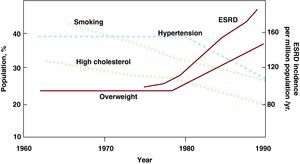
The metabolic syndrome (MetS) is a cluster of risk factors for atherosclerotic cardiovascular (CV) and renal disease that are linked to overweight, obesity, and a lack of physical activity,1 and include central (intra-abdominal) obesity, insulin resistance, impaired glucose tolerance, atherogenic dyslipidemia, hypertension, and proinflammatory states.2 Criteria for diagnosis of the MetS as established by the United States National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III)2 are listed in Table 1. The MetS doubles the risk for CV disease, more than triples the risk for CV mortality,3 and raises the risk for type 2 diabetes by about 5-fold. Obesity plays a particularly central role in the pathomechanisms of MetS and raises the risk for chronic kidney disease (CKD) by about 4-fold. The 2 chief risk factors for end-stage renal disease, hypertension and type 2 diabetes, are both linked to MetS and obesity. Moreover, a rise in the incidence of end-stage renal disease that was observed despite a decline in the prevalence of some CV risk factors has closely paralleled the increasing prevalence of obesity (Figure 1).4
Table 1. Criteria for Diagnosis of Metabolic Syndrome According to the US National Cholesterol Education Program Adult Treatment Panel III.
| Risk factor | Defining level |
| Abdominal obesity | Waist circumference: men, >102cm (>40 in); women, >88cm (>35 in) |
| Triglycerides | >150 mg/dL (1.69 mmol/L) |
| HDL cholesterol | Men<40 mg/dL (1.04 mmol/L); women<50 mg/dL (1.29 mmol/L) |
| Blood pressure | >130/85mmHg |
| Fasting glucose | >110 mg/dL (6.1 mmol/L). |
HDL, high-density lipoprotein.
Diagnosis of the metabolic syndrome requires the presence of at least 3 of the listed criteria.
Source: Ford et al. 2
Figure 1. Estimated prevalence of cardiovascular risk factors as assessed by the National Health and Nutrition Examination Surveys I, II, and III and incidence of end stage renal disease as reported by the United States Renal Data Systems Surveys. A rise in the incidence of end-stage renal disease paralleled the increasing prevalence of obesity. ESRD, end-stage renal disease. From Hall et al, 4 with permission.
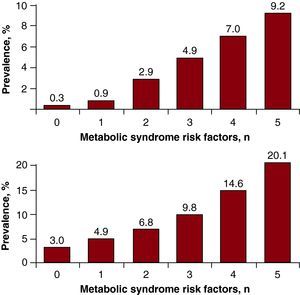
The prevalence of MetS is increasing to epidemic proportions not only in the United States and urbanized world, but also in developing nations.5 It affects ∼25% of adults in the United States6 and 20%-30% of the adult population in most countries,7 and continues to rise with increasing affluence, obesity, lack of physical activity, and aging of the population, and bears a significant healthcare cost. Individual employees with MetS double the healthcare costs of those without any risk factors.6 While each risk factor in this constellation could alone increase CKD, studies have shown that the MetS components act synergistically.8 The MetS is also an important predictor of early renal dysfunction and the odds ratios (OR) of CKD and microalbuminuria increase with the number of MetS components9, 10 (Figure 2). Nevertheless, the mechanism of its momentous effects on the kidney remains to be elucidated.
Figure 2. Prevalence of chronic kidney disease (top) and microalbuminuria (bottom) by number of the metabolic syndrome components. From Chen et al, 10 with permission.
Prospective data have demonstrated the impact of MetS on evolution of CKD, and highlighted the importance of targeting MetS for prevention of renal disease and premature death.8 Clinical studies agree that by the time overt signs of kidney involvement – proteinuria and reduced glomerular filtration rate – are found, structural damage has already been established, and it is thus critical to detect the earliest changes to better understand the underlying pathophysiological state and devise targeted interventions.11 Early detection, monitoring, and modulation of the effects of MetS on target organs present a major challenge for healthcare professionals facing an epidemic of overweight and sedentary lifestyle. It is being recognized that aggressively addressing multiple-risk populations would produce significant reductions in the incidence and prevalence of morbidity and mortality, and that treatment decisions should be based on the presence of multiple risk factors, such as the constellation of MetS. This mandates greater understanding of the harmful effects of MetS on target organs, and design of individualized diagnostic and treatment strategies.
According to the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) clinical practice guidelines,12 CKD can be categorized into 5 levels of severity, mainly using estimated glomerular filtration rate (eGFR) to define the different stages of kidney disease (Table 2). Based on this NKF KDOQI classification, a little over 10 million adults in the United States have stage 1 or stage 2 CKD, which exhibit eGFR within normal limits but are accompanied by other evidence of kidney injury. An alternative system has been recently proposed, using eGFR and proteinuria measures to categorize the risk for clinically relevant loss of kidney function or death in patients with CKD.13 Chronic kidney disease increases CV morbidity and mortality and constitutes a risk factor for adverse outcomes in other acute and chronic diseases. Compelling evidence indicates that CKD can be detected early through screening programs, which could permit early intervention to reduce the risks of CV events, kidney failure, and death that are associated with CKD.14
Table 2. Current National Kidney Foundation Kidney Disease Outcomes Quality Initiative Staging System Risk for Chronic Kidney Disease.
| Stage | eGFR (mL/min/1.73 m2) |
| 1 | ≥90 |
| 2 | ≥60<90 |
| 3 | ≥30<60 |
| 4 | ≥15<30 |
| 5 | <15 |
eGFR: estimated glomerular filtration rate (mL/min per body surface area).
The decreases in eGFR in the different stages of chronic kidney disease need to be accompanied by the presence of proteinuria and/or other evidence of kidney damage.
Source: National Kidney Foundation. 12
In the article published in Revista Española de Cardiología, Landecho et al.15 tested the hypothesis that MetS and its traits were associated with the early stages of CKD, and that they have a synergistic effect on the development of arteriosclerosis, represented by carotid intima-media thickness (IMT). They studied 1498 subjects recruited from 2163 consecutive subjects that underwent a general medical examination over a period of 10years. Insulin resistance was defined on the basis of the Homeostasis Model Assessment (HOMA) index. The carotid IMT measurements were made in 1000 of the 1498 subjects using Doppler ultrasound and a cut-off point for abnormal carotid IMT set at 0.75mm.
The authors found an age-dependent increase in prevalence of early kidney disease (EKD), with an overall 8.9% prevalence of early CKD among the 1498 subjects.15 This rate is higher than estimates in previous studies performed in Spain (around 2.2% according to the Spanish study Epidemiología de la Insuficiencia Renal Crónica en España) or in the United States.14 This finding has no clear explanation other than sampling error. Nevertheless, the prevalence of EKD increased progressively with the number of traits of MetS, from 2.9% of the subjects with no MetS traits to 20% in subjects diagnosed with MetS, and reached 26.3% specifically in elderly subjects with MetS. Both MetS and EKD were associated with an increase in carotid IMT, probably because atherosclerosis, MetS, and CKD can be driven by similar cardiovascular risk factors like hypertension, insulin resistance, obesity, dyslipidemia, and inflammation. The prevalence of EKD was higher in subjects with MetS in all age groups, as previously suggested by analysis of data obtained from 7832 participants in the third National Health and Nutrition Examination Survey (NHANES III).10
Each trait of MetS was associated with a high OR of EKD, interestingly with the exception of low high-density lipoprotein (HDL). While low HDL is an important component of the abnormal lipid profile found in CKD patients, the early stage of EKD may theoretically be associated with more subtle functional changes in HDL, such as its capacity to accept cholesterol from macrophages, or cholesterol efflux capacity.16 Importantly, while obesity is a recognized risk factor for CKD, this study shows that it doubles the risk of an earlier stage of kidney disease. The authors concluded that MetS is an important risk marker for EKD and that their coexistence in patients significantly increases the risk of atherosclerosis as determined by carotid IMT. The current study indeed underscores the importance of the crosstalk between the kidney, the cardiovascular system, and mechanisms of early atherosclerosis.
As the authors indicated,15 the study was associated with several limitations. The definition of EKD was based on a single measurement of albumin/creatinine ratio, which may vary and might be influenced by other factors. In addition, while the carotid IMT is an accepted marker of structural changes related to early atherosclerosis, it might not reflect the early functional alterations consequent to the disease. Moreover, the observed changes in albumin/creatinine ratio may in fact reflect early dysfunction rather than structural changes in the kidney, and might thus better correlate to the early functional changes of atherosclerosis observed in patients with MetS and obesity, such as the degree of endothelial function.
The current paper may also support the notion that the early changes in kidney function associated with MetS do not only result from MetS but might also contribute to its mechanism, similar to the role that insulin resistance plays in the pathogenesis of this syndrome. This observation may have important clinical implications because they suggest that development of laboratory findings consistent with EKD in patients with MetS may reflect the systemic nature of MetS and serve as a marker for the progression of the syndrome. Future studies should be directed to elucidate the potential role of using this marker for prognosis and assessment of successful therapy, and to develop preventive and interventional tactics to decrease the prevalence and association of both EKD and MetS.
FundingPartly supported by grant numbers HL085307, DK77013, HL77131, DK73608, HL92954, and AG 31750 from the National Institutes of Health of the United States.
Conflicts of interestNone declared.
Corresponding author: Division of Nephrology and Hypertension, Mayo Clinic, 200 First Street SW, Rochester, MN 55905 United States. lerman.lilach@mayo.edu