Scarce research has been performed in ambulatory patients with chronic heart failure in the Mediterranean area. Our aim was to describe survival trends in our target population and the impact of prognostic factors.
MethodsWe carried out a population-based retrospective cohort study in Catalonia (north-east Spain) of 5659 ambulatory patients (60% women; mean age 77 [10] years) with incident chronic heart failure. Eligible patients were selected from the electronic patient records of primary care practices from 2005 and were followed-up until 2007.
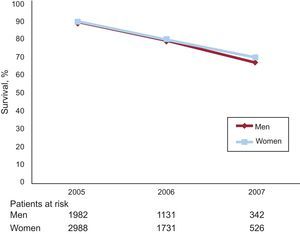
ResultsDuring the follow-up period deaths occurred in 950 patients (16.8%). Survival after the onset of chronic heart failure at 1, 2, and 3 years was 90%, 80%, 69%, respectively. No significant differences in survival were found between men and women (P=.13). Cox proportional hazard modelling confirmed an increased risk of death with older age (hazard ratio=1.06; 95% confidence interval, 1.06-1.07), diabetes mellitus (hazard ratio=1.53; 95% confidence interval, 1.33-1.76), chronic kidney disease (hazard ratio=1.73; 95% confidence interval, 1.45-2.05), and ischemic heart disease (hazard ratio=1.18; 95% confidence interval, 1.02-1.36). Hypertension (hazard ratio=0.73; 95% confidence interval, 0.64-0.84) had a protective effect.
ConclusionsService planning and prevention programs should take into consideration the relatively high survival rates found in our area and the effect of prognostic factors that can help to identify high risk patients.
Keywords
The prevalence of chronic heart failure (CHF) in developed countries is between 1% and 3% and increases with age.1–4 The management of CHF represents an important economic burden for healthcare systems and accounts for 1% to 2% of the total health care expenditure.5,6
CHF is also lethal, particularly after onset,7,8 and worsens after hospital admission.9–11 Other factors such as age, sex and comorbidities have been described to be determinants of prognosis.12 The interaction among these factors is complex13 and complicates management particularly in primary care where diagnosis is often initiated14 and patients are followed-up. However, little research has been performed in ambulatory patients managed in the community.15 Most studies performed to date have been clinical trials or studies that included patients after hospital discharge.7 Moreover, little is known on specific trends and prognostic factors for community CHF cohorts in the Mediterranean area; a lower incidence16 and lower risk of fatal coronary heart disease have been described17,18 even though cardiovascular risk factors are similar to those found in the rest of Europe.19 In Spain, trends in survival are mainly reported by the national data registry from hospital-based heart failure clinics20 and large community population-based studies representing the Mediterranean lifestyle are lacking.
The aim of this study was to document longitudinal survival trends in ambulatory patients with CHF in Catalonia (north-east Spain) and to assess the impact of comorbidity and hospitalization on survival.
METHODSStudy Design and SettingWe designed a population-based retrospective cohort study using the resources of a project published in clinical trials database (NCT00792402), which evaluated the impact of a computerized clinical guideline on CHF in Catalonia (population of 7 210 50821). Briefly, in this project, a pragmatic, nonequivalent, controlled, before-and-after quasi-experimental study was performed using a population-based approach. Patients from 2 regions (urban and rural) were included. This project was established to evaluate a complex intervention in the urban setting where primary care practices (PCPs) were randomized. Half the PCPs followed usual care management plus a computerized clinical guideline on CHF and half underwent a disease management intervention.
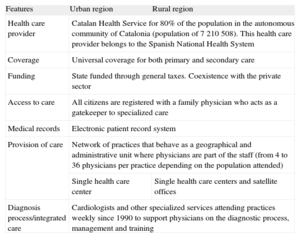
For the purpose of this study, data from both regions were combined. Despite urbanization differences, both regions shared the same organisational features22 (Table 1). Ethical approval for this study was obtained from the Health Care Ethics Committee of the Institut d’Investigació en Atenció Primària Jordi Gol.
Organizational Features of Participating Primary Care Practices
| Features | Urban region | Rural region |
| Health care provider | Catalan Health Service for 80% of the population in the autonomous community of Catalonia (population of 7 210 508). This health care provider belongs to the Spanish National Health System | |
| Coverage | Universal coverage for both primary and secondary care | |
| Funding | State funded through general taxes. Coexistence with the private sector | |
| Access to care | All citizens are registered with a family physician who acts as a gatekeeper to specialized care | |
| Medical records | Electronic patient record system | |
| Provision of care | Network of practices that behave as a geographical and administrative unit where physicians are part of the staff (from 4 to 36 physicians per practice depending on the population attended) | |
| Single health care center | Single health care centers and satellite offices | |
| Diagnosis process/integrated care | Cardiologists and other specialized services attending practices weekly since 1990 to support physicians on the diagnostic process, management and training | |
We included incident patients attending PCPs from 2005 to 2007. Patients aged more than 30 years old with a diagnostic code related to CHF, registered by their primary care physician (I11.0, I13.0, I13.2, I50, I50.0, I50.1, I50.9, P29.0, according to the International Classification of Diseases Tenth Revision used in primary care) were included. As a measure of diagnostic accuracy we only included patients prescribed diuretics. In the urban region, we included the randomized set of PCPs that followed usual care plus clinical practice guideline on CHF and excluded those PCPs that underwent the disease management intervention. We included all PCPs in the rural region.
MeasuresWe measured survival after the onset of CHF until death or the end of follow-up (December 31st, 2007). Onset of CHF referred to the recorded date of diagnosis of CHF, which we extracted from the primary care electronic patient records. Registration of the diagnosis was done by primary care physicians and in our context is usually done after cardiologist consultation or advice (Table 1) or after the patient has been admitted to hospital. As a measure of the accuracy of the diagnosis, we only included patients prescribed diuretics. We also measured survival in patients with hospital admission for cardiovascular causes during the follow-up, as a primary discharge diagnosis (398-398.99, 402-402.91, 428-428.9, 997.1, 403.90-403.91, 404-404.93, 411-411.89, 414-414.9 according to the International Classification of Diseases Ninth Revision used by hospitals). We included mortality from any cause.
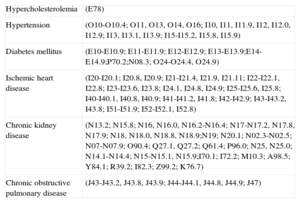
Potential comorbidities associated with survival were defined on the basis of the International Classification of Diseases Tenth Revision codes registered in the primary care electronic patient records either before or at the onset of CHF and were chosen according to a review of the literature, clinical relevance, and availability. We included patient age and sex, hypercholesterolemia, hypertension, diabetes mellitus, ischemic heart disease, chronic obstructive pulmonary disease, and chronic kidney disease (Table 2). We obtained age by calculating the difference between the date of inclusion in our study (January 1st 2005) and date of birth and considered 2 categories: patients aged less than 65 years and patients aged 65 years or older. Setting was also considered as a covariate.
International Classification of Diseases Tenth Revision Codes Related to CoMorbidity Included in This Study
| Hypercholesterolemia | (E78) |
| Hypertension | (O10-O10.4; O11, O13, O14, O16; I10, I11, I11.9, I12, I12.0, I12.9; I13, I13.1, I13.9; I15-I15.2, I15.8, I15.9) |
| Diabetes mellitus | (E10-E10.9; E11-E11.9; E12-E12.9; E13-E13.9;E14-E14.9;P70.2;N08.3; O24-O24.4, O24.9) |
| Ischemic heart disease | (I20-I20.1; I20.8, I20.9; I21-I21.4, I21.9, I21.11; I22-I22.1, I22.8; I23-I23.6, I23.8; I24.1, I24.8, I24.9; I25-I25.6, I25.8; I40-I40.1, I40.8, I40.9; I41-I41.2, I41.8; I42-I42.9; I43-I43.2, I43.8; I51-I51.9; I52-I52.1, I52.8) |
| Chronic kidney disease | (N13.2; N15.8; N16, N16.0, N16.2-N16.4; N17-N17.2, N17.8, N17.9; N18, N18.0, N18.8, N18.9;N19; N20.1; N02.3-N02.5; N07-N07.9; O90.4; Q27.1, Q27.2; Q61.4; P96.0; N25, N25.0; N14.1-N14.4; N15-N15.1, N15.9;I70.1; I72.2; M10.3; A98.5; Y84.1; R39.2; I82.3; Z99.2; K76.7) |
| Chronic obstructive pulmonary disease | (J43-J43.2, J43.8, J43.9; J44-J44.1, J44.8, J44.9; J47) |
From January 2005 to December 2007, we extracted data from 3 national database sources, which we were able to match because every Catalan citizen has a unique and anonymous identification number for health care use. The central database of the Catalan Health Service facilitated data abstraction from the electronic patient records of PCPs. Data from hospital admissions was gathered from the Division of Demand and Activity Registries (Minimum Basic Data Set for Acute-care Hospitals) of the Catalan Health Service, where all Catalan hospitals are required to send in their data for reimbursement. Information on mortality was gathered from the Mortality Register of Catalonia, where fatalities had to be notified. We recorded as fatality cases patients codified as such in the primary care electronic patient records register and those also identified in the Mortality Register of Catalonia.
None of the officers responsible for data abstraction were involved in the subsequent data analysis.
Statistical MethodsDescriptive data from our sample on age, sex and comorbidities are presented. We calculated the entire cohort follow-up period and reported the median, minimum and maximum values. Candidate variables significantly associated with mortality in the bivariate analysis (P<.05) were included as potential covariates in the multivariable model. In the bivariate model, the chi square text and Fisher's exact test were used for categorical variables and Student's t test for continuous variables. Kaplan Meier analysis was used to determine long-term survival. The Cox proportional hazards model was used to examine the independent effect of candidate variables. The forward and backward step technique with the likelihood ratio test was used. Discrimination of the model was calculated with Harrell's C-index, and calibration of the model was calculated with the Gronnesby and Borgan test. Constant hazard was tested with the log (−log S[x]) vs Log(time) graphic. All tests were 2-tailed and significance was set at the 5% level (α=0.05). Missing values were calculated (0.2% of our final sample) and were found not relevant in our analysis.
The statistical analysis was performed with SPSS v18 software and StataCorp12.
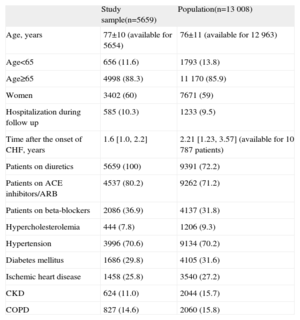
RESULTSInitially we identified 13 008 potentially eligible patients with a diagnosis of CHF from 43 PCPs, covering a population of 1 039 342 listed citizens.
We excluded 2221 patients without registration of the date of diagnosis and 5128 patients with a prevalent diagnosis of CHF or without a prescription for diuretics. Our final sample consisted of 5659 patients from 43 PCPs: 3641 (64.3%) from urban areas (covering a population of 558 515 inhabitants) and 2018 (35.7%) from rural settings (covering a population of 480 827 inhabitants). The median follow-up period of the entire cohort was 3 years with a minimum of 0.08 years and a maximum of 3 years.
Patient characteristic in the sample did not differ substantially from those of the initial population (Table 3). The mean (standard deviation) age of our sample was 77 (10) years; 88.3% of the patients were aged 65 years or more and 60% were women. During the study period, 585 patients (10.3%) were hospitalized for cardiovascular causes. The median interval after the onset of CHF was 1.6 years. Regarding comorbidities, the bivariate analysis showed that in those patients who died during the follow-up, hypertension was more prevalent in women (P=.022) and in patients aged 65 years or more (P=.029), while chronic obstructive pulmonary disease (P<.001), ischemic heart disease (P<.001), and chronic kidney disease (P=.009) were more common in men. Diabetes mellitus was more frequent in patients aged less than 65 years (P=.041), while hypercholesterolemia was also more frequent, although this difference was not statistically significant (P=.771).
Patient Characteristics
| Study sample(n=5659) | Population(n=13 008) | |
| Age, years | 77±10 (available for 5654) | 76±11 (available for 12 963) |
| Age<65 | 656 (11.6) | 1793 (13.8) |
| Age≥65 | 4998 (88.3) | 11 170 (85.9) |
| Women | 3402 (60) | 7671 (59) |
| Hospitalization during follow up | 585 (10.3) | 1233 (9.5) |
| Time after the onset of CHF, years | 1.6 [1.0, 2.2] | 2.21 [1.23, 3.57] (available for 10 787 patients) |
| Patients on diuretics | 5659 (100) | 9391 (72.2) |
| Patients on ACE inhibitors/ARB | 4537 (80.2) | 9262 (71.2) |
| Patients on beta-blockers | 2086 (36.9) | 4137 (31.8) |
| Hypercholesterolemia | 444 (7.8) | 1206 (9.3) |
| Hypertension | 3996 (70.6) | 9134 (70.2) |
| Diabetes mellitus | 1686 (29.8) | 4105 (31.6) |
| Ischemic heart disease | 1458 (25.8) | 3540 (27.2) |
| CKD | 624 (11.0) | 2044 (15.7) |
| COPD | 827 (14.6) | 2060 (15.8) |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; CHF, chronic heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease.
Data are expressed as no. (%), mean±standard deviation or median [interquartile range].
During the follow-up period, 950 patients died (16.8%).
Survival after the first, second and third year of follow-up was 90%, 80%, 69%, respectively (Figure); no significant differences (P=.13) in survival were found between men and women.
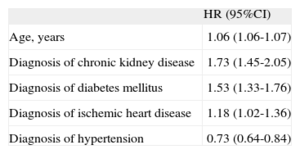
Cox proportional hazard modelling (Table 4) confirmed an increased risk of death for older age (hazard ratio [HR]=1.06; 95% confidence interval [95%CI], 1.06-1.07), diabetes mellitus (HR=1.53; 95%CI, 1.33-1.76), chronic kidney disease (HR=1.73; 95%CI, 1.45-2.05), and ischemic heart disease (HR=1.18; 95%CI, 1.02-1.36). Hypertension (HR=0.73; 95%CI, 0.64-0.84) had a protective effect. We did not find a significant effect according to the setting.
Multivariable Model Reporting the Effect of Prognostic Factors on Survival (N=5647). Cox Proportional Hazards Model
| HR (95%CI) | |
| Age, years | 1.06 (1.06-1.07) |
| Diagnosis of chronic kidney disease | 1.73 (1.45-2.05) |
| Diagnosis of diabetes mellitus | 1.53 (1.33-1.76) |
| Diagnosis of ischemic heart disease | 1.18 (1.02-1.36) |
| Diagnosis of hypertension | 0.73 (0.64-0.84) |
95%CI, 95% confidence interval; HR, hazard ratio.
The assumption of constant hazard was met. The discrimination of the model was 0.67.
Calibration of the model (P=.03) was significant for the first decile only and was not significant for the remaining deciles, indicating that the model failed in patients with lower risk.
DISCUSSIONIn our study 90% of ambulatory patients with CHF survived 1 year after onset. Independent predictors of a worse outcome were older age, diabetes mellitus, chronic kidney disease, and ischemic heart disease. In contrast with previous studies carried out in hospital-based cohorts or selected patients from clinical trials, we evaluated mortality trends and predictors of mortality for ambulatory patients in a Mediterranean community-based cohort.
Comparisons with other studies are hampered by differences in patient selection, patient characteristics, and follow-up periods. Nevertheless, our survival rates were higher than those reported in the literature, such as the Framingham8 (57% for men and 64% for women) and Rochester23 (77%) studies in the United States, and the Hillingdon7 (62%) study in the United Kingdom. All of these studies reported incident CHF. In our study, survival was also higher than that in a study in the Netherlands24 (74% survival at 1 year), which used a selection process similar to ours. In prevalent CHF, studies in central Europe reported a 1-year survival rate of 87.4%25 and 89%.26
On the other hand, our survival rates for incident CHF were in line with those reported by the Spanish national data registry from hospital-based heart failure clinics20 (survival rates at 1 and 2 years of 90% and 80%, respectively). Higher mortality (about 30% mortality at 1 year) was found in the south of Spain,27 although this phenomenon has been described as a paradox,28 as this mortality is the highest in Spain and is associated with ischemic heart disease mortality, illiteracy, and unemployment.29 In contrast, we found a low rate of hypercholesterolemia and ischemic heart disease in our cohort, which could partly explain our positive results on survival. None of the above studies analyzed the effect of comorbidities on outcomes.
Our results show that Mediterranean countries may also have better outcomes for CHF in addition to the favorable trends reported in coronary heart disease.17,18 It has been hypothesized that regional factors,30 as well as the implementation of evidence-based therapies and risk factor management,19 may confer protection. At the organizational level, there may be differences in the role played by primary care in health care systems on risk factor control and in fast tracking to specialist care. To allow comparisons, these issues should be further investigated in epidemiological studies in other Mediterranean countries.
Despite differences in patient selection and patient characteristics, the predictors of worse prognosis in our study were similar to those found in previous community-based studies. There is common agreement on the effect of older age both in the United States and Europe, although disparities exist regarding sex and other prognostic factors. Although we found no effect of sex on survival, several studies have reported better survival in women.8,24,25 Other factors that increase the risk of death are diabetes mellitus,8,26,31 hospitalization25 and renal failure.7,23,25,26.
Hypertension has been previously reported23 as a positive predictor for survival. In a multivariable analysis, we found better survival among patients with a diagnosis of hypertension registered in their electronic medical records. The higher survival was probably due to the negative effect of low systolic blood pressure on prognosis described elsewhere7,25,26 rather than to the diagnosis of hypertension itself, which is one of the causes of diastolic heart failure and is more prevalent in women and older patients, who usually have a longstanding history of hypertension.24,32,33
LimitationsOur study has some potential design limitations concerning the inclusion of participants and measures. Although we did not have access to the set of PCPs excluded in the urban region, we found no significant differences among the regions included in this study. We expected that any other ethnic or socioeconomic effect on outcomes would have been minimized by our selection process, which developed from a previous randomization performed for a concomitant disease management intervention.
We identified CHF patients through their primary care physician's electronic patient records but did not know how many of them had undergone echocardiography and therefore lacked information on the etiology of CHF, which would have aided interpretation of our results. As a measure of diagnostic accuracy, we only selected patients who had been prescribed diuretics to perform our data analysis and possibly missed patients with CHF not receiving diuretics.
Usually, in our setting, primary care physicians register the diagnosis of CHF after confirmation by a specialist. This specialist is also involved in the diagnostic process and management of these patients in the community and provides support to primary care physicians in their setting, as this has been part of our integrated care program since 199034 (Table 1). Although we could not exclude the possibility that diagnosis of CHF was made clinically by the primary care physician alone in some cases, our results on survival were consistent with those found in the Spanish national data registry.
Our predictive model had a modest predictive power (c=0.67) and also low goodness-of-fit (P=.03), particularly for the first decile, with higher goodness-of-fit for the remaining deciles, indicating that the model failed in patients at lower risk. These results could be explained by 2 reasons: a) comorbidities were identified through the primary care physicians’ registration in electronic patient records and we were unable to capture how long patients had been exposed to the conditions or to obtain information on severity by using biomarkers, and b) the sample size was large (over 500 cases in each decile), increasing the possibility that every small difference would be significant. Nonetheless, our model was clinically relevant and in line with reports in the literature.
Because of the low registration on New York Heart Association classification and left ventricular ejection fraction, we could not present survival data according to these factors. Such information would have provided more detailed information on the severity of CHF. Primary care physicians do not usually record this information, nor do they do so as open access text, which also hampered access.
Finally, we considered the date of registration of CHF in the primary care physicians’ electronic medical records, which did not necessary reflect the date when the diagnosis was made, although our survival rates matched those in national database registers.
CONCLUSIONSSurvival rates in our community cohort of patients with CHF were relatively high. Clinicians and managers need to consider this favorable prognosis in service planning, as well as the effect of prognostic factors, which could help to identify high-risk patients.
FUNDINGThis study was supported by Instituto de Salud Carlos III, Spanish Ministry of Health (grant number PI07/91020).
CONFLICTS OF INTERESTNone declared.
We gratefully acknowledge the researchers of the CHF Project: Concepció Morera, Valeria Pacheco, Joan Cabratosa, Núria Fabrellas, Júlia Roura, Margarita Puigvert, Josep Paredes, Carola Orrego, Joaquim Bañeres, and Carles Benet. We also thank Miguel Angel Muñoz, Xavier Bonfill, and Rosa Suñol for comments on a previous manuscript, and the Institut d’Investigació en Atenció Primària Jordi Gol. and Boni Bolibar for administering funding and providing research advice. We thank the directors and informatics officers of the national databases for providing the relevant information and particularly Josep M. Picas, Delfí Faixedas, and Maria Luisa Bernard-Antoranz. We are also grateful to the Catalan Division of Demand and Activity Registries and the Mortality Register of Catalonia for reporting data on hospitalizations and mortality respectively, and to Núria Mora for her advice on the statistical analysis.