There is a paucity of data on prehospital cardiac arrest in Spain. Our aim was to describe the incidence, patient characteristics, and outcomes of out-of-hospital emergency care for this event.
MethodsWe conducted a retrospective analysis of a prospective registry of cardiopulmonary arrest handled by an out-of-hospital emergency service between January 2008 and December 2012. The registry included all patients considered to have a cardiac etiology as the cause of arrest, with a descriptive analysis performed of general patient characteristics and factors associated with good neurologic outcome at hospital discharge.
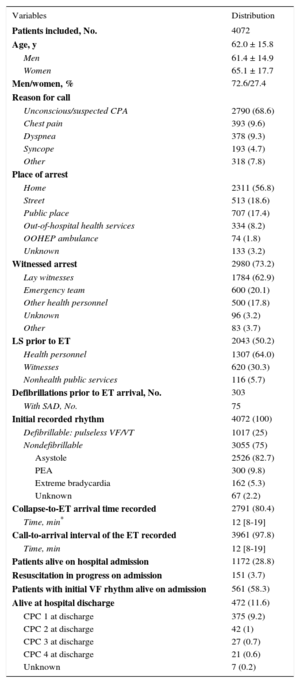
ResultsA total of 4072 patients were included, with an estimated incidence of 14.6 events per 100000 inhabitants and year; 72.6% were men. The mean age was 62.0 ± 15.8 years, 58.6% of cases occurred in the home, 25% of patients had initial defibrillable rhythm, 28.8% of patients arrived with a pulse at the hospital (58.3% of the group with defibrillable rhythm), and 10.2% were discharged with good neurologic outcome. The variables associated with this recovery were: witnessed arrest (P=.04), arrest witnessed by emergency team (P=.005), previous life support (P=.04), initial defibrillable rhythm (P=.0001), and performance of a coronary interventional procedure (P=.0001).
ConclusionsMore than half the cases of sudden cardiac arrest occur at home, and the population was found to be relatively young. Although recovery was satisfactory in 1 out of every 10 patients, there is a need for improvement in the phase prior to emergency team arrival. Coronary interventional procedures had an impact on patient prognosis.
Keywords
Cardiovascular diseases are the main cause of death in Spain.1 Among them, there are high rates of ischemic heart disease with sudden cardiac death (SCD) as the most common form of death.2,3 Overall estimates of the incidence of cardiopulmonary arrest (CPA) in general and of SCD in particular vary widely in every country,4 mainly because the estimates are based on calculations that use different information sources, which can entail a certain margin of error.5 Similar to incidence, survival after out-of-hospital CPA varies considerably between countries with similar health care structures.6,7 Consequently, it is not uncommon to express CPA incidence and outcomes in relation to out-of-hospital emergency service care.8
Around 8 out of every 10 sudden cardiac arrests are known to be of cardiac etiology (or more generally, cardiovascular) and could be labeled as SCD.9,10 Hence, out-of-hospital CPAs are traditionally always attributed to a cardiac etiology unless a specific cause is clearly identified.11
Although some general results on out-of-hospital CPA in Spain have been published in recent years,12–14 there is no known figure on the true incidence of SCD in Spain. Information is also lacking on the final outcomes of patients who had an out-of-hospital CPA of possible cardiovascular cause.
The aim of this study was to describe the incidence and characteristics of out-of-hospital SCD seen by emergency teams (ETs) and the outcomes at hospital discharge in terms of survival and neurologic outcome.
METHODSA retrospective analysis was conducted of a continuous registry of patients attended by out-of-hospital ETs for CPA between January 2008 and December 2012. The characteristics and methodology of the registry have been described previously.13 Briefly, the Registro Andaluz de Parada Cardiaca Extrahospitalaria (Andalusian Registry of Out-of-hospital Cardiac Arrest) is a prospective, ongoing registry of CPA cases seen by ETs of the Empresa Pública de Emergencias Sanitarias de Andalucía (EPES, Public Health Emergency Company of Andalusia). This public health service handles out-of-hospital health emergencies in Andalusia, with an actual catchment population of 5575128 inhabitants (67.14% of the population, as the total for Andalusia is 8 302 923). Its ETs have an on-board physician.
Inclusion Criteria and MethodsThe registry is included in the EPES general information system. The information system is a real-time record of all calls and responses provided throughout Andalusia. The information system meets the legal requirements for personal data security and protection set forth in the Spanish legislation. The cardiopulmonary arrest registry automatically includes all cases in which the medical history of the encounter includes a diagnosis of CPA or ventricular fibrillation (ICD-9 [International Classification of Diseases, Ninth Revision, Clinical Modification]). These codes are recorded in the information system and are the link for automatic inclusion of the case. Along with the case, a series of variables are automatically recorded in the information system. Other variables are manually entered in the database by accessing the electronic medical records. The variables collected include epidemiology variables, prehospital event and care, hospitalization (use of hypothermia and percutaneous coronary intervention [PCI]), and final outcome, including neurologic outcome. The variables were defined using the Utstein model.11
In-hospital follow-up of patients was performed using the unified electronic medical record of the Servicio Andaluz de Salud. Follow-up at discharge was performed by a standard telephone survey, centralized for all of Andalusia, from an EPES coordination center. The survey asked patients for consent to an interview and to use of their data. Access to the national death certificate center of the Spanish Ministry of Health is requested every year.
Quality AssurancePatients were included according to a design intended to minimize professional intervention and to avoid inclusion and interpretation biases. The database includes internal controls to minimize transcription errors. Every 6 months, the EPES quality system audits a representative sample of medical records to check the diagnosis and degree of completion of key CPA variables.
Statistical AnalysisA descriptive analysis was performed by measures of central tendency and measures of scatter for quantitative variables and by absolute and relative distribution frequency for qualitative variables. A univariate analysis was used to compare the individual effect of each variable on the possibility of arriving with a pulse at the hospital and of good neurologic outcome at hospital discharge, expressed as Cerebral Performance Category grades 1 and 215 (CPC 1-2). The Student t test was used to compare the means, and the chi-square and Fisher tests were used for categorical variables. A multivariable logistic regression analysis was performed using CPC 1-2 at hospital discharge as a dependent variable. Variables with a P value<.1 in the bivariate analysis and less than 5% of losses were included by the forward stepwise method, also including the odds ratio (OR) and the respective 95% confidence intervals (95%CI). Significance was set at P<.05 for the various analyses.
A bivariate analysis was performed to compare patients who arrived at the hospital with patients who died in situ and to compare the group of patients with CPC 1-2 at hospital discharge with the group with poor (CPC 3-4) or unknown neurologic outcome or in-hospital death. Logistic regression was performed using a forward stepwise multivariable analysis, with arrival with a pulse at the hospital taken as the dependent variable. Likewise, forward stepwise multivariable logistic regression was performed for the group of patients who arrived at the hospital, taking CPC 1-2 neurologic outcome at hospital discharge as the dependent variable.
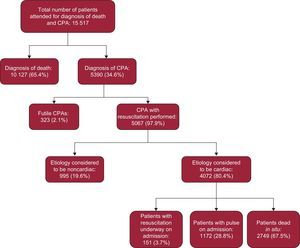
RESULTSDuring the period analyzed, 15 517 patients were attended in a situation of CPA and/or death. In 65.3% of these patients, the ETs only recorded patient death (by diagnosing instantaneous death or unattended death, ICD-9 codes 798.1 and 798.9, respectively). Advanced life support measures were begun in 34.6% of all patients but were stopped in 323 (2.1%) patients because the measures were considered futile. Among 5067 patients who finally received advanced life support, arrest was considered to be of cardiac etiology in 4072 (80.4%) (Figure).
The age range was 0 to 96 years: 199 patients (4.9%) were<35 years old, 14 of them in the first year of life; 2884 (70.8%) were between 35 and 74 years old, and 989 (24.3%) ≥ 75 years old.
Based on the catchment population with EPES land-based ETs, the incidence recorded was 14.6 SCD events per 100 000 inhabitants and year (10.6% men and 4.0% women): 8.0 and 2.7 cases per 100 000 inhabitants and year of men and women between 35 and 74 years, respectively.
Men accounted for 72.6% of these patients, 25% of arrests were treated with initial defibrillable rhythm, and 32.5% of patients arrived at the hospital, although 3.7% arrived while resuscitation measures were still underway, ie, without spontaneous pulse at hospital arrival. In this group, only 1 patient was discharged from the hospital. Among patients with an initial defibrillable rhythm, up to 58.3% arrived at the hospital with a pulse. Among all patients who arrived at the hospital with a pulse, 266 patients (20.1%) required no orotracheal intubation.
In the phase prior to ET arrival, excluding arrests witnessed by health professionals, basic life support measures were performed by witnesses in 20.9% of patients. Automatic defibrillators were used in 75 patients, on 5 occasions by lay witnesses.
Final survival at discharge for the entire series was 11.2% and 10.2% of patients had good neurologic outcome (CPC 1-2). Among these patients with good neurological outcome at discharge, 43.1% were not intubated during prehospital care. The general patient and care characteristics are shown in Table 1.
Descriptive Analysis: General Characteristics of the Population and the Care Received
| Variables | Distribution |
|---|---|
| Patients included, No. | 4072 |
| Age, y | 62.0 ± 15.8 |
| Men | 61.4 ± 14.9 |
| Women | 65.1 ± 17.7 |
| Men/women, % | 72.6/27.4 |
| Reason for call | |
| Unconscious/suspected CPA | 2790 (68.6) |
| Chest pain | 393 (9.6) |
| Dyspnea | 378 (9.3) |
| Syncope | 193 (4.7) |
| Other | 318 (7.8) |
| Place of arrest | |
| Home | 2311 (56.8) |
| Street | 513 (18.6) |
| Public place | 707 (17.4) |
| Out-of-hospital health services | 334 (8.2) |
| OOHEP ambulance | 74 (1.8) |
| Unknown | 133 (3.2) |
| Witnessed arrest | 2980 (73.2) |
| Lay witnesses | 1784 (62.9) |
| Emergency team | 600 (20.1) |
| Other health personnel | 500 (17.8) |
| Unknown | 96 (3.2) |
| Other | 83 (3.7) |
| LS prior to ET | 2043 (50.2) |
| Health personnel | 1307 (64.0) |
| Witnesses | 620 (30.3) |
| Nonhealth public services | 116 (5.7) |
| Defibrillations prior to ET arrival, No. | 303 |
| With SAD, No. | 75 |
| Initial recorded rhythm | 4072 (100) |
| Defibrillable: pulseless VF/VT | 1017 (25) |
| Nondefibrillable | 3055 (75) |
| Asystole | 2526 (82.7) |
| PEA | 300 (9.8) |
| Extreme bradycardia | 162 (5.3) |
| Unknown | 67 (2.2) |
| Collapse-to-ET arrival time recorded | 2791 (80.4) |
| Time, min* | 12 [8-19] |
| Call-to-arrival interval of the ET recorded | 3961 (97.8) |
| Time, min | 12 [8-19] |
| Patients alive on hospital admission | 1172 (28.8) |
| Resuscitation in progress on admission | 151 (3.7) |
| Patients with initial VF rhythm alive on admission | 561 (58.3) |
| Alive at hospital discharge | 472 (11.6) |
| CPC 1 at discharge | 375 (9.2) |
| CPC 2 at discharge | 42 (1) |
| CPC 3 at discharge | 27 (0.7) |
| CPC 4 at discharge | 21 (0.6) |
| Unknown | 7 (0.2) |
CPA, cardiopulmonary arrest; CPC, Cerebral Performance Category; ET, emergency team; LS, life support; OOHEP, out-of-hospital emergency service; PEA, pulseless electrical activity; SAD, semiautomatic defibrillator; VF, ventricular fibrillation; VT, ventricular tachycardia.
Unless otherwise indicated, data are expressed as n (%), mean ± standard deviation, or median [interquartile range].
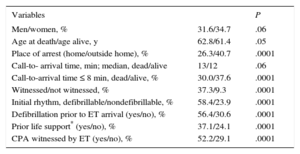
The variables associated with the probability of patients arriving alive at the hospital or arrival with a pulse are listed in Table 2. During hospitalization, 20 patients were treated with hypothermia and 249 patients underwent PCI.
Univariate Analysis: Variables Associated With Patients Arriving Alive at the Hospital (n=4072)
| Variables | P | |
|---|---|---|
| Men/women, % | 31.6/34.7 | .06 |
| Age at death/age alive, y | 62.8/61.4 | .05 |
| Place of arrest (home/outside home), % | 26.3/40.7 | .0001 |
| Call-to- arrival time, min; median, dead/alive | 13/12 | .06 |
| Call-to-arrival time ≤ 8 min, dead/alive, % | 30.0/37.6 | .0001 |
| Witnessed/not witnessed, % | 37.3/9.3 | .0001 |
| Initial rhythm, defibrillable/nondefibrillable, % | 58.4/23.9 | .0001 |
| Defibrillation prior to ET arrival (yes/no), % | 56.4/30.6 | .0001 |
| Prior life support* (yes/no), % | 37.1/24.1 | .0001 |
| CPA witnessed by ET (yes/no), % | 52.2/29.1 | .0001 |
CPA, cardiopulmonary arrest; ET, emergency team.
Statistical significance was set at P<.05.
Good neurologic outcome at hospital discharge in the group of admitted patients was associated with an action interval<8 min, initial defibrillable rhythm, witnessed CPA (particularly witnessed by the ET), and interventions prior to ET arrival, life support, and defibrillation (Table 3).
Univariate Analysis: Variables Associated With Good Neurologic Outcome at Hospital Discharge Among Admitted Patients (n=1245; Cerebral Perfomance Category 1-2, n=417)
| Variables | P | |
|---|---|---|
| Men/women, % | 37.5/23.8 | .0001 |
| Mean age, y, CPC 1-2 (no/yes) | 62.2/60.4 | .08 |
| Site of arrest (home/outside home), % | 26.4/39.8 | .0001 |
| Call-to-arrival interval, min; median, CPC 1-2 (no/yes) | 11.5/12 | .1 |
| Call-to-arrival interval ≤ 8 min, CPC 1-2 (no/yes), % | 34.9/43.4 | .01 |
| Witnessed/not witnessed | 36.5/17.4 | .0001 |
| CPA witnessed by ET (yes/no), % | 48.7/28.7 | .0001 |
| Initial rhythm, defibrillable/nondefibrillable, % | 55.6/16.1 | .0001 |
| Defibrillation prior to ET arrival (yes/no), % | 50.0/31.2 | .0001 |
| Prior life support* (yes/no), % | 38.5/19.5 | .0001 |
| CPA in progress/pulse present on admission, % | 0.7/38.3 | .0001 |
| PCI (yes/no), % | 52.5/6.5 | .0001 |
CPA, cardiopulmonary arrest; CPC, Cerebral Perfomance Category; ET, emergency team; PCI, percutaneous coronary intervention.
Statistical significance was set at P < .05.
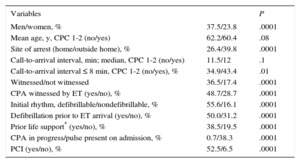
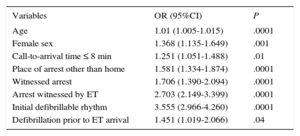
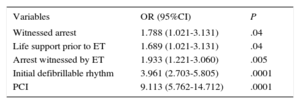
The logistic regression results for variables associated with patients arriving with a pulse at the hospital and hospital discharge with good neurologic outcome (CPC 1-2) (Tables 4 and 5, respectively) yielded the following variables of interest: defibrillable rhythm, witnessed CPA, CPA not occurring at home, and hospital treatment with PCI.
Multivariable Analysis: Variables Associated With Patients Arriving Alive at the Hospital (Pulse Present)
| Variables | OR (95%CI) | P |
|---|---|---|
| Age | 1.01 (1.005-1.015) | .0001 |
| Female sex | 1.368 (1.135-1.649) | .001 |
| Call-to-arrival time ≤ 8 min | 1.251 (1.051-1.488) | .01 |
| Place of arrest other than home | 1.581 (1.334-1.874) | .0001 |
| Witnessed arrest | 1.706 (1.390-2.094) | .0001 |
| Arrest witnessed by ET | 2.703 (2.149-3.399) | .0001 |
| Initial defibrillable rhythm | 3.555 (2.966-4.260) | .0001 |
| Defibrillation prior to ET arrival | 1.451 (1.019-2.066) | .04 |
95%CI: 95% confidence interval; ET, emergency team; OR, odds ratio.
Statistical significance was set at P<.05.
Multivariable Analysis: Variables Associated With Good Neurologic Outcome at Hospital Discharge (n=1245; Cerebral Perfomance Category 1-2, n=417)
| Variables | OR (95%CI) | P |
|---|---|---|
| Witnessed arrest | 1.788 (1.021-3.131) | .04 |
| Life support prior to ET | 1.689 (1.021-3.131) | .04 |
| Arrest witnessed by ET | 1.933 (1.221-3.060) | .005 |
| Initial defibrillable rhythm | 3.961 (2.703-5.805) | .0001 |
| PCI | 9.113 (5.762-14.712) | .0001 |
95%CI%, 95% confidence interval; ET, emergency team; OR, odds ratio; PCI, percutaneous coronary intervention.
Statistical significance was set at P<.05.
We present the results of the largest SCD series analyzed in Spain. The incidence observed in our registry, 14.6 cases per 100 000 inhabitants and year, is well below the figures reported by population registries in Spain,2 particularly when focusing on the age bracket with the highest prevalence of ischemic heart disease (35-74 years). In this age bracket, the population registries report figures of 21 and 5.6 cases, which are somewhat higher than 2-fold our results (8.0 men and 2.7 women per 100 000 inhabitants and year), particularly among men.3 These figures are noteworthy but are not unusual whenever registries of resuscitated arrests are compared with population data on sudden death, as the latter include all patients, even those not receiving health care. This is also a low annual incidence when compared with data from other countries that, although varying widely, have a mean of 35 and 54 cases per 100 000 inhabitants and year in Europe and North America, respectively.6–8 We estimated that 8 out of every 10 CPAs included in our registry were of cardiac cause, a common finding in the main registries similar to ours. This finding is of interest, particularly after the new etiologic classification of the latest recommendations on Utstein-style CPA data collection and reporting, which combines medical causes as a whole.16 This will also make it possible to compare future outcomes and to determine whether they can be carried over to our setting.
In our study, the approximate ratio of men-to-women is 3:1, and SCD affects a rather young population for the mean life expectancy of Spain. In this series, 1 out of every 4 arrests were seen after a telephone call motivated mainly for a reason other than altered consciousness. This should be taken into consideration by the coordination center for out-of-hospital emergency services because some of these situations, such as gasping, are known to be associated with a better prognosis.17
Survival with good neurologic outcome at discharge was 10.2%. A situation of ongoing resuscitation was not advantageous for patients because final survival focused on the group of patients admitted with a spontaneous pulse (almost 30% of all patients). Although noncardiac arrest has a poorer prognosis,18,19 the outcomes are similar to and even better than those reported by other large registries. In addition, global data indicate that survival is 6% in North America, 2% in Asia, 11% in Australia, and 9% in Europe.7 On comparing more recent data with years that coincide with the study period, we found survival rates ranging from 7.8% in Japan,20 9.0% in the United States,21 and 10.4% in Denmark.22
Despite these results, some aspects are very relevant and known to influence the final prognosis, thus warranting reflection.
A fourth of all CPAs were not witnessed, which made it hard to determine the time of the event and to draw conclusions on actual time intervals. Nevertheless, these intervals were longer than desirable both when the time of collapse could be estimated and when the call-to-ET arrival time was analyzed, although they were consistent with the findings published by other out-of-hospital emergency services in Spain.23,24 This is important because care begun within 8 minutes was associated with the probability of hospital admission. The phase prior to ET arrival reveals a critical area for improvement. Only 1 out of every 5 patients received basic life support from witnesses. Automatic defibrillators were also rarely used, a key aspect in our series, as 25% of patients had initial defibrillable rhythms and almost 60% of them arrived at the hospital alive. Despite these figures, both actions were associated with the final prognosis and the probability of patients being admitted alive to the hospital, respectively. It is essential to develop interventions that encourage public involvement in this preliminary phase. These are probably the most important actions to improve overall patient survival.22
More than half the arrests occurred at home, a factor negatively associated with the final prognosis. Arrest at home led to a lower prevalence of initial defibrillable rhythms and had a higher percentage of unwitnessed arrests, in which delays in ET intervention and lower rates of resuscitation by witnesses are a consistent finding in different countries with distinct out-of-hospital emergency service structures.25–27 Patient age and sex are also known prognostic factors,28,29 although in our series sex and age were associated with the probability of live hospital admission, but not with survival or neurologic outcome at discharge.
Along with initial rhythm, witnessing of the arrest by the ET was associated with survival with good neurologic outcome, a finding also reported in the literature.30
The proportion of specific types of care after resuscitation (hypothermia and PCI) was discrete. Because the percentages of application were low, it was to be expected that their statistical influence was not significant, as in the case of hypothermia. However, PCI correlated closely to survival and good final neurologic outcome. Although this is somewhat known,31 its impact on final outcome is nevertheless surprising. Because the role of hypothermia in post-resuscitation treatments is currently controversial,32 this finding is particularly noteworthy. Although possible selection biases of patients who received PCI cannot be excluded, it is an affordable strategy for facilities with primary angioplasty programs. The identification of ST-segment elevation acute myocardial infarction as the cause of the arrest and patient referral to a specific facility if the condition is identified should be part of the care provided by the ET after resuscitation. This debate on the regionalization of health care when attending CPAs is already underway.33
LimitationsThis registry is based on an automatic system for case inclusion. Although it includes mechanisms used for quality assurance, undetected errors in patient coding cannot be ruled out, which would mean that a few patients may not have been included.
The incidence of CPA was calculated based on the number of cases seen by EPES ETs. Although in our case, airborne ETs guarantee the possibility of care throughout the entire community of Andalusia (nearly 9 million inhabitants), land-based ETs cover actual basic health care for CPA. Apart from the debate on health care resources and reality,34,35 we decided to estimate only the population in the catchment area. In terms of etiology, the cardiac cause of out-of-hospital CPA is an estimate. Sudden cardiac arrest is known to be associated with several heart diseases,36 and autopsy reveals that it includes some deaths not strictly considered to be cardiac.3,6,9 However, this is a bias present in all out-of-hospital CPA registries.
The registry included patients prospectively in chronological order but was analyzed retrospectively. Consequently, there are certain variables with a loss of information that would contribute to slight differences in the outcomes. In particular, the loss of information about the time of arrest limits any analysis of the influence of collapse-to-start of resuscitation time.
CONCLUSIONSSudden cardiac death usually occurs at home and affects a relatively young population. Although the rates of survival with good neurologic outcome are comparable to those of similar countries, there are major areas for improvement, particularly in the stage prior to ET arrival. Coronary interventional procedures had a considerable impact on patient recovery.
FUNDINGThe registry is funded by a research grant from the Instituto Carlos III, with cofunding from the FEDER (Fondo Europeo de Desarrollo Regional) funds and the Fundación Progreso y Salud (public research agency of the Consejería de Salud of the Junta de Andalucía).
CONFLICTS OF INTERESTNone declared.