CA, CMD, cocaine+ | CMD+cocaine |
| 13 | F, 22 | Clubfeet, joint laxity, 37 weeks of pregnancyFH: familial hyperlaxity | Lower back pain with dyspnea | Anxiety | CMD | Suspicion of familial TAD |
| 14 | M, 34 | No | Lower back pain with general malaise | Renal colic | BAV, LVH, DAA, CMD, AA | Congenital heart disease |
| 15 | M, 29 | No | Lower back pain and neck pain | Did not consult | BAV, DAA, CMD | Congenital heart disease |
| 16 | F, 26 | Turner syndrome (with BAV, DAA, and HT) | Abdominal pain and diarrhea. Syncope | 1st consultation: acute gastroenteritis2nd consultation: basal pneumonia | BAV, LVH, DAA, CMD | Suspicion of familial TAD+congenital heart disease+HT |
| 17 | F, 20 | Turner syndrome (with BAV and DAA) | Epigastric pain and vomiting | Acute gastroenteritis | BAV, DAA. No histologic study of aorta | Suspicion of familial TAD+congenital heart disease |
| 18 | M, 33 | Cocaine use | Nausea, diarrhea, posterior chest pain radiating to back. Leukocytosis | Acute gastroenteritis | LVH, DAA, CMD | CMD+cocaine |
| 19 | M, 35 | FH: valve replacement surgery in 2 siblings | General malaise, dizziness, sweating, and vomiting | Did not consult | LVH, DAA, CMD | Suspicion of familial TAD |
| 20 | M, 26 | HT | General malaise, dizziness | Did not consult | CoAo, LVH, DAA, AA, severe CA, CMD | Congenital heart disease+HT |
| 21 | F, 33 | No | Headache | Migraine | Marfan phenotype, LVH, CMD | Suspicion of familial TAD |
| 22 | M, 35 | Split palate surgeryFH: aortic aneurysm and HT in father | Buccal pain, general malaise, and shivers | No urgent conditions | LVH, DAA | Suspicion of familial TAD |
| 23 | M, 24 | No | Cervicobrachial pain | Did not consult | Marfan phenotype, CMD | Suspicion of familial TAD |
| 24 | M, 31 | No | Sore throat | Pharyngitis | LVH, DAA, CMD | Unknown |
| 25 | M, 31 | Surgery for CoAoHT | No | Did not consult | CoAo, LVH, CMD, moderate CA | Congenital heart disease+HT |
| 26 | M, 28 | Cocaine use | No | Did not consult | BAV, LVH, CMD, cocaine+ | Congenital heart disease+cocaine |
| 27 | F, 19 | Cocaine use | No | Did not consult | CMD | CMD+cocaine |
| 28 | M, 24 | Cocaine use | No | Did not consult | CMD | CMD+cocaine |
| 29 | M, 29 | No | No | Did not consult | Marfan habitus, BAV, DAA, CMD | Suspicion of familial TAD+congenital heart disease |
| 30 | M, 23 | No | No | Did not consult | Marfan habitus, DAA, CMD | Suspicion of familial TAD |
| 31 | M, 32 | No | No | Did not consult | BAV, DAA, CMD | Congenital heart disease |
| 32 | M, 22 | No | No | Did not consult | Nonspecific | Unknown |
| 33 | M, 32 | No | No | Did not consult | CMD | Unknown |
| 34 | M, 34 | FH: familial polycystosis | Unknown | No data | Nonspecific. No histologic study of aorta | Suspicion of familial TAD |
| 35 | F, 28 | HT and hyperthyroidism | Unknown | No data | LVH, moderate CA, AA. No histologic study of aorta | HT |
AA, aortic atherosclerosis; BAV, bicuspid aortic valve; CA, coronary atherosclerosis; CMD, cystic medial degeneration; CoAo, coarctation of the aorta; DAA, dilatation of the ascending aorta; F, female; FH, family history; HTN, hypertension; LVH, left ventricular hypertrophy; M, male; TAD, thoracic aortic dissection.
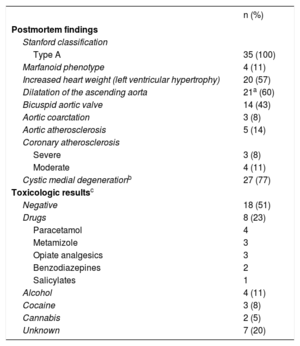
All dissections were Stanford type A with pericardial rupture. In no cases did dissection affect only the descending aorta (Stanford type B), although in 6 of 20 for whom this datum was known, dissection extended to the abdominal aorta. The most common macroscopic findings were dilatation of the ascending aorta (60%), increased heart weight (57%), bicuspid aortic valve (BAV) (43%), Marfan phenotype (11%), and aortic coarctation (8%). The mean heart weight was 470±135g, 32% higher than expected for body weight (355±56g). The mean diameter of the ascending aorta was 4±1.3cm, and it was>5cm in 4 cases. The intimal tear was most often single (86%), horizontal (57%), and at a mean distance of 2.10cm from the sinotubular junction. In 4 cases, there were 2 tears, and in 1, there were 3 in the ascending aorta, the aortic arch, and the subclavian outflow. The histopathologic study showed cystic medial degeneration (CMD) in 27 (77%) participants. In 3 cases, no histologic study was performed on the aorta and, therefore, this datum is unknown.
The toxicologic analysis detected drugs without cardiovascular toxicity in 8 cases, usually analgesics; alcohol in 4 (2 with alcoholemia<0.5g/L), cocaine in 3, and cannabis in 2 (Table 4). Cocaine may have been a predisposing factor in 6 males: 5 known users (2 with positive toxicology) and 1 other case, with no known use, in which cocaine was detected in the toxicologic analysis. In these 6 cases, the histologic study revealed CMD and in 2, BAV (Table 3 and Table 4).
Postmortem Findings and Toxicologic Results for SD due to TAD in Individuals Aged 1 to 35 Years (n=35)
| n (%) | |
|---|---|
| Postmortem findings | |
| Stanford classification | |
| Type A | 35 (100) |
| Marfanoid phenotype | 4 (11) |
| Increased heart weight (left ventricular hypertrophy) | 20 (57) |
| Dilatation of the ascending aorta | 21a (60) |
| Bicuspid aortic valve | 14 (43) |
| Aortic coarctation | 3 (8) |
| Aortic atherosclerosis | 5 (14) |
| Coronary atherosclerosis | |
| Severe | 3 (8) |
| Moderate | 4 (11) |
| Cystic medial degenerationb | 27 (77) |
| Toxicologic resultsc | |
| Negative | 18 (51) |
| Drugs | 8 (23) |
| Paracetamol | 4 |
| Metamizole | 3 |
| Opiate analgesics | 3 |
| Benzodiazepines | 2 |
| Salicylates | 1 |
| Alcohol | 4 (11) |
| Cocaine | 3 (8) |
| Cannabis | 2 (5) |
| Unknown | 7 (20) |
SD, sudden death; TAD, thoracic aortic dissection.
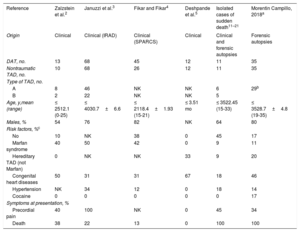
There are few hospital series of TAD in children and young people.2–5 Although there are some isolated published reports of SD due to TAD in persons aged 35 years or younger,11–21 our study is the first series specific to this age group. Its importance lies in the fact that the cases were out-of-hospital SDs not diagnosed antemortem, for which forensic autopsy was available. The patient population had not been included in clinical studies and provides valuable additional information to further our understanding of this rare condition. Table 5 and Table 6 compare our findings with the largest published clinical series of TAD.
Main Clinical Characteristics of TAD Series in Individuals Younger Than 35 Years
| Reference | Zalzstein et al.2 | Januzzi et al.3 | Fikar and Fikar4 | Deshpande et al.5 | Isolated cases of sudden death11–21 | Morentin Campillo, 2018a |
|---|---|---|---|---|---|---|
| Origin | Clinical | Clinical (IRAD) | Clinical (SPARCS) | Clinical | Clinical and forensic autopsies | Forensic autopsies |
| DAT, no. | 13 | 68 | 45 | 12 | 11 | 35 |
| Nontraumatic TAD, no. | 10 | 68 | 26 | 12 | 11 | 35 |
| Type of TAD, no. | ||||||
| A | 8 | 46 | NK | NK | 6 | 29b |
| B | 2 | 22 | NK | NK | 5 | |
| Age, y,mean (range) | ≤ 2512.1 (0-25) | ≤ 4030.7±6.6 | ≤ 2118.4±1.93 (15-21) | ≤ 3.51 mo | ≤ 3522.45 (15-33) | ≤ 3528.7±4.8 (19-35) |
| Males, % | 54 | 76 | 82 | NK | 64 | 80 |
| Risk factors, %c | ||||||
| No | 10 | NK | 38 | 0 | 45 | 17 |
| Marfan syndrome | 40 | 50 | 42 | 0 | 9 | 11 |
| Hereditary TAD (not Marfan) | 0 | NK | NK | 33 | 9 | 20 |
| Congenital heart diseases | 50 | 31 | 31 | 67 | 18 | 46 |
| Hypertension | NK | 34 | 12 | 0 | 18 | 14 |
| Cocaine | 0 | 0 | 0 | 0 | 0 | 17 |
| Symptoms at presentation, % | ||||||
| Precordial pain | 40 | 100 | NK | 0 | 45 | 34 |
| Death | 38 | 22 | 13 | 0 | 100 | 100 |
IRAD, International Registry of Acute Aortic Dissection; NK, not known; SPARCS, Statewide Planning and Research Cooperative System (New York State Department of Health patient database); TAD, thoracic aortic dissection.
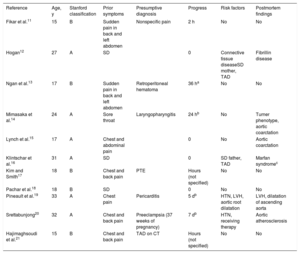
Main Characteristics of Isolated Cases of SD Due to TAD in Individuals Younger Than 35 Years (Autopsy-based Studies)
| Reference | Age, y | Stanford classification | Prior symptoms | Presumptive diagnosis | Progress | Risk factors | Postmortem findings |
|---|---|---|---|---|---|---|---|
| Fikar et al.11 | 15 | B | Sudden pain in back and left abdomen | Nonspecific pain | 2 h | No | No |
| Hogan12 | 27 | A | SD | 0 | Connective tissue diseaseSD mother, TAD | Fibrillin disease | |
| Ngan et al.13 | 17 | B | Sudden pain in back and left abdomen | Retroperitoneal hematoma | 36 ha | No | No |
| Mimasaka et al.14 | 24 | A | Sore throat | Laryngopharyngitis | 24 hb | No | Turner phenotype, aortic coarctation |
| Lynch et al.15 | 17 | A | Chest and abdominal pain | 0 | No | Aortic coarctation | |
| Klintschar et al.16 | 31 | A | SD | 0 | SD father, TAD | Marfan syndromec | |
| Kim and Smith17 | 18 | B | Chest and back pain | PTE | Hours (not specified) | No | No |
| Pachar et al.18 | 18 | B | SD | 0 | No | No | |
| Pineault et al.19 | 33 | A | Chest pain | Pericarditis | 5 db | HTN, LVH, aortic root dilatation | LVH, dilatation of ascending aorta |
| Srettabunjong20 | 32 | A | Chest and back pain | Preeclampsia (37 weeks of pregnancy) | 7 db | HTN, receiving therapy | Aortic atherosclerosis |
| Hajimaghsoudi et al.21 | 15 | B | Chest and back pain | TAD on CT | Hours (not specified) | No | No |
CT, computed tomography; HT, hypertension, LVH, left ventricular hypertrophy; PTE, pulmonary thromboembolism; SD, sudden death; TAD, thoracic aortic dissection.
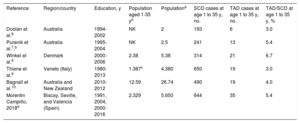
Although TAD is rare in young people,2–5 there are no epidemiologic data on the incidence of this condition. In our forensic autopsy-based series, the incidence of mortality for SD due to TAD between age 1 and 35 years was very low (0.09/100 000 inhabitants/y). The percentage of TAD in large SCD series of victims aged 1 to 35 years, based on postmortem studies, ranges between 3% and 7% (Table 7),6–10 and our study falls within this range (5.4%). The percentage of SCD due to TAD in young people compared with TAD at all age brackets was similar to that reported by Januzzi et al.3 (7% of TAD in all persons younger than 40 years), and the proportion in participants up to age 19 years was similar to the study by Fikar and Fikar4 (0.37% of people younger than age 21 years). As in adults,1 TAD in youth was more common in males (75%),1,3,4 and in our series, the relative risk was 4-fold higher for males.
Demographic and Epidemiologic Data in the Main SCD Series Among Individuals Aged 1 to 35 years Compared With the Current Study
| Reference | Region/country | Education, y | Population aged 1-35 ya | Populationa | SCD cases at age 1 to 35 y, no. | TAD cases at age 1 to 35 y, no. | TAD/SCD at age 1 to 35 y, % |
|---|---|---|---|---|---|---|---|
| Doolan et al.6 | Australia | 1994-2002 | NK | 2 | 193 | 6 | 3.0 |
| Puranik et al.7,b | Australia | 1995-2004 | NK | 2.5 | 241 | 13 | 5.4 |
| Winkel et al.8 | Denmark | 2000-2006 | 2.38 | 5.38 | 314 | 21 | 6.7 |
| Thiene et al.9 | Veneto (Italy) | 1980-2013 | 1.387c | 4.380 | 650 | 19 | 3.0 |
| Bagnall et al.10 | Australia and New Zealand | 2010-2012 | 12.59 | 26.74 | 490 | 19 | 4.0 |
| Morentin Campillo, 2018d | Biscay, Seville, and Valencia (Spain) | 1991, 2004, 2000-2016 | 2.329 | 5.650 | 644 | 35 | 5.4 |
SCD; sudden cardiac death; TAD, thoracic aortic dissection.
At least 1 risk factor was detected in 51% of our study participants, with this figure rising to 83% when postmortem findings (marfanoid phenotype, cardiovascular abnormalities, and presence of cocaine in the toxicologic analysis) were also considered (Table 3 and Table 5). In clinical series, risk factors are present in 62%4 to 90%2 of youth. A review of isolated cases of SD due to TAD showed that a risk factor was found in 60% during the postmortem study; however, most were not diagnosed during the victim's lifetime (Table 5).11–21 In the Italian series of Veneto,9 a congenital substrate was identified in the 19 cases.
The predisposing factors were different in young people than in adults. Hypertension and atherosclerosis was present in 75% and 30% of adults, respectively.1,3 In our series, 5 (14%) patients had been diagnosed with hypertension (3 with aortic coarctation), a level below that of the series reported by Januzzi et al.3 (34%). No cases in our study had a history of atherosclerosis, although the autopsy revealed aortic or coronary atherosclerosis in 9 cases.
Congenital Heart DiseasesThe frequency of congenital heart disease in TAD among children and young people was 46% (n=16) in our series (Table 3), with previous studies reporting rates of 30% to 50%.2–4 One of the most important was BAV,26,27 observed in the autopsy of 14 (43%) cases. In BAV, the risk of dissection is 5- to 18-fold higher than in the case of the tricuspid aortic valve.26 Another anomaly associated with TAD was aortic coarctation,27 detected in our series in 3 cases with a history of hypertension. Cardiac surgery on the aortic valve, a prior condition reported in 1 case, was also related to a higher risk of TAD.3
Hereditary DisordersHereditary connective system disorder-related TAD usually occurs in young people, and Marfan syndrome is the best known.27 In clinical series, its frequency is between 40% and 50%.2,4
In our series, 11 (31%) cases had a possible predisposing genetic substrate (Table 3). In 4 individuals, the autopsy reported marfanoid phenotype, none diagnosed in life. A review of the 11 isolated cases of SD due to TAD with a postmortem study (Table 5 and Table 611–21) found only 1 case.16 This lower frequency of Marfan syndrome in forensic series may be due to greater clinical suspicion, thus making it more likely for the condition to be diagnosed during the person's lifetime. In addition, 2 patients had been diagnosed with Turner syndrome. Because TAD is associated with BAV, dilatation of the ascending aorta, and aortic coarctation, it is 6-fold more common in Turner syndrome than in the general population and tends to occur in childhood and adolescence. This complication accounted for 8% of deaths in Turner syndrome.28
Another 5 participants with a family history indicating a genetic basis could be included (Table 3): 1 with a family history of Beals syndrome (case 6), another suspected to have Ehlers-Danlos syndrome (case 13), and a third suspected to have Loeys-Dietz syndrome (case 22).27 The fourth patient had a family history of autosomal dominant polycystic kidney disease (case 34). Only a few cases of this association have been described in individuals younger than age 35 years.29 The fifth case had a family history of valve disease, and the postmortem study revealed dilatation of the ascending aorta and CMD (case 19).
The high frequency of hereditary risk factors highlights the importance of identifying patients with underlying genetic mutations.30 A recent article has described the characteristics of 4 cases with their molecular genetic basis.5 During autopsy, it is recommended that samples be taken (blood in EDTA at –80°C) for genetic studies. A family study is also recommended in the current scientific guidelines.22 By including multidisciplinary studies when investigating SCD, the number of TAD cases of unknown origin are expected to drop due to family cardiologic assessment and due to advances in cardiovascular genetics.
Substance AbuseCocaine use is associated with numerous cardiovascular complications and with SCD.31 Recent cocaine use leads to an increased risk of SCD of up to 4-fold32 among young people and, although rare, is another significant risk factor for TAD.33 In a study by Hsue et al.,33 14 of 38 cases of TAD were associated with recent cocaine use, particularly in youth. In our study, cocaine was a risk factor in 6 (17%) participants, a much higher frequency than that reported in surveys on cocaine use among the general population34; 2 of the 6 cases had BAV; however, the presence of CMD in all of them was more relevant. These data indicate that cocaine may have an effect on a weakened aortic wall and increase the risk of dissection. The frequency of cannabis use was 8%, an expected level in view of cannabis use and the long mean half-life of the Spanish population.34 The relatively high presence of analgesic drugs in the toxicologic analysis is not surprising, given the prevalence of pain symptoms prior to death.
Clinical PresentationEarly diagnosis of TAD is clearly important in view of its high immediate mortality. Severe chest pain of rapid onset is the most common symptom of presentation1,3; 12 (34%) victims had this symptom and 8 consulted a physician, although none suspected TAD even though risk factors were recorded in the history of 2. From a medical and legal point of view, this diagnostic error could lead to claims being filed for medical malpractice. Likewise, 3 of the 4 individuals with chest pain who did not consult a physician had risk factors. Failure to suspect this condition in persons with chest pain and with risk factors for TAD when they visit the emergency room and the failure of some persons to consult the emergency room are certainly an important health issue.
Our data indicate that TAD should be included in the differential diagnosis of young patients with precordial pain and a concomitant illness, particularly in the presence of hypertension or left ventricular hypertrophy on electrocardiography.
On many occasions, the course of TAD is characterized by a nonspecific picture with atypical symptoms (34% had symptoms other than chest pain before death) or a cataclysmic onset (26% had no previous symptoms). In both situations, a high degree of clinical suspicion is needed and, consequently, diagnosis is extremely difficult. Roberts et al.35 suspected that 23% cases of TAD are not clinically diagnosed (due to the low rate of clinical autopsies), a supposition that is also supported by some forensic series.36
Anatomic PathologyStanford type A dissections, detected in all our cases, also predominate at these ages and, as in the case of adults, onset consists of SD more often than in the case of type B.37 Conversely, Januzzi et al.3 reported that up to 32% of TAD in young people only affected the descending aorta. This difference could be explained by the type of sample (forensic vs hospital).
Increased heart weight indicating left ventricular hypertrophy was detected in 57% of cases, a very high figure for a young population. The condition appears to have several causes, among them congenital heart disease (mainly BAV and, to a lesser extent, aortic coarctation), hypertension, obesity, severe kidney disease, and cocaine use.
Some patients with TAD have been reported to have dilatation of the ascending aorta, which showed a high prevalence (60%) in our study but which had only been recorded as medical history for 1 patient diagnosed with Turner syndrome. This finding should be interpreted with caution from the clinical standpoint because there is no adequate correlation between postmortem values for aorta diameter and values obtained from living patients by imaging techniques.
In 27 (77%) cases, we observed CMD, a characteristic but poorly specific sign of various hereditary connective tissue disorders. This term has been used in a confusing manner, and recent efforts have unified the criteria used to recognize characteristic histopathologic patterns for certain genetic aortic syndromes, for the purpose of distinguishing between the various etiologies.38
LimitationsDue to the retrospective nature of the study, in the oldest autopsies the aorta was not measured precisely; hence, the grade of dilatation might not have been accurately established. Furthermore, there is no adequate correlation between postmortem values for aorta diameter and values obtained from living patients by imaging techniques. Although all dissections were Stanford type A, in some cases we could not rule out extension of the dissection to the descending aorta. Last, the study analyzed a small number of fatal cases of TAD in a series of forensic autopsies; however, our results appear to confirm and to add new information to reports from previous clinical studies about this rare condition. Therefore, these data are useful from the clinical standpoint and can be cautiously extrapolated to the general population.
CONCLUSIONSThe incidence of SCD due to TAD in individuals younger than 35 years is very low, and the population at greatest risk are young males. The most common risk factor is congenital heart disease, a condition often not diagnosed during the victim's lifetime. Familial TAD syndrome was suspected in almost one third of cases. Another significant risk factor is cocaine use. In one third of cases, SD was preceded by symptoms of chest pain. Consequently, SD should be included among the possible diagnoses of severe precordial pain once an ischemic origin has been excluded. On occasions, TAD can be diagnosed, although a high degree of clinical suspicion is needed, particularly among younger patients. The inclusion of forensic sources in acute aortic disease registries, such as the RESA (Spanish Registry of Acute Aortic Syndrome),1 would provide useful data to supplement hospital data.
CONFLICTS OF INTERESTNone declared.
- –
TAD generally affects people older than 50 years. In young people, this is a rare cause of SCD. Few series have investigated the problem of TAD in patients younger than 35 years. This age bracket has distinct clinical and pathologic characteristics from adults, with unusual risk factors and atypical presentation.
- –
The incidence of SCD due to TAD up to age 35 years is very low, and the condition mainly affects young males. The most important risk factor is congenital heart disease, followed by familial TADs and cocaine use. The differential diagnosis of chest pain in young people should include TAD, particularly when there are risk factors. Forensic study can more clearly define the characteristics of TAD and be useful to identify the index case and to enhance subsequent cardiologic and genetic studies of family members.
We would like thank Dr Covadonga Audicana for her assistance with the epidemiologic and statistical analysis.